Abstract
BACKGROUND AND PURPOSE: Hydroxyapatite ceramic microparticles are newly developed embolic materials. The purpose of this study was to evaluate the characteristics, embolic properties of hydroxyapatite ceramic microparticles, and effects of transcatheter embolization from an angiographic standpoint and to histopathologically evaluate the results of animal experimentation.
METHODS: After physical evaluation of the characteristics and embolic properties of hydroxyapatite microparticles (100–250 μm in diameter), microcatheter superselective renal artery embolization was performed in rabbits by using this material. Follow-up angiography and histopathologic study of 18 rabbits were performed at different intervals within 24 weeks after embolization.
RESULTS: No microcatheter clogging was observed because of excellent visibility of this material in the suspension and because of its excellent navigability due to its nearly oval shape with no “spines.” Angiographic renal arterial devascularization was consistently obtained without unexpected proximal occlusions; follow-up angiography showed persistent occlusion. Histopathologic evaluation confirmed satisfactory embolization of peripheral arteries. Chronic inflammatory cells were observed in several vessels containing hydroxyapatite microparticles. No evidence of angionecrosis, hemorrhage, or extraluminal migration was noted in any sections.
CONCLUSION: Hydroxyapatite microparticles are excellent biocompatible embolic materials with good visibility during injection control, capable of producing effective occlusion of the distal arteriocapillary bed.
Among embolic materials for hypervascular tumors, particles are preferred to liquid, if used in appropriate size, because of ease of handling and safety. Various solid embolic agents have been developed, including Gelfoam (1), microfibrillar collagen (2), collagen microbeads (3), dextran (4), polyvinyl alcohol particles (5), and trisacryl gelatin (6). Several types of particulate embolic materials are currently available, but they are not necessarily satisfactory for clinical use, because of their reported complications (3, 7–18) and because of the frequent incidence of microcatheter clogging due to their irregular shape and poor particle visibility in the contrast medium suspension. A few newer embolic agents have improved their poor visibility by the use of coloring and do not have the disadvantage of spines. Hydroxyapatite (Ca10[PO4]6(OH)2) is a form of calcium phosphate with a microporous structure. Synthetic hydroxyapatite is a ceramic that is stable and biocompatible (19); it has been widely applied clinically in prosthetic grafts in orthopaedic surgery, plastic and reconstructive surgery, spinal surgery, cranial reconstruction, and oral surgery. To our knowledge, the properties and characteristics of hydroxyapatite as an embolic agent have never been investigated.
Methods
Medical grade nanocrystalline stoichiometric (Ca/P = 1.67) hydroxyapatite suspension was synthesized through wet reaction by adding phosphoric acid into calcium hydroxide suspension. The suspension was dried into the spherical powder (15 μm in diameter) by using a spray drying technique. The powder was calcined at 700°C and jet-milled for conditioning. The conditioned powder was again mixed with water and dried in a mold to obtain a porous block (50% porosity). The porous block was crushed into small microspheres by a granulator machine. The particle size of microspheres was precisely calibrated to be 100 to 250 μm in diameter by screen mesh, and finally, the microsphere was sintered at 800°C. The microsphere was pure hydroxyapatite according to chemical analysis, including X-ray powder diffraction. Sterilization was obtained by using ethylene oxide gas during 24 hr before use. The suspension of hydroxyapatite in contrast media was made in various concentrations, and we used hydroxyapatite suspension with 10 mg of hydroxyapatite particles for 10 mL of 80% contrast media. One-milliliter syringes were mainly used. Visibility, sedimentation rate, and incidence of aggregation were visually examined and compared with those of polyvinyl alcohol particles of the same size (100–250 μm in diameter) and concentration. Controllability of injection through a 2.7-French microcatheter and frequency of clogging phenomenon were also studied. The renal arteries of rabbits, all of which were fed a standard laboratory diet, were chosen for evaluating this embolic material. Eighteen rabbits weighing 2.5 to 4.0 kg were anesthetized with intramuscular administration of ketamine (50 mg/kg) and atropine sulfate (1 mg/kg). They were transbronchially intubated, and no rabbits needed mechanical ventilation. After surgical exposure of the femoral artery, a 2.7-French microcatheter (Target Therapeutics, Japan) was advanced into the renal artery by using a microguidewire under fluoroscopic guidance. Selective angiography of the renal artery was performed before embolization. Hydroxyapatite microparticles were mixed with contrast medium at a concentration of 320 mgI/mL (Hexabrix 320; Tokyo Tanabe Co. Ltd., Tokyo, Japan) and slowly injected by using 1.0-mL graded syringes until flow stagnation was observed under fluoroscopy. After embolization, superselective angiography was again performed. The punctured femoral artery was compressed manually for hemostasis, and the skin was closed. The rabbits were divided into six groups of three rabbits each according to interval after embolization: immediately after embolization and 1 day, 1 week, 3 weeks, 12 weeks, and 24 weeks after embolization. Follow-up angiography was performed in the latter five groups. All the animals were killed by using a standard method (overdose of anesthetic agents). Both kidneys (one side, embolized; contralateral, control) with surrounding tissues and vessels were removed at autopsy after perfusion fixation with 10% formaldehyde solution under approximately 100 cm H2O pressure through the catheter in the thoracic aorta. After paraffin embedding, the kidneys were sectioned and examined under the light microscope with hematoxylin and eosin staining.
Results
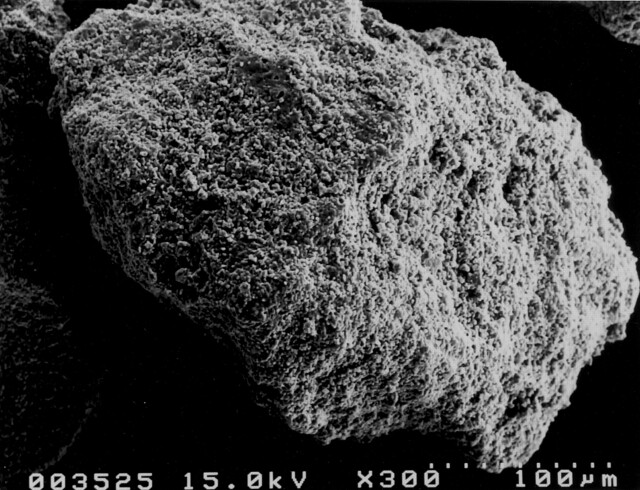
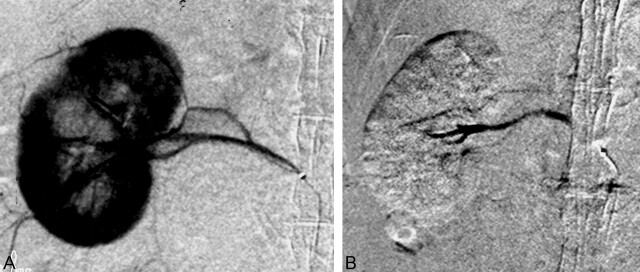
Scanning electron micrographs show that hydroxyapatite particles have a nearly oval shape with no spines and a microporous structure (Fig 1). The visibility of particles in the contrast medium suspension is significantly superior to that of polyvinyl alcohol particles of the same diameter and concentration (Fig. 2). The diffusion of hydroxyapatite particles in the suspension was also good because of its slow sedimentation rate in the contrast media. Injection through a microcatheter was always easy, and no microcatheter clogging was experienced because of the easy visibility of particles in the suspension. We could easily control the injection rate under good visual monitoring so that we were able to avoid particles cluster at the microcatheter hub and injection syringe. All the rabbits except three well tolerated the anesthetic and endovascular procedures. Of the three rabbits, two had infection of the femoral wound and one had circulatory and respiratory system dysfunction after additional administration of anesthetic agents. The endovascular procedure was successfully performed in all animals. Angiography showed all embolized renal arteries to be occluded after gradual blood flow reduction with 10 to 30 mg of the particles (Fig 3A and B); follow-up angiography showed persistence of occlusion in all the rabbits during a period of 1 day to 24 weeks (Fig 4). Macroscopic findings of embolized kidney were as follows: renal arteries were thrombosed, and kidneys were decreased in size in proportion to the interval between embolization and resection. On histologic sections, hydroxyapatite microparticles appeared slightly basophilic. No material fragmentation was observed on any of the sections examined. The microparticles reached the peripheral renal medullary arteries within 100 to 250 μm in diameter (Fig. 5A). No arterial wall necrosis or hemorrhagic changes around the occluded vessels were found in any of the sections studied. A few small round cells and multinuclear cells were observed in the thrombus or organized tissues among the embolic materials. All sections, prepared in every interval ≤24 weeks after embolization, showed complete vascular occlusion with no recanalization and no extraluminal migration, and hydroxyapatite microparticles were still found with no resorption. Histologic findings in larger arteries with a diameter of approximately 400 μm were nearly the same as those in smaller vessels (Fig 5B).
Fig 1.
Scanning electron microscopic image shows the oval shape of hydroxyapatite ceramic microparticles. Surface has microporous structure with no spine (original magnification, ×300).
Fig 2.
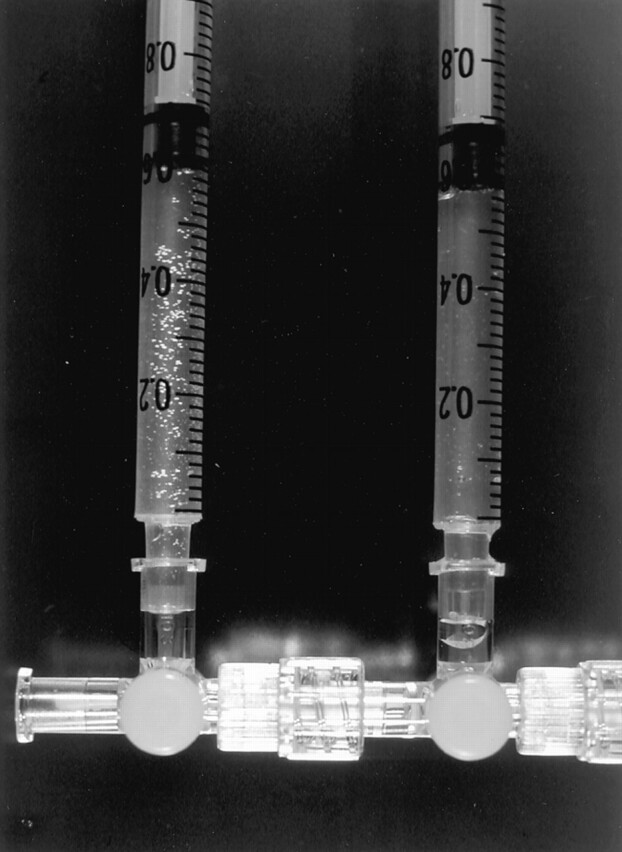
Visibility of the suspension of hydroxyapatite ceramic microparticles in 80% contrast media (left) is comparatively superior to that of polyvinyl alcohol particles of the same size (right) contained in the 1.0-mL graded syringes.
Fig 3.
Selective right renal arterial angiogram of a rabbit.
A, Before embolization.
B, Immediately after embolization with hydroxyapatite microparticles. The renal artery is occluded with hydroxyapatite microparticles after embolization.
Fig 4.
Twenty-four weeks after embolization, persistent occlusion of the embolized right renal artery can be seen. The right kidney seems to have atrophic change.
Fig 5.
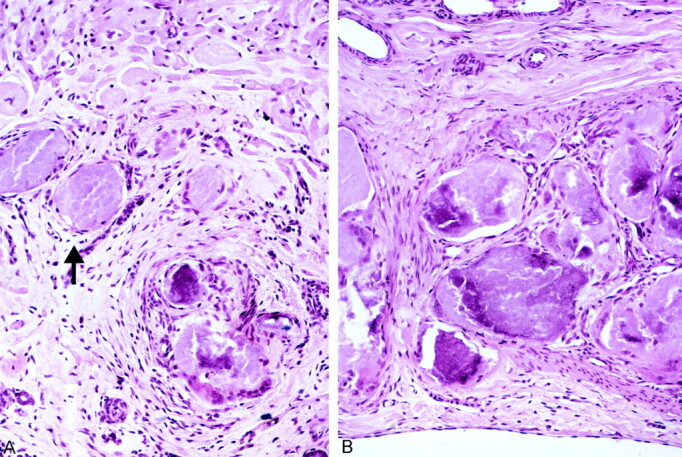
Photomicrographs.
A, Three weeks after embolization, kidney shows hydroxyapatite microparticles (arrow) reaching the peripheral renal medullary arteries of approximately 200 μm in diameter. No arterial wall necrosis, extraluminal migration, or hemorrhagic changes are found. Several small round cells can be seen in the thrombus (hematoxylin and eosin; original magnification, ×100).
B, Histologic findings in larger arteries are nearly the same as those in smaller vessels (hematoxylin and eosin; original magnification, ×100).
Discussion
Hydroxyapatite ceramics share numerous microstructural similarities with human hydroxyapatite (19), which accounts for 65% of bones. Excellent biocompatibility and usefulness of hydroxyapatite ceramics have been consistently reported in bone, soft tissues, and other organs (19–21). It has already been used in clinical practice, mainly as a bone substitute (20). Little is known, however, regarding intravascular use (22), especially concerning safety of use and effectiveness as an embolic material to produce intra-arterial occlusion.
Role of Manufacturing Process
The microporous structure of hydroxyapatite ceramics is related to thermal distribution during the manufacturing process. The surface area of hydroxyapatite ceramics is 0.5 m2/g at 1200°C, 22 m2/g at 800°C, and 47 m2/g at 400°C. It is relatively easy to select the adequate temperature for a particular purpose during the process (21). It is also known that apatite structure is degraded by phosphorylation if produced at temperatures >1300°C and that a strong inflammatory response to a foreign body develops if produced at temperatures <700°C (23). As a bone substitute, the characteristics of hydroxyapatite ceramics should be governed during the manufacturing process primarily by its hardness, which leads to less fragility, and also by the appropriate selection of size of microporous structure for osteoblastic induction (24, 25). Hydroxyapatite ceramics produced at approximately 1100°C were reported to have the best performance for these purposes. However, as microparticles for embolization, adequate specific gravity suitable for good suspension with contrast media is required in addition to minimal brittleness. The microparticles that we produced at 800°C well fulfilled all these conditions.
Requirements for Clinical Use
Turjman et al (3) described the requirements for the ideal particulate embolic material: easiness of passing through a microcatheter, effectiveness in producing vascular occlusion, homogeneous embolization, easy availability, biocompatibility, relatively benign inflammatory response, and no carcinogenesis. The easiness of passing through a microcatheter is mainly related to the shape of the particles; nearly spheroid or oval particles with a smooth surface and no spine are ideal for this purpose. Shape also has an effect on the response of the surrounding tissues. Misiek et al (26) implanted hydroxyapatite particles of two different shapes—one smooth and rounded and the other irregular and sharp—in buccal soft tissue and reported that both induced a very mild inflammatory response, although the resolution of the inflammatory response proceeded at a faster rate with the smooth and rounded particles. One additional requirement to help prevent clogging of microcatheters is clear visibility of particles in the suspension of contrast media. We often encounter clogging of microcatheters during embolization with currently available embolic agents, which can be disappointing because successful placement of microcatheters can prove very difficult. It is thought that clogging is primarily related to poor visibility of particles, which keeps the operator unaware of their focal attenuation in the microcatheter and cluster formation, which occurs most commonly at the microcatheter hub. No such clogging occurred with our material. To obtain a homogeneous embolization result, in addition to shape and particulate surface, lack of fragmentation is another criterion that helps during embolization. Our particles, produced at 800°C, were not easily breakable under normal conditions during embolization procedures; also, we were able to show that the particles retained their shape without fragmentation in our histopathologic study. Moreover, hydroxyapatite ceramics are easily available because they have already been in clinical use for some time in several countries. Carcinogenesis has not been reported to date. Application to humans has been approved by the Food and Drug Administration. The remaining two requirements—effectiveness in producing vascular occlusion and a relatively mild and benign inflammatory response—were shown in our experimental animal study. Embolization was complete and persisted for ≤24 weeks without recanalization. A mild inflammatory response, without acute angionecrosis and focal hemorrhage, was observed in the examined sections and was considered to play a synergistic role with the embolic materials to ensure effective thrombosis (3). The results of our experimental study are the first reported results to indicate the usefulness and safety of hydroxyapatite ceramics as an embolic material.
Conclusion
In conclusion, hydroxyapatite ceramic microparticles are an excellent biocompatible embolic material with good visibility during injection control, capable of producing effective occlusion of distal arteriocapillary beds with a resulting mild benign inflammatory response and preservation of the arterial feeders.
References
- 1.Berenstein A, Russell E. Gelatin sponge in therapeutic neuroradiology: a subject review. Radiology 1981;141:105–112 [DOI] [PubMed] [Google Scholar]
- 2.Kumar A, Kaufman SL, Patt J, Posey JB, Maxwell DD, White RI Jr. Preoperative embolization of hypervascular head and neck neoplasms using microfibrillar collagen. AJNR Am J Neuroradiol 1982;3:163–168 [PMC free article] [PubMed] [Google Scholar]
- 3.Turjman F, Massoud TF, Vinters HV, et al. Collagen microbeads: experimental evaluation of an embolic agent in the rete mirabile of the swine. AJNR Am J Neuroradiol 1995;16:1031–1036 [PMC free article] [PubMed] [Google Scholar]
- 4.Dion JE, Rankin RN, Viñuela F, Fox AJ, Wallace AC, Mervart M. Dextran microsphere embolization: experimental and clinical experience with radiologic-pathologic correlation: work in progress. Radiology 1986;160:717–721 [DOI] [PubMed] [Google Scholar]
- 5.Purdy PD, Samson D, Batjer HH, Risser RC. Preoperative embolization of cerebral arteriovenous malformations with polyvinyl alcohol particles: experience in 51 adults. AJNR Am J Neuroradiol 1990;11:501–510 [PMC free article] [PubMed] [Google Scholar]
- 6.Bendszus M, Klein R, Burger R, Warmuth-Metz M, Hoffmann E, Solymosi L. Efficacy of trisacryl gelatin microspheres versus polyvinyl alcohol particles in the preoperative embolization of meningiomas. AJNR Am J Neuroradiol 2000;21:255–261 [PMC free article] [PubMed] [Google Scholar]
- 7.Davidson GS, Terbrugge KG. Histologic long-term follow-up after embolization with polyvinyl alcohol particles. AJNR Am J Neuroradiol 1995;16[suppl 4]:843–846 [PMC free article] [PubMed] [Google Scholar]
- 8.Quisling RG, Mickle JP, Ballinger WB, Carver CC, Kaplan B. Histopathologic analysis of intraarterial polyvinyl alcohol microemboli in rat cerebral cortex. AJNR Am J Neuroradiol 1984;5:101–104 [PMC free article] [PubMed] [Google Scholar]
- 9.Teasdale E, Patterson J, McLellan D, Macpherson P. Subselective preoperative embolization for meningiomas: a radiological and pathological assessment. J Neurosurg 1984;60:506–511 [DOI] [PubMed] [Google Scholar]
- 10.Wakhloo AK, Juengling FD, Van Velthoven V, Schumacher M, Hennig J, Schwechheimer K. Extended preoperative polyvinyl alcohol microembolization of intracranial meningiomas: assessment of two embolization techniques. AJNR Am J Neuroradiol 1993;14:571–582 [PMC free article] [PubMed] [Google Scholar]
- 11.Hieshima GB, Everhart FR, Mehringer CM, et al. Preoperative embolization of meningiomas. Surg Neurol 1980;14:119–127 [PubMed] [Google Scholar]
- 12.Suyama T, Tamaki N, Fujiwara K, Hamano S, Kimura M, Matsumoto S. Peritumoral and intratumoral hemorrhage after gelatin sponge embolization of malignant meningioma: case report. Neurosurgery 1987;21:944–946 [DOI] [PubMed] [Google Scholar]
- 13.Kallmes DF, Evans AJ, Kaptain GJ, et al. Hemorrhagic complications in embolization of a meningioma: case report and review of the literature. Neuroradiology 1997;39:877–880 [DOI] [PubMed] [Google Scholar]
- 14.Hayashi T, Shojima K, Utsunomiya H, Moritaka K, Honda E. Subarachnoid hemorrhage after preoperative embolization of cystic meningioma. Surg Neurol 1987;27:295–300 [DOI] [PubMed] [Google Scholar]
- 15.Motozaki T, Otuka S, Sato S, et al. Preoperative embolization with gelfoam powder for intracranial meningioma causing unusual peritumoral hemorrhage: with reference to the mechanism of hemorrhage [in Japanese]. No Shinkei Geka 1987;15:95–101 [PubMed] [Google Scholar]
- 16.Watanabe K, Matsumura K, Matsuda M, Handa J. Meningioma with intratumoral and subdural hemorrhage as an immediate complication of therapeutic embolization: case report [in Japanese]. Neurol Med Chir (Tokyo) 1986;26:904–907 [DOI] [PubMed] [Google Scholar]
- 17.Schumacher M, Horton JA. Treatment of cerebral arteriovenous malformations with PVA: results and analysis of complications. Neuroradiology 1991;33:101–105 [DOI] [PubMed] [Google Scholar]
- 18.Sorimachi T, Koike T, Takeuchi S, et al. Embolization of cerebral arteriovenous malformations achieved with polyvinyl alcohol particles: angiographic reappearance and complications. AJNR Am J Neuroradiol 1999;20:1323–1328 [PMC free article] [PubMed] [Google Scholar]
- 19.Costantino PD, Friedman CD, Jones K, Chow LC, Pelzer HJ, Sisson GA Sr. Hydroxyapatite cement: I. basic chemistry and histologic properties. Arch Otolaryngol Head Neck Surg 1991;117:379–384 [DOI] [PubMed] [Google Scholar]
- 20.Okumura T, Oda Y, Mori K. Tissue compatibility of newly developed bioceramics. Neurol Med Chir (Tokyo) 1984;24:909–914 [DOI] [PubMed] [Google Scholar]
- 21.Salyer KE, Hall CD. Porous hydroxyapatite as an onlay bone-graft substitute for maxillofacial surgery. Plast Reconstr Surg 1989;84:236–244 [DOI] [PubMed] [Google Scholar]
- 22.Tsugita M, Tsuru S, Takasaki K, et al. Basic study of chemo-embolization of the liver using hydroxyapatite granules [in Japanese]. Gan To Kagaku Ryoho 1989;16:3423–3428 [PubMed] [Google Scholar]
- 23.de Groot K. Bioceramics consisting of calcium phosphate salts. Biomaterials 1980;1:47–50 [DOI] [PubMed] [Google Scholar]
- 24.Hulbert SF, Morrison SJ, Klawitter JJ. Tissue reaction to three ceramics of porous and non-porous structures. J Biomed Mater Res 1972;6:347–374 [DOI] [PubMed] [Google Scholar]
- 25.Predecki P, Stephan JE, Auslaender BA, Mooney VL, Kirkland K. Kinetics of bone growth into cylindrical channels in aluminum oxide and titanium. J Biomed Mater Res 1972;6:375–400 [DOI] [PubMed] [Google Scholar]
- 26.Misiek DJ, Kent JN, Carr RF. Soft tissue responses to hydroxyapatite particles of different shapes. J Oral Maxillofac Surg 1984;42:150–160 [DOI] [PubMed] [Google Scholar]