Abstract
BACKGROUND AND PURPOSE: The objective of this study was to assess whether MR imaging can image the neurovascular bundle in patients with fractures of the mandible. In addition, an attempt was made to evaluate whether MR images provide information regarding the continuity of the inferior alveolar nerve before surgery and regarding signal intensity changes after trauma.
METHODS: We analyzed preoperative MR images of 23 patients with mandibular fractures. Object-oriented sagittal view proton density- and T1-weighted sequences (before and after the administration of contrast agent) were used not only in an attempt to obtain purely qualitative information regarding nerve continuity in the neurovascular bundle (inferior alveolar nerve, artery, vein) but also to perform quantitative region-of-interest measurements of signal intensities at four defined measurement sites. The measurements were compared with those obtained for a patient population with healthy mandibles.
RESULTS: It was possible to interpret MR images in 21 cases. MR imaging findings showed that the neurovascular bundle had been cut in two patients and was intact in the remaining 19 patients. These MR imaging findings were confirmed intraoperatively in all cases. Although we found no significant signal intensity differences between patients with intact nerves and patients with cut nerves, we found significant differences between patients with mandibular fractures and patients with unremarkable mandibles.
CONCLUSION: It is possible to diagnose the interruption of nerve continuity by using MR imaging. Signal intensity measurements in the neurovascular bundle provide no information regarding nerve continuity.
Fractures of the mandible often accompany minor traumas. Dislocated fractures are usually treated by osteosynthesis (ie, the mandible is surgically fixed by using a metal or biodegradable implant) (1). If clinical signs or symptoms of a nerve lesion are present, the continuity of the nerve is examined and, if indicated, restored by epineurial repair or interfascicular nerve grafting. Whether a nerve lesion is suspected depends on the clinical neurologic examination and the extent of fracture dislocation. New methods assess the sensibility of the nerve to heat stimulation in the region of the mental foramen. All methods use an indirect approach to diagnosing nerve injury. A direct method of detecting nerve lesions is still unavailable.
Improved MR imaging software and hardware have made it possible to produce detailed images of cranial nerves. The T2 constructive interference in steady state sequence has shown what high resolution is necessary to image these fine structures (2). The visualization of pathologic processes in nerves requires not only high resolution T2-weighted sequences but also proton density- and T1-weighted sequences if neural structures that are not surrounded by liquor are to be imaged with sufficient contrast and if signal intensity changes are to be quantified after contrast agent administration (3). In vitro studies and recent case reports (4–7) have shown that it is possible to obtain MR images of the mandible that meet the aforementioned requirements.
The objective of this study was to assess whether it is possible to visualize the neurovascular bundle of the mandibular canal in patients with mandibular fracture. In addition, we attempted to image the continuity of the nerve before surgery.
Methods
We retrospectively analyzed the MR images of 23 patients with mandibular fractures who had been examined between July 2000 and January 2002 (19 men and four women; age range, 18–64 years; mean age, 28.3 years). The examinations were performed on a 1.5-T imaging unit. We used object-oriented sagittal view T1-weighted sequences (15/6.1 [TR/TE]; flip angle, 30 degrees; fat saturated; field of view, 270 mm; matrix, 512 × 326 mm; section thickness, 1.5 mm; imaging time, 3/50 min [before/after administration of contrast agent]) and proton density-weighted sequences (15/6.1; flip angle, 15 degrees; field of view, 270 mm; matrix 512 × 326 mm; section thickness, 1.5 mm; imaging time, 3/50 min [before/after administration of contrast agent]). Nerve continuity was assessed on the basis of the proton density-weighted sequences. A radiologist who was unfamiliar with the clinical signs and symptoms of the patients evaluated subjectively whether an interruption of nerve continuity was visible. Nerve interruption was diagnosed when the continuity of the nerve bundle was no longer visible and when individual damaged nerve fibers were visible in the area of the fracture site. After the MR imaging examination, all patients received surgical treatment. The continuity of the inferior alveolar nerve was assessed intraoperatively.
Signal intensities were measured at four particular sites in the neurovascular bundle, which had been defined as regions of interest (minimum size, 15 voxels; maximum size, 32 voxels) for the sagittal view T1-weighted sequences before and after the administration of contrast agent. Two regions of interest were proximal and two were distal to the fracture. For each measurement site, we thus obtained one signal intensity value before and one after the administration of contrast agent. These two values were used to calculate a percent of signal intensity increase for each of the four measurement sites. Signal intensity increases were determined for the entire patient population, for patients with neurologic disorders of the inferior alveolar nerve, and for patients with severe dislocation. The values obtained for these groups were compared with those obtained for a patient population with healthy mandibles (29 patients, each of whom had undergone MR imaging for possible mandibular disease and was found to have an unremarkable mandibula) on one side (t test) (Fig 1).
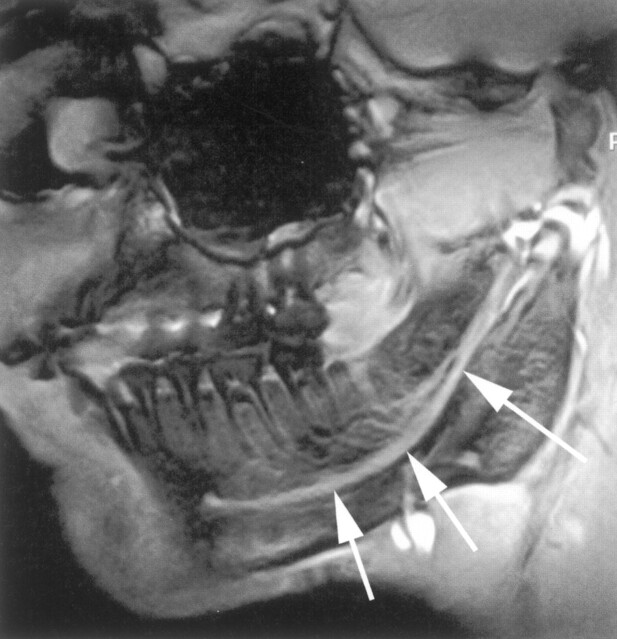
Fig 1.
Sagittal view proton density-weighted fast field-echo image. Mandibular MR image of a patient with a healthy mandible shows a normal neurovascular bundle (arrows).
Results
It was possible to interpret 21 of the 23 MR imaging examinations. In two of the 23 cases, motion artifacts made it impossible to assess the neurovascular bundle accurately, although the mandibular canal was still defined.
Based on subjective evaluation of the neurovascular bundles, the radiologist (B.K.) came to the conclusion that the continuity of the nerve was interrupted in two patients (Fig 2) and that the nerves were intact in the remaining 19 patients (Fig 3). In all cases, surgical exploration confirmed the MR imaging findings.
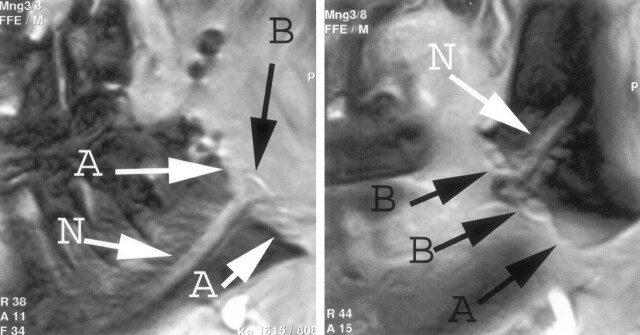
Fig 2.
Sagittal view proton density-weighted fast field-echo images. Severely dislocated fracture of the mandible (A arrows) and individual ruptured nerve fibers of the neurovascular bundle in the fracture site (B arrows) can be seen. Images clearly show an interruption of the neurovascular bundle (N arrows).
Fig 3.
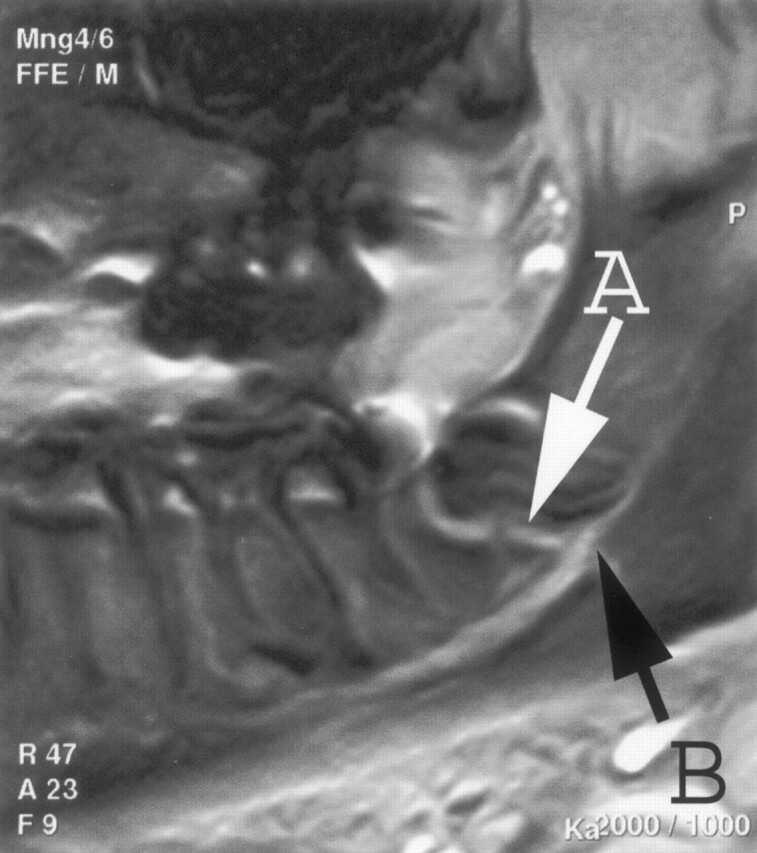
Sagittal view proton density-weighted fast field-echo image. Severely dislocated fracture of the mandible can be seen. In contrast to Figure 2, however, this image shows no interruption of the neurovascular bundle (B arrow) at the fracture site (A arrow). Accordingly, nerve continuity is confirmed on the basis of MR imaging findings.
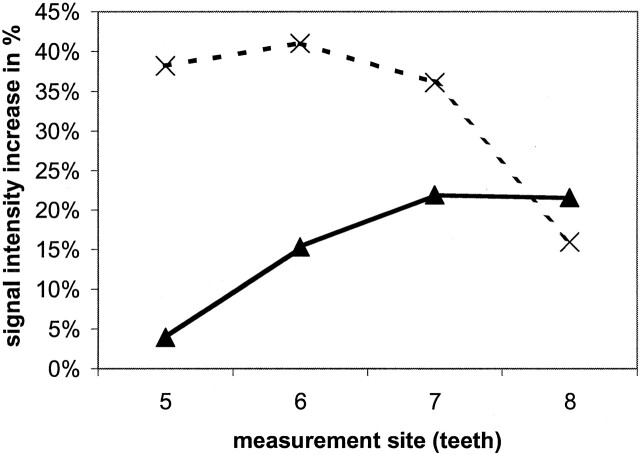
Signal intensity measurements provided evidence of differences among the various groups of patients. A comparison of the signal intensity increases measured for patients with fractures of the mandible and the values for the patient population with healthy mandibles showed that after the administration of contrast agent, the patients with mandibular fractures had far higher signal intensity increases at the two distal sites and at the nearest proximal site than did the patients with healthy mandibles. The differences were statistically significant (measurement site 2 [second molar], P = .025; measurement site 3 [first molar], P < .01; measurement site 4 [second premolar], P = .015). The signal intensity increases measured for the patients at the first proximal measurement site were similar to those obtained for the patients with healthy mandibles; these differences were not significant (P > .05) (Fig 4). Similarly, the differences between the signal intensity increases measured for patients with neurologic disorders and those for patients without neurologic abnormalities were not statistically significant (P = .13).
Fig 4.
Graph shows comparison of signal intensity increases measured for patients with mandibular fractures and patients with healthy mandibles at four measurement sites. Solid line with triangles, mean values for patients with healthy mandibles; dashed line with Xs, mean values for patients with mandibular fractures.
Patients with severe dislocation of the mandibular fracture showed higher signal intensity increases than did patients with minor dislocation of the fracture. The differences in the measurements obtained for the two groups of patients at the two proximal measurement sites were not significant (measurement site 1, P = .56; measurement site 2, P = .49); however, the differences in the measurements obtained at the two distal sites were more significant (measurement site 3, P = .07; measurement site 4, P = .005). Neither the age of the patient nor the affected side had an effect on signal intensity differences.
Discussion
Mandibular fractures can be associated with damage to the neurovascular bundle in the mandibular canal. Nerve ruptures can cause neuralgia and impaired sensibility. Long-term sequelae of nerve injury can be prevented by epineurial repair or interfascicular nerve grafting. Before these are performed, however, an interruption of nerve continuity must be diagnosed. A safe diagnosis can be established by surgical exploration. When conservative treatment is chosen, nerve damage is assessed on the basis of the extent of impaired sensibility. Thus, it is impossible to make a safe diagnosis when a conservative approach is chosen.
Unlike CT, MR imaging allows imaging of the neurovascular bundle (5). This requires the use of a high resolution technic (512 matrix), a surface coil, and a low section thickness. In vitro studies have shown that it is possible to accurately image the neurovascular bundle when these requirements are met. 3-T systems even allow nerves to be distinguished from vessels (4). Case reports suggest that it is also possible to visualize the neurovascular bundle in vivo (3).
The results we obtained for a patient population confirmed this finding. We were able to provide information regarding nerve continuity for all patients for whom interpretable examination results were available. All our findings were confirmed intraoperatively.
Signal intensity measurements in the neurovascular bundle, which provide valuable prognostic results for other cranial nerves (ie, grade of inflammation or perfusion), show no differences between patients with intact or interrupted nerves. This may be because of the partial volume effects, which are unavoidable when a section thickness of 1.5 mm is used. However, when comparing patients with mandibular fractures with patients with healthy mandibles, we observed significant signal intensity differences at the two measurement sites nearest to the fracture and at the most distal site. This may be because of increased perfusion of the neurovascular bundle in response to the trauma.
To some extent, MR imaging is limited by motion artifacts, which is the reason it was impossible to interpret two of the 23 examinations. These motion artifacts were associated with intraoral soft-tissue injuries, which accompany acute fractures of the mandible and may cause swallowing movements. However, high resolution images, which could be used for diagnostic purposes, were available from 21 patients.
Signal intensity measurements have shown that it is possible to image changes in the neurovascular bundle by using high resolution technology. Our study provided evidence of considerable signal intensity differences between the patient population with mandibular fractures and the patient population with healthy mandibles. However, we were unable to distinguish between patients with and those without neurologic disorders on the basis of signal intensity measurements. This may be because of the limitation of the retrospective analysis, which included a section thickness of 1.5 mm. This section thickness causes partial volume effects that make it impossible to measure the nerve separately. The differences between patients with mandibular fractures and those with healthy mandibles strongly suggest that MR imaging-based signal intensity measurements provide evidence of pathophysiological processes in the inferior alveolar nerve as well as in other cranial nerves (3).
Conclusion
What are the ramifications of these results for the clinical approach to patients with fractures of the mandible? Conventional radiographs or CT scans continue to be sufficient for evaluating patients without neurologic disorders and patients who need surgery. Patients who are to receive conservative treatment and who show a neurologic abnormality in the area of the inferior alveolar nerve can undergo an MR imaging examination before wiring. MR images, including sagittal view proton-density sequences, make it possible to establish with certainty whether the neurovascular bundle is intact.
References
- 1.Ellis E III. Treatment methods for fractures of the mandibular angle. Int J Oral Maxillofac Surg 1999;28:243–252 [PubMed] [Google Scholar]
- 2.Casselman J, Kuhweide R, Deimling M, Ampe W, Dehaene I, Meeus L. Constructive interference in steady state-3DFT MR imaging of the inner ear and cerebellopontine angle. AJNR Am J Neuroradiol 1993;14:47–57 [PMC free article] [PubMed] [Google Scholar]
- 3.Kress BP, Griesbeck F, Efinger K, et al. Bell’s palsy: what is the prognostic value of measurements of signal intensity increases with contrast enhancement on MRI? Neuroradiology 2002;44:428–433 [DOI] [PubMed] [Google Scholar]
- 4.Ikeda K, Ho KC, Nowicki BH, Haughton VM. Multiplanar MR and anatomic study of the mandibular canal. AJNR Am J Neuroradiol 1999;17:579–584 [PMC free article] [PubMed] [Google Scholar]
- 5.Gahleitner A, Nasel C, Schick S, Bernhart T, Mailath G, Dorffner S, Watzek G, Imhof H, Trattnig S. Dental magnetic resonance tomography (dental MRI) as a method for imaging maxillo-mandibular tooth retention structures [in German]. Rofo Fortschr Geb Rontgenstr Neuen Bildgeb Verfahr 1998;169:424–428 [DOI] [PubMed] [Google Scholar]
- 6.Nasel C, Gahleitner A, Breitenseher M, Czerny C, Solar P, Imhof H. Dental MR tomography of the mandible. J Comput Assist Tomogr 1998;22:498–502 [DOI] [PubMed] [Google Scholar]
- 7.Salvolini E, De Florio L, Regnicolo L, Salvolini U. Magnetic resonance applications in dental implantology: May–June technical notes and preliminary results. Radiol Med (Torino) 2002 May–June;103:526–529 [PubMed] [Google Scholar]