Abstract
Summary: We describe a case of presumed postpartum infundibuloneurohypophysitis, which is a rare inflammatory process involving the pituitary stalk and posterior pituitary. Only one case has been previously reported in a postpartum woman. Serial MR images obtained in our patient revealed spontaneous regression of inflammation. The critical position of the inflammation leads to hormonal deficiencies, mostly involving the posterior pituitary. Treatment options include hormone replacement; the role of pharmacological steroids is controversial.
Infundibuloneurohypophysitis typically presents with diabetes insipidus. It is an uncommon disorder, likely of autoimmune origin. To the best of our knowledge, only one case in a postpartum patient has been reported in the literature (1). Here we report another case in a postpartum patient.
Case Report
A 22-year-old woman presented for evaluation of polyuria and polydipsia. Her symptoms started approximately 6 months after she had uncomplicated vaginal delivery. The patient reported urine volume >8 liters per day. She was unable to resume menstrual cycles and had persistent galactorrhea. On review of systems, she had 10 kg of weight gain over 6 months and reported headaches but denied blurred vision. Her medical and family histories were unremarkable, and she was not taking any medications. Visual fields were intact to confrontation. Laboratory data were remarkable for serum osmolality of 300 mOsm/kg H2O and urine osmolality of 62 mOsm/kg H2O with serum sodium of 153 mEq/L, confirming the clinical diagnosis of diabetes insipidus. MR imaging of the brain (1.5T MR system) showed a solid enhancing mass within the pituitary infundibulum measuring 3 × 5 × 4 mm located just inferior to the optic chiasm with loss of posterior pituitary hyperintensity (Fig 1A–C). Anterior pituitary function testing—including prolactin, luteinizing hormone (LH), follicle-stimulating hormone (FSH), thyrotropin (TSH), free thyroxin 4 (FT4), and corticotropin (ACTH) stimulation tests—was normal. Visual field testing, serum angiotensin-converting enzyme (ACE) level, and chest radiography findings were normal. Lumbar puncture did not reveal any evidence of malignancy by cytology.
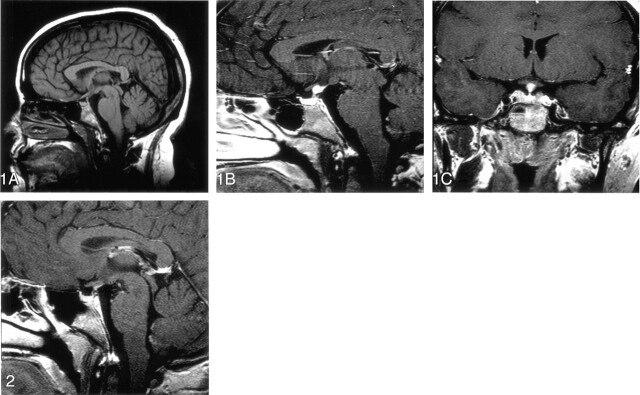
Fig 1.
MR images obtained in a postpartum 20-year-old woman with presumed infundibuloneurohypophysitis.
A, Sagittal precontrast T1-weighted image demonstrates thickening of the superior aspect of infundibulum with loss of posterior pituitary hyperintensity.
B and C, Sagittal (B) and coronal (C) contrast-enhanced T1-weighted images demonstrate enhancement of the thickened superior infundibulum.
On the basis of clinical presentation, laboratory, and imaging data, a presumptive diagnosis of infundibuloneurohypophysitis was made. Differential diagnosis also included germinoma and granulomatous diseases such as sarcoidosis. These were, however, considered to be unlikely in view of normal serum ACE level, chest radiography findings, and lumbar puncture results. Therapy with desmopressin (DDAVP) nasal spray 10 mg twice a day and parlodel 7.5 mg at bedtime was initiated. The patient had prompt resolution of polyuria and a decrease in galactorrhea shortly after starting the therapy. She continued to have weight gain, however, and had not resumed menses 9 months later, so cyclical estrogen therapy with oral contraceptives was started. During her last follow-up visit, she continued to complain of weight gain. No other hormonal deficiencies were detected. The patient continues to take DDAVP and oral contraceptives. Serial pituitary MR images revealed a gradual decrease in size of the enhancing superior infundibular lesion. Follow-up imaging after 4 years shows total resolution of contrast enhancement (Fig 2).
Fig 2.
Contrast-enhanced sagittal T1-weighted image demonstrates resolution of contrast enhancement and thickening of the superior aspect of infundibulum.
Discussion
Lymphocytic hypophysitis is a rare noninfectious, probable autoimmune inflammatory disorder of the pituitary (1–6). Depending on the location of the lesion, they have been characterized into lymphocytic adenohypophysitis (LAH) (3, 5) with or without involvement of the neurohypophysis and lymphocytic infundibuloneurohypophysitis (LIN) (1, 2, 4). LAH rarely presents with diabetes insipidus (5), whereas this is usually the presentation in cases of LIN (2, 4).
LAH, the more frequent of the two, has been described mostly in the postpartum period, although there are reports of this disease occurring in men and postmenopausal women (3). Hashimoto et al (3) reviewed 124 cases of lymphocytic adenohypophysitis, and nearly 60% of them had onset of disease in relation to pregnancy. Lymphocytic and plasma cell infiltration of the anterior pituitary has been verified histologically in LAH (6). Lymphocytic adenohypophysitis presents with an enlarged enhancing anterior pituitary with isolated or multiple hormonal deficiencies. Generally, in the ascending order, are deficiencies of growth hormone, serum prolactin, FSH/LH, TSH and ACTH are involved (4). A possible hypothesis to explain this phenomenon is the topographical location of pituitary cells and the centrifugal pattern of pituitary blood flow, which lead to progressive spreading of inflammation in that order.
LIN typically presents as central diabetes insipidus (2, 4, 5) as seen in our patient. Imura et al (2) reviewed 17 cases of idiopathic diabetes insipidus; MR imaging findings were consistent with those of LIN. Two of these patients had histologic verification of T-cell infiltration of infundibulum and neurohypophysis. The lesion typically is isolated to the pituitary stalk. The posterior pituitary retains its connections with the hypothalamus, via the hypothalamic hypophyseal tract, and functions as a primary reservoir for vasopressin and oxytocin, unlike the anterior pituitary, which has the capability of synthesizing its own hormones. Anterior pituitary function can be affected in LIN by the critical location of the lesion in the stalk leading to disruption of regulatory hormones or secondary to progression to involve the adenohypophysis. Most of the reported cases of LIN, however, remain isolated to the pituitary stalk without extension to involve the adenohypophysis or anterior pituitary hormonal deficiency (1, 2, 4). The MR imaging finding of an enhancing mass in the stalk is often associated with loss of hyperintensity in the posterior pituitary, although isolated absence of the hyperintense posterior pituitary could be a normal variant (7). Why MR imaging and histologic studies show disease to be restricted to the posterior pituitary remains unknown (8). The differential diagnosis includes sarcoidosis, Wegner granulomatosis, eosinophilic granuloma, metastasis, neoplasm-like germinoma, and, rarely, syphilis. Enlargement of the stalk can have tumor-like appearance, and some patients have undergone pituitary exploration because of suspicion of a pituitary tumor (9).
Our patient did not have a clinical or laboratory manifestation of the above entities and presented in the postpartum period. Our review of literature revealed only one reported case of LIN presenting in postpartum women (1). None of 17 patients in the Imura series (2) presented in the postpartum period. In two of the 17 patients who received glucocorticoid treatment after surgery, the width of the pituitary stalk diminished. The lesions regressed spontaneously in the other 15 patients (2). The clinical and radiological presentation in our patient was classic infundibuloneurohypophysitis, possibly of lymphocytic origin; after discussion with the patient, we chose to follow up the patient with hormone replacement therapy and to forgo performing a biopsy to verify the diagnosis.
Both adenohypophysitis and lymphocytic infundibulohypophysitis have long been considered to be of autoimmune origin but with different antigenic stimuli (2, 10). In LIN, the self-limiting inflammatory process is compatible with the autoimmune hypothesis of idiopathic diabetes insipidus (2). The preponderance of women in published series (2) and the presence of T-cell infiltration in biopsy-proved cases also favor this hypothesis. Presentation in the postpartum period in our patient also supports this hypothesis. Moreover, reports of coexistence of LIN with other autoimmune diseases such as lupus erythematosis also suggest an autoimmune etiology of this disorder (5, 11). Vasopressin cell antibodies (AVP) have been found in patients with idiopathic diabetes insipidus with or without other autoimmune diseases (10). Recently, De Bellis et al (12) showed the presence of AVP antibodies in patients with diabetes insipidus and pituitary stalk thickening consistent with LIN. In the same series, patients with diabetes insipidus but without pituitary stalk thickening did not have AVP antibodies. Therefore, the presence of AVP antibodies appears to be a good marker of autoimmune diabetes insipidus in patients with LIN (12).
Conclusion
Our patient was treated with DDAVP only, and steroid treatment was not initiated. On serial MR images, the mass showed spontaneous regression, which is consistent with the presumptive diagnosis of infundibuloneurohypophysitis. The patient remains on desmopressin consistent with most other cases that show permanent diabetes insipidus. We believe that, in the proper clinical context, an invasive biopsy with possible detrimental complications can be avoided and close follow-up with MR imaging and supportive hormonal therapy is the most judicious option.
References
- 1.Havenbergh TV, Robberecht W, Wilms G, et al. Lymphocytic infundibulohypophysitis presenting in the postpartum period: case report. Surg Neurol 1996;46:280–246 [DOI] [PubMed] [Google Scholar]
- 2.Imura H, Nakao K, Shimastu A, et al. Lymphocytic infundibuloneurohypophysitis as a cause of central diabetes insipidus. N Engl J Med 1993;329:683–689 [DOI] [PubMed] [Google Scholar]
- 3.Ahmed SR, Aiello DP, Page R, et al. Necrotizing infundibulo-hypophysitis: a unique syndrome of diabetes insipidus and hypopituitarism. J Clin Endocrinol Metab 1993;76:1499–1504 [DOI] [PubMed] [Google Scholar]
- 4.Tubirdy N, Saunders D, Thom M, et al. Infundibulohypophysitis in a man presenting with diabetes insipidus and cavernous sinus involvement. J Neurol Neurosurg Psychiatry 2001;71:798–801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hashimoto K, Takao T, Makino S. Lymphocytic adenohypophysitis and lymphocytic infundibulohypophysitis. Endocr J 1997;44:1–10 [DOI] [PubMed] [Google Scholar]
- 6.Nishioka H, Ito H, Sano T, Ito Y. Two cases of lymphocytic hypophysitis presenting with diabetes insipidus: a variant of lymphocytic infundibulo-neurohypophysitis. Surg Neurol 1996;46:285–290 [DOI] [PubMed] [Google Scholar]
- 7.Sato N, Sze G, Endo K. Hypophysitis: endocrinoogical and dynamic MR findings. AJNR Am J Neuroradiol 1998;19:439–444 [PMC free article] [PubMed] [Google Scholar]
- 8.Kojima H, Nojima T, Nagamshima K, et al. Diabetes insipidus caused by lymphocytic infundibulo-neurohypophysitis. Arch Pathol Lab Med 189;113:1399–1401 [PubMed] [Google Scholar]
- 9.Tsujii S, Takeuchi J, Koh M, et al. A candidate case for lymphocytic infundibulo-neurohypophisitis mimicking a neurohypophysial tumor. Intern Med 1997;36:293–297 [DOI] [PubMed] [Google Scholar]
- 10.Scherbaum WA, Bottazzo GF, Czernichow P, et al. Role of autoimmunity in central diabetes insipidus. In Czernichow P, Robinson AG, eds. Diabetes insipidus in man. Basel: Karger;1985:232–239 [Google Scholar]
- 11.Hashimoto K, Asaba K, Tamura K, et al. A case of lymphocytic infundibuloneurohypophysitis associated with systemic lupus erythematosus. Endocr J 2002;49:605–610 [DOI] [PubMed] [Google Scholar]
- 12.De Bellis A, Colao A, Bizzarro A, et al. Longitudinal study of vasopressin-cell antibodies and of hypothalamic –pituitary region on magnetic resonance imaging in patients with autoimmune and idiopathic complete central diabetes insipidus. J Clin Endocrinol Metab 2002;87:3825–3829 [DOI] [PubMed] [Google Scholar]