Abstract
Summary: Massive hemoptysis is not commonly seen in patients who have nasopharyngeal carcinoma. It most often is the result of both radiation therapy and skull base infection. We present a practical imaging approach by using MR imaging and conventional angiography that may facilitate the prevention of such life-threatening bleeding and help provide effective control of infection. With the aid of these studies, clinicians may be able to manage this condition with more confidence.
Patients with nasopharyngeal carcinoma (NPC) who have been treated with high-dose radiation therapy are at risk of developing carotid artery erosion and even pseudoaneurysm formation with possible life-threatening epistaxis. The occurrence of epistaxis after treating a patient with a head and neck malignancy has been reported elsewhere (1). The published literature on this topic primarily stresses treatment options such as external compression, transarterial embolization, or more recently, the use of covered stents (2, 3). We report the cases of three patients treated with 3D conformal radiation therapy for NPC who demonstrated focal soft tissue necrosis at follow-up MR imaging examination and who then had subsequent massive hemorrhage. The presence of this MR imaging finding should suggest further evaluation of the vasculature by conventional angiography. The purpose of this article is to report this uncommon finding in patients treated with radiation therapy for an NPC and emphasize the usefulness of angiography to rule out the possible formation of a pseudoaneurysm of the internal carotid artery and thus guide further treatment strategy. To the best of our knowledge, this MR imaging finding has not been previously highlighted as a warning sign indicating that immediate angiography should be performed.
Case Reports
Case 1
A 55-year-old man, who had a diagnosis of NPC 1 year earlier, underwent a complete course of concomitant chemoradiation therapy. He had an uneventful clinical course until 2 weeks before admission, when he developed otorrhea and a malodorous postnasal drip. MR imaging showed nonenhancing soft tissue containing small air bubbles in the left lateral recess of the nasopharynx with superiolateral extension to the carotid artery (Fig 1A–C). The diagnostic impression was that of necrosis of the pharyngeal mucosa, underlying soft tissues, and the skull base, possibly related to the either radiation therapy or an aggressive infection. The patient had no other significant complaints. Two weeks after the MR imaging study, the patient suddenly had massive epistaxis. Bleeding was initially controlled by Vaseline gauze packing of the nasopharynx. On the 2nd hospital day, the patient sustained another massive bleed with a subsequent drop in blood pressure, development of a fever, and an altered mental status. An emergency angiogram obtained after failing to maintain the patient’s vital signs showed an aneurysmal sac protruding from the high cervical carotid artery (Fig 1D). The active pooling of contrast media into the parapharyngeal space could be clearly appreciated at fluoroscopy. Adequate collateral flow from the right internal carotid artery and the posterior circulation was noted, and the left carotid artery was occluded by an inflated balloon with the subsequent cessation of the bleeding. Although there was no more active bleeding, the fulminant bacterial-fungal infection persisted for 2 months. Supportive antifungal drug therapy failed to control the infection, and the patient died of meningioencephalitis and sepsis.
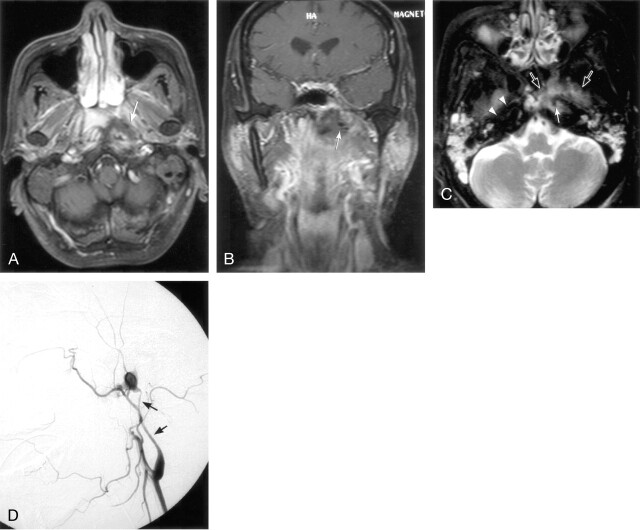
Fig 1.
Case 1, with nasopharyngeal tissue necrosis and pseudoaneurysm, led to a grave outcome.
A, Axial contrast-enhanced T1-weighted MR image shows the nonenhancing soft tissues, mixed with tiny air bubbles in left-sided nasopharyngeal lateral recess (arrow).
B, Coronal contrast-enhanced T1-weighted image shows a complex mass containing soft tissue and air bubbles (arrow) just beneath skull base.
C, Axial T2-weighted MR image shows an intermediate hyperintense soft tissue mass (open arrows) surrounding the high cervical carotid artery with possible aneurysm formation (arrow). Note the normal right carotid artery for comparison (arrowheads).
D, Left carotid angiogram, lateral projection, shows an aneurysm with rapid contrast medium filling and extravasation in the high cervical internal carotid artery (arrows), after which no antegrade flow beyond the aneuyrsm is identified.
Case 2
A 59-year-old man had been uneventfully treated for NPC 1 year earlier. He then developed intermittent self-limited epistaxis along with halitosis. Nasopharyngoscopy showed irregular, sloughing mucosa, and a nasopharyngeal swab culture revealed a fungal infection. An MR imaging study showed tissue necrosis extending from the lateral nasopharyngeal mucosal surface to the ipsilateral carotid artery. The carotid artery lumen just proximal to the skull base appeared to be abnormally dilated, raising the suspicion of an aneurysm. Unfortunately, 2 days after the MR imaging study, the patient suffered a massive epistaxis at home and died.
Case 3
A 50-year-old man had a history of recurrent NPC that was treated with a second regimen of conformal radiation therapy 6 months prior. Two weeks before admission, he developed frequent episodes of hemoptysis, followed by episodes of fever. An MR imaging study showed similar findings to those seen on the previous two cases that suggested tissue necrosis associated with osteomyelitis (Fig 2A, B). Nasopharyngoscopy showed considerable amount of blood-tainted debris present in the nasopharyngeal roof. The otorhinolaryngoleal surgeons were hesitant to debride the wound because of the risk of provoking uncontrollable bleeding or inducing the rupture of the aneurysm. This hesitancy was based on our experience with the prior two cases. The angiogram performed on the 2nd hospital day showed no evidence of active bleeding or pseudoaneurysm formation from either the external and internal carotid arteries around the regions of skull base and nasopharynx. In this setting, the clinician debrided the sloughing tissue and cauterized the smaller bleeders, after which broad-spectrum antibiotics were given. The tissue cultures showed the presence of a streptococcal infection, and the patient made the recovery with no further episodes of hemoptysis or fever. He was discharged on the 15th hospital day.
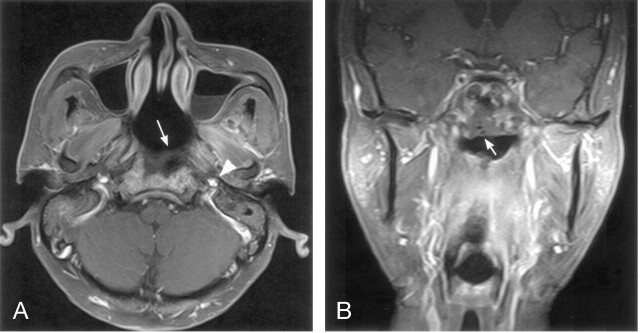
Fig 2.
Case 3, with similar MR findings to Case 1, had a prompt angiography study and much better prognosis.
A, Axial contrast-enhanced T1-weighted image shows a nonenhancing soft tissue in the right nasopharyngeal lateral recess, extending to the carotid sheath (arrows) and encasing the carotid artery (open arrow). Note the contralateral carotid artery for comparison (arrowhead).
B, Coronal contrast-enhanced T1-weighted MR image shows the necrotic mass with lateral extension into the parapharyngeal space (arrow).
Discussion
NPC is among the most common diseases in southern China, Hong Kong, Taiwan, and Singapore. The typical imaging findings are a nasopharyngeal mass, local invasion to the retropharyngeal or parapharyngeal spaces, erosion through the skull base, and cervical lymphadenopathy. Tumor extension to the prestyloid compartment of the parapharyngeal space and then further extension to the carotid sheath are frequent sites of NPC tumor spread (4, 5). Almost every case of NPC typically demonstrates fairly homogeneous enhancement on MR images. Necrotic areas or nonenhancing regions are uncommon imaging findings and the presence of “focal tissue necrosis” is a fairly unique event in either before treatment or after radiation therapy.
We present three patients with NPC and the imaging findings of focal tissue necrosis following their routine course of radiation therapy. Of the thousands of NPC cases treated at our institutions in the past decade, “focal tissue necrosis” secondary to radiation therapy is rare. In addition, although tumor extension through the multiple layers of intervening fascia (6) to the carotid sheath is common, the development of a carotid aneurysm is rare. More commonly, such aneurysms occur secondary to trauma or as a result of a parapharyngeal space infection (7). In our cases, the combination of an infection superimposed on an already fragile radiated mucosa may have led to epistaxis due to small vessel erosion or possibly the formation of an aneurysm. It is proposed that MR imaging alone cannot predict the stability of the perivascular tissue about the carotid artery. A pseudoaneurysm is extremely fragile, because the wall of the artery has been damaged and therefore is more subject to rupture, possibly leading to a rapid, life-threatening event. Hence, once the imaging suspicion of an aneurysm is raised, more aggressive treatment, rather than watchful waiting, is suggested. On the other hand, osteomyelitis of the skull base most commonly is associated with temporal bone infections or immunocompromised patients. Likewise, a history of previous radiation therapy to the head and neck seems to predispose to the development of osteomyelitis as seen in the NPC cases presented. The mainstay of treatment of radiation-induced osteomyelitis is culture-guided antibacterial or antifungal systemic therapy with aggressive surgical debridement of necrotic tissue (8). The results of an angiography study help provide treatment guidelines as demonstrated in our cases.
Conclusion
We present three cases of NPC in patients who had symptoms of fever and halitosis along with the MR imaging findings of necrotic nasopharyngeal tissue. This combination of findings should alert the clinicians involved with the care of these patients that an aneurysm may be present. On the basis of our experience, conventional angiography in these cases may be warranted to guide treatment and thereby avoid the catastrophic events described.
References
- 1.Lam HC, Abdullah VJ, Wormald PJ, Van Hasselt CA. Internal carotid artery hemorrhage after irradiation and osteoradionecrosis of the skull base. Otolaryngol Head Neck Surg 2001;125:522–527 [DOI] [PubMed] [Google Scholar]
- 2.Cheng KM, Chan CM, Cheung YL, et al. Endovascular treatment of radiation-induced petrous internal carotid artery aneurysm presenting with acute haemorrhage: a report of two cases. Acta Neurochir (Wien)2001;143:351–355; discussion 355–356 [DOI] [PubMed] [Google Scholar]
- 3.Low YM, Goh YH. Endovascular treatment of epistaxis in patients irradiated for nasopharyngeal carcinoma. Clin Otolaryngol 2003;28:244–247 [DOI] [PubMed] [Google Scholar]
- 4.Chong VF, Fan YF, Mukherji SK. Carcinoma of the nasopharynx. Semin Ultrasound CT MR 1998;19:449–462 [DOI] [PubMed] [Google Scholar]
- 5.Ng SH, Chang JT, Ko SF, et al. MRI in recurrent nasopharyngeal carcinoma. Neuroradiology 1999;41:855–862 [DOI] [PubMed] [Google Scholar]
- 6.Som PM, Curtin HD. Fascia and spaces of the neck. In: Som PM, Curtin HD, eds. Head and Neck Imaging. 4th ed. St. Louis: Mosby;2003. :1805–1827
- 7.Connors JJ III., Wojak JC. Arteriovenous fistulae and traumatic vascular lesions. In: Connors JJ III, Wojak JC, eds. Interventional Neuroradiology. Philadelphia: WB Saunders;1999. :160–179
- 8.Ducic Y. Management of osteomyelitis of the anterior skull base and craniovertebral junction. Otolaryngol Head Neck Surg 2003;128:39–42 [DOI] [PubMed] [Google Scholar]