Abstract
Summary: Positron emission tomography (PET) has become a critical diagnostic tool in the discovery and staging of malignancies in the head and neck. Although PET is accurate for detecting cancer, increased 18 F-fluorodeoxyglucose (FDG) uptake can be seen in healthy tissues such as muscle, fat, and glands and uptake can be seen in tissues affected by inflammation or granulomatous disease. Combined PET and CT (PET/CT) can often overcome these difficulties by fusing anatomic and physiological data, but radiographic findings of some disease processes can be confusing even with fused imaging techniques. We present two cases of FDG uptake in the posterior pharynx, localized by combined PET/CT, which was initially interpreted as squamous cell carcinoma. The increased activity was ultimately attributed to Teflon-induced granulomas. It is important for radiologists to recognize potential causes of false-positive PET/CT findings to improve our diagnostic accuracy and to avoid unnecessary biopsies and surgeries.
Positron emission tomography (PET) with 18 F-fluorodeoxyglucose (FDG) has been increasingly used in the diagnostic workup of patients with masses in the head and neck (1,2). Although PET can be helpful by detecting an increase in metabolic activity in malignant tissues, it is hindered by a lack of precise anatomic localization. The lack of spatial resolution, along with variable physiological uptake in the head and neck, makes PET prone to false-positive interpretations. The combined technique of PET/CT is ideal for studying lesions of the pharynx because of the improved spatial localization and better differentiation of neoplastic and nonneoplastic tissues (3).
One of the recognized nonneoplastic causes of FDG uptake is granulomatous reactions. Teflon (polytetrafluoroethylene) injected into soft tissues has been shown to cause such granulomatous reactions (4). Before it was known that Teflon caused granulomas, this supposedly inert substance was commonly employed in many areas of medicine, including urology and otolaryngology. Teflon was considered useful because, by nature, it is very stable, the body does not degrade it, and it was thought not to relocate over time. It was used widely in the 1980s to augment areas that were deficient in tissue volume, including the urethral sphincter and the posterior pharynx.
This report discusses the cases of two patients who had been treated with Teflon injection for velopharyngeal insufficiency and demonstrated markedly increased FDG activity in the posterior pharynx on PET/CT scans. The lesions were initially interpreted as malignancies but later proved to be the result of Teflon granulomas.
Case Reports
Case 1
A 68-year-old male patient presented with a 1-week history of progressively worsening bilateral occipital headache. Twenty-five years earlier, the patient had undergone a cleft palate repair with Teflon implant for velopharyngeal insufficiency. Physical examination revealed a submucosal mass in the posterior nasophyarynx.
The patient underwent a whole-body combined PET/CT (CPS Innovations, Knoxville, TN) to evaluate for nasopharyngeal carcinoma and identify potential metastases. Ten milliCurie (mCi) of FDG were administered intravenously, and after a 1-hour delay, contrast-enhanced CT images were obtained from the skull base through the abdomen. The CT portion of the examination demonstrated a 4.7 cm × 2.3 cm enhancing retropharyngeal mass extending from the clivus to the oropharynx (Fig 1). This mass eroded completely through the clivus but was contained by the dura. The mass extended into the left neurovascular space with encasement of the left internal carotid artery but no arterial stenosis. The mass demonstrated diffuse, intense FDG uptake. These findings were considered highly suspicious for squamous cell carcinoma of the nasopharynx. The remainder of the examination was normal, including cervical lymph nodes.
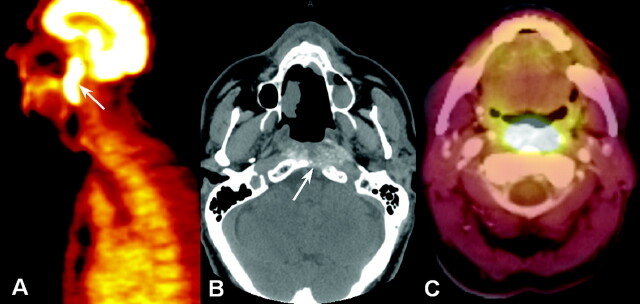
Fig 1.
Pharyngeal Teflon granuloma (case 1).
A, Sagittal PET scan shows a large area of dramatically increased FDG uptake in the posterior pharynx (arrow).
B, Axial unenhanced CT scan (performed 2 days before combined PET/CT) shows heterogeneously increased attenuation throughout the posterior pharyngeal mass. The clivus is eroded (arrow), and surrounding soft tissues are infiltrated. On a contrast-enhanced CT scan, the increased attenuation might be mistaken for enhancement.
C, Fused PET/CT scan obtained at a slightly lower level than that of B demonstrates that the FDG uptake corresponds to the erosive mass.
A transnasal endoscopic biopsy was performed to confirm the diagnosis of malignancy. Histopathologic results demonstrated foreign-body granulomatous reaction with chronic inflammation but no tumor cells. Immunohistochemical staining pattern of the tissue revealed a proliferation of reactive B cells, T cells, and polyclonal plasma cells.
The history of velopharyngeal insufficiency with Teflon injection was deemed the most likely cause of the elevated FDG uptake. The patient, however, remained concerned about malignancy and complained of worsening headaches. He thus underwent two further endoscopic operations to debulk the clival mass. Histopathologic frozen sections at the time of surgery were considered suspicious for chordoma. Final pathologic reports, however, indicated abundant foreign-body giant-cell reaction and reactive fibrosis with no tumor detected, consistent with a Teflon-induced granuloma. Immunohistochemistry was negative for malignant cell markers such as S100, CAM5.3, and EMA.
The patient recovered well and reported complete resolution of his headaches. The dysphagia from his velopharyngeal insufficiency had returned, however, so he underwent pharyngeal hydroxyapatite injection 6 months later. At that time, clinical and radiographic follow-up revealed no evidence of tumor.
Case 2
A 65-year-old male patient presented to an outside hospital with symptoms of dysphagia. He had undergone a velopharyngeal insufficiency repair with Teflon injection 27 years earlier. Physical examination revealed a large mass in the posterior nasopharynx. The patient underwent contrast-enhanced CT of the neck, whole-body PET/CT (Fig 2), and MR imaging of the neck (Fig 3). PET images were obtained with 10-mCi FDG and a 40-minute delay. These examinations were all interpreted as consistent with a nasopharyngeal malignancy, and the patient was referred to an oncologist for treatment.
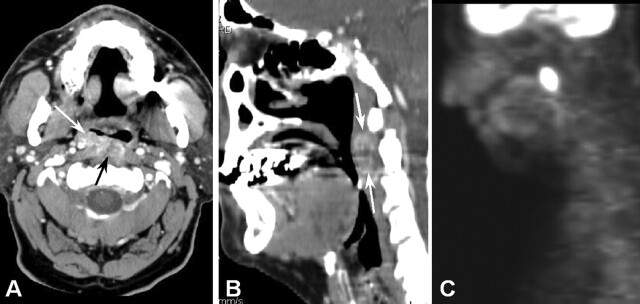
Fig 2.
Presumed pharyngeal Teflon granuloma (case 2).
A, Contrast-enhanced axial CT scan demonstrates an ill-defined mass in the right side of the posterior pharynx (arrows). The mass infiltrates the surrounding soft tissues, particularly the left longus coli muscle.
B, Sagittal reconstruction of the same CT scan clarifies the location of the mass (arrows) and is useful for comparison to sagittal PET findings (C).
C, Sagittal PET scan demonstrates marked FDG uptake in the mass.
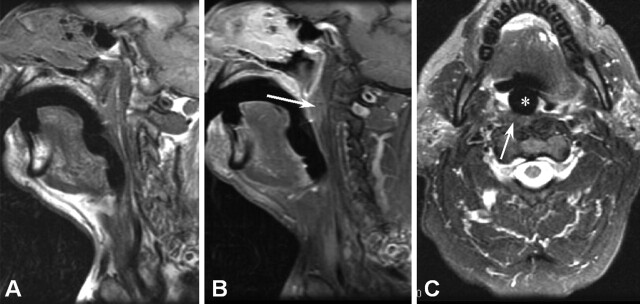
Fig 3.
MR imaging of Teflon granuloma (case 2).
A, Precontrast sagittal T1-weighted image does not demonstrate the pharyngeal mass well.
B, Postcontrast sagittal T1-weighted image demonstrates weak, ill-defined enhancement in the posterior pharyngeal wall (arrows).
C, T2-weighted axial image demonstrates intermediate signal intensity within the mass (arrow), lower than expected for tumor. The patient’s palatal drop prosthesis (asterisk [*]) causes minimal artifact.
The patient came to our institution for a second opinion, and the radiological examinations were reviewed. On the basis of the CT findings of a well-circumscribed mass with inherently high attenuation, and the MR imaging finding of only intermediate T2 signal intensity in the area of suspected tumor, a radiographic diagnosis of Teflon-induced granuloma was made. Short interval follow-up was recommended. The patient returned at 3 months, 6 months, and 1 year for further clinical and radiographic examination. The pharyngeal lesion was deemed stable on the basis of clinical and radiological assessment, supporting the presumptive diagnosis of Teflon-induced granuloma. The patient underwent no further therapy.
Discussion
Velopharyngeal insufficiency is the incomplete closure of one or more structures in the posterior pharynx, resulting in hypernasal speech or the inability to successfully swallow without regurgitation (5). Velopharyngeal insufficiency has several etiologies including congenital abnormalities such as overt and submucosal cleft palate, neuromuscular disease such as myasthenia gravis, iatrogenic following adenoidectomy, and idiopathic decreased muscle tone (6, 7). One of the most problematic symptoms in patients with velopharyngeal insufficiency is hypernasal speech; air escapes through the nose when pronouncing consonants. Another presentation of velopharyngeal insufficiency is persistent dysphagia in patients without a Zenker diverticulum or a history of gastro-esophageal reflux disease. In patients who suffer from a decrease in the muscle tone or bulk in the posterior pharynx as their underlying structural deformity, Teflon injection has been used to supplement tissue and allow for complete closure of the pharyngeal sphincters.
Teflon is an inert, resinous polymer of tetrafluoroethylene. In the early 1980s, liquid Teflon was considered an ideal material to correct certain types of velopharyngeal insufficiency because it is biologically stable and was thought not to change in thickness or migrate in vivo (8). Teflon use in this patient population declined when it was implicated in foreign-body-reactive granulomas. These granulomas were not recognized initially, because they are typically slowly progressive and may be delayed in onset for many years. Current surgical treatments for velopharyngeal insufficiency include palatoplasty or pharyngoplasty, or the injection of autologous collagen or hydroxyapatite to augment the posterior pharynx (9).
The CT appearance of a Teflon granuloma can be easily confused with that of carcinoma. In a Teflon granuloma, the soft-tissue planes are infiltrated with enhancing material (scar). As Figure 1 demonstrates, surrounding bone or cartilage may be eroded (10). Teflon itself is radiographically attenuated, but it may spread through the soft tissues and be mistaken for tumor enhancement or calcification. Ironically, the use of PET or combined PET/CT may increase the suspicion for carcinoma. Granulomas incited by Teflon are intensely FDG-avid and are easily confused with malignancy (11).
A thorough review of the patient’s history is usually sufficient to suggest the possibility of Teflon granuloma, but because of the decreased use of Teflon, clinicians may be less aware of its potential for disease. If Teflon granuloma is suspected, MR imaging can be used to confirm the diagnosis. The fibrous reaction incited by long-standing Teflon injection is generally of low-to-intermediate T2 signal intensity, whereas carcinoma should have increased T2 signal intensity. This was the major finding that allowed us to suggest Teflon granuloma in patient 2.
Conclusion
Teflon injection may have significant foreign-body granulomatous reaction with inflammation and fibrosis. As with other inflammatory processes, this results in increased FDG uptake. The aggressive nature of these lesions may cause bone erosion or invasion of soft tissues. These findings are easily misinterpreted as malignancy on the basis of CT, PET, or combined PET/CT findings. Teflon granulomas are characterized by hyperattenuated, poorly defined masses on unenhanced CT scans, intermediate signal intensity on T2-weighted MR images (less signal intensity than expected for tumor), and avid FDG-PET uptake. A complete clinical history and familiarity with the effects of Telfon injection can help to avoid misdiagnosis of Teflon granuloma.
References
- 1.Fukui MB, Blodgett TM, Meltzer CC. PET/CT imaging in recurrent head and neck cancer. Semin Ultrasound CT MR 2003;24:157–163 [DOI] [PubMed] [Google Scholar]
- 2.Chisin R, Macapinlac HA. The indications of FDG-PET in neck oncology. Radiol Clin North Am 2000;38:999–1012 [DOI] [PubMed] [Google Scholar]
- 3.Beyer T, Townsend DW, Brun T, et al. A combined PET/CT scanner for clinical oncology. J Nucl Med 2000;41:1369–1379 [PubMed] [Google Scholar]
- 4.Malizia AA Jr, Reiman HM, Myers RP, et al. Migration and granulomatous reaction after periurethral injection of polytef (Teflon). JAMA 1984;251:3277–3281 [PubMed] [Google Scholar]
- 5.Johns DF, Rohrich RJ, Awada M. Velopharyngeal incompetence: a guide for clinical evaluation. Plast Reconstr Surg 2003;112:1890–1897 [DOI] [PubMed] [Google Scholar]
- 6.Fernandes DB, Grobbelaar AO, Hudson DA, Lentin R. Velopharyngeal incompetence after adenotonsillectomy in non-cleft patients. Br J Oral Maxillofac Surg 1996;34:364–367 [DOI] [PubMed] [Google Scholar]
- 7.Conley SF, Gosain AK, Marks SM, Larson DL. Identification and assessment of velopharyngeal inadequacy. Am J Otolaryngol 1997;18:38–46 [DOI] [PubMed] [Google Scholar]
- 8.Furlow LT Jr, Williams WN, Eisenbach CR 2nd, Bzoch KR. A long-term study on treating velopharyngeal insufficiency by Telfon injection. Cleft Palate J 1982;19:47–56 [PubMed] [Google Scholar]
- 9.Seagle MB, Mazaheri MK, Kixon-Wood VL, Williams WN. Evaluation and treatment of velopharyngeal insufficiency: the University of Florida experience. Ann Plastic Surg 2002;48:464–70 [DOI] [PubMed] [Google Scholar]
- 10.Smith RM, Goldwasser MS, Sabol SR. Erosion of a Teflon-proplast implant into the middle cranial fossa. J Oral Maxillofac Surg. 1993;51:1268–1271 [DOI] [PubMed] [Google Scholar]
- 11.Yeretsian RA, Blodgett TM, Branstetter BF, et al. Teflon-induced granuloma: a false-positive finding with PET resolved with combined PET and CT. AJNR Am J Neuroradiol 2003;24:1164–1166 [PMC free article] [PubMed] [Google Scholar]