Abstract
Summary: Infiltrating lipoma is an uncommon mesenchymal neoplasm that characteristically infiltrates adjacent tissues and tends to recur after excision. This type of lipoma is extremely rare in the head and neck region. We report a case of a giant infiltrating lipoma of the face, studied with CT and MR imaging.
Lipomas are one of the most common soft-tissue mesenchymal tumors, accounting for approximately 16% of all these neoplasms. They may arise in all parts of the body. Their occurrence in the head and neck, however, is relatively rare (1).
Benign lipomatous tumors have been subclassified according to their histologic features and growth patterns into classic lipoma (solitary or multiple), fibrolipoma, angiolipoma, infiltrating lipoma, intramuscular lipoma, hibernoma, pleomorphic lipoma, lipoblastomatosis, and diffuse lipoblastomatosis. Infiltrating lipoma is an uncommon mesenchymal neoplasm that characteristically infiltrates adjacent tissues and tends to recur after excision. Locations at the limbs is the more frequent, with 50% of cases located in the thigh, 20% in the shoulder region and upper arm, 20% in the chest wall, and 10% in other locations. This type of lipoma is extremely rare in the head and neck region, and its congenital type is rare (2–4). The first two cases of oral infiltrating lipoma were reported by Bennhoff and Wood in 1978 (5).
Few additional cases of oral-facial infiltrating lipomas have been reported in the surgical literature (2, 4–13). We report a case of a giant infiltrating lipoma of the face, studied with CT and MR imaging.
Case Report
A 37-year-old white female patient presented with a 2-year history of slowly progressive swelling of the right cheek and parotidomasseteric and submandibular areas (Fig 1). Clinical examination revealed a painless nontender soft mass with ill-defined borders occupying the low part of parotid and masseteric region, the entire cheek, and a portion of the submandibular region. The mass was firm and fixed, and the overlying skin was normal without signs of discoloration or abnormal vascularization. There was no clinical evidence of enlargement of the cervical nodes. Intraoral examination showed a submucosal swelling and stuffing the lower buccal sulcus, associated with a large bulge of the lateral wall of the oropharynx, on the right side. However, the covering mucosa was normal in color and texture without ulceration or inflammatory signs.
Fig 1.
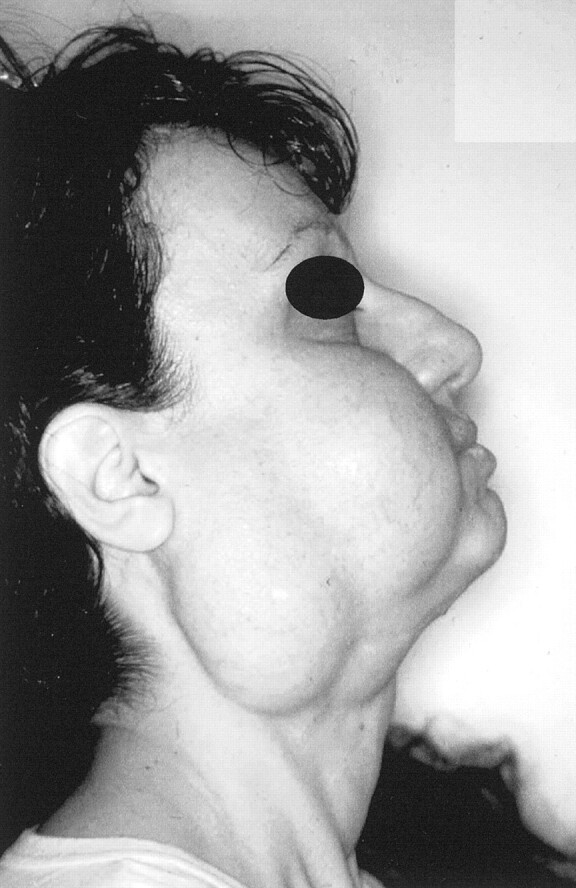
Photograph of a 37-year-old white female patient who presented with a 2-year history of slowly progressive swelling of the right cheek and parotidomasseteric and submandibular areas.
The patient underwent CT of the maxillofacial and neck region with conventional equipment (Somatom HiQ; Siemens, Erlangen, Germany). Axial CT scans, obtained before and after the IV administration of iodinated contrast medium, showed an expansive ill-defined mass occupying the parotidomasseteric region (the parotid gland was compressed and posteriorly displaced), infraorbital area, pterygopalatine fossa, and submandibular area and extending deeply toward the right parapharyngeal space (Fig 2). The airway at that level was narrowed and displaced to the left.
Fig 2.
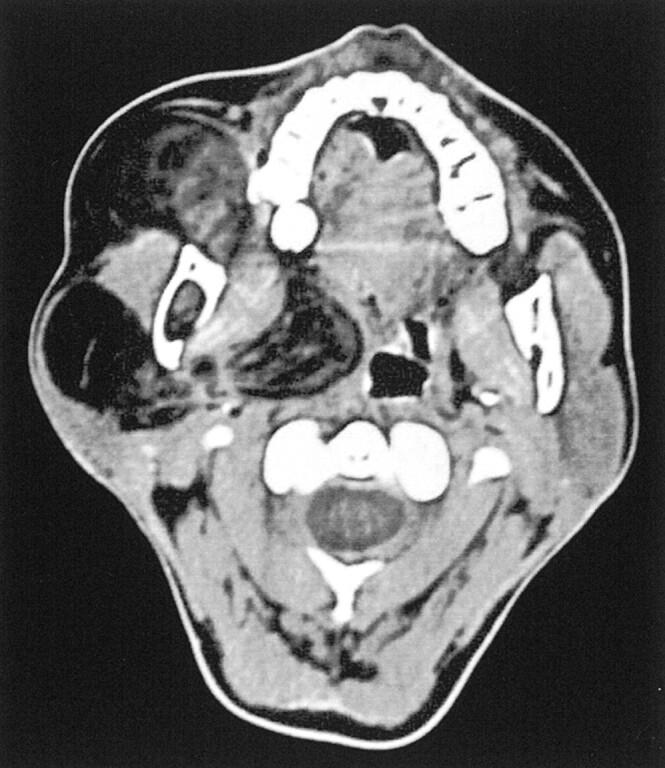
Axial contrast-enhanced CT scan shows an expansive, ill-defined, inhomogeneously hypoattenuated mass occupying the parotidomasseteric region and extending deeply toward the right parapharyngeal space. The parotid gland is compressed and displaced posteriorly. No contrast enhancement is evident. Linear densities within the lipomatous region are consistent with fibrous materials revealed by histologic examination.
The lesion appeared as large areas of wide hypoattenuation, similar to adipose structures, intersected by irregular bands of relative hyperattenuation. Contrast enhancement was not evident, nor was it evident in the lipomatous areas or the intersecting linear region. No calcification was observed within the mass, and no signs of bone erosion were identified.
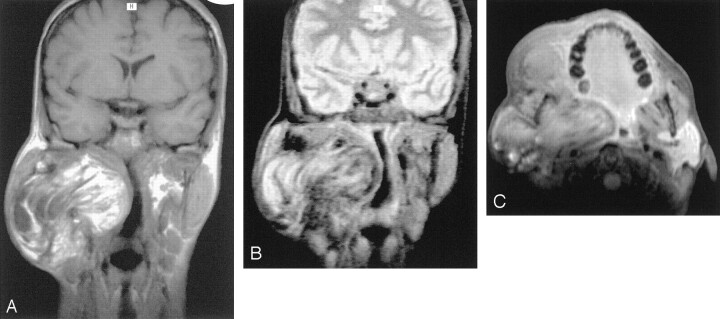
The patient underwent MR imaging with a 1.0-T superconductive imaging unit (Magnetom SP 42 E, Siemens). Spin-echo T1-weighted images were obtained in the axial, coronal, and sagittal planes (450/10 [TR/TE]) before and after the IV administration of contrast medium. Spin-echo fat-suppressed T1-weighted images with selective chemical shift cut (900/22) and axial view spin-echo DP-T2-weighted sequences (2000/13, 80 [TR/TE, second TE]) were obtained.
The lesion had inhomogeneous high signal intensity on T1-weighted images (Fig 3A), with moderate decreased signal intensity on T2-weighted images (Fig 3B). Irregular linear regions of hypointensity also were present. Fat-suppressed T1-weighted images showed a partial suppression of the lesion, consistent with fat (Fig 3C). The lesion showed ill-defined margins without a clear plane of cleavage between the mass and the adjacent muscular structures, especially pterygoid and masseter muscles that appeared displaced and compressed.
Fig 3.
MR images obtained with a 1.0-T superconductive imaging unit.
A, Coronal spin-echo T1-weighted MR image (512/17) shows an inhomogeneous hyperintense lesion located in the parotidomasseteric region and extending deeply toward the parapharyngeal space.
B, On spin-echo T2-weighted MR image without fat suppression (2300/80), decreasing signal intensity is appreciable and irregular linear regions of markedly hypointense signal are present.
C, Axial contrast-enhanced fat-suppressed spin-echo T1-weighted MR image (900/22) shows partial suppression of the lesion, consistent with fat. The lesion nevertheless shows ill-defined margins without a clear plane of cleavage between the mass and the adjacent muscular structures, especially the pterygoid and masseter muscles that appeared displaced and compressed. No evidence of contrast enhancement within the mass can be seen.
Surgical treatment was instituted, via a posterolateral transmandibular approach. The mass had a fatty yellow appearance and lacked a defined capsule. The posterior part of the lesion, deeply expanding toward the parapharyngeal space, was firmly attached to the surrounding muscles and the ramus of mandible. The cheek appeared diffusely infiltrated, up to the cutaneous planes. Complete excision was performed, preserving the parotid and submandibular gland and facial nerve (Fig 4).
Fig 4.
Photograph of surgical specimen. Removal of the mass was difficult, because the posterior part of the lesion was firmly attached to the surrounding muscles and the ramus of mandible. The gross appearance of the mass is that of an irregular, lobulated, firm fatty lesion with no evidence of encapsulation.
Pathologic examination revealed a lipomatous lesion with intersecting fibrous bands. The lesion was devoid of a capsule and comprised uniform-appearing mature adipocytes; some sections revealed the presence of myxoid hypocellular areas and inflammatory cell infiltration, with prevalence of lymphocytes. Diffuse infiltration of entrapped striated muscles was seen; lipoblasts, cellular atypism, or mitoses indicating liposarcoma were not identified (Fig 5). The 15-month follow-up studies revealed no recurrence.
Fig 5.
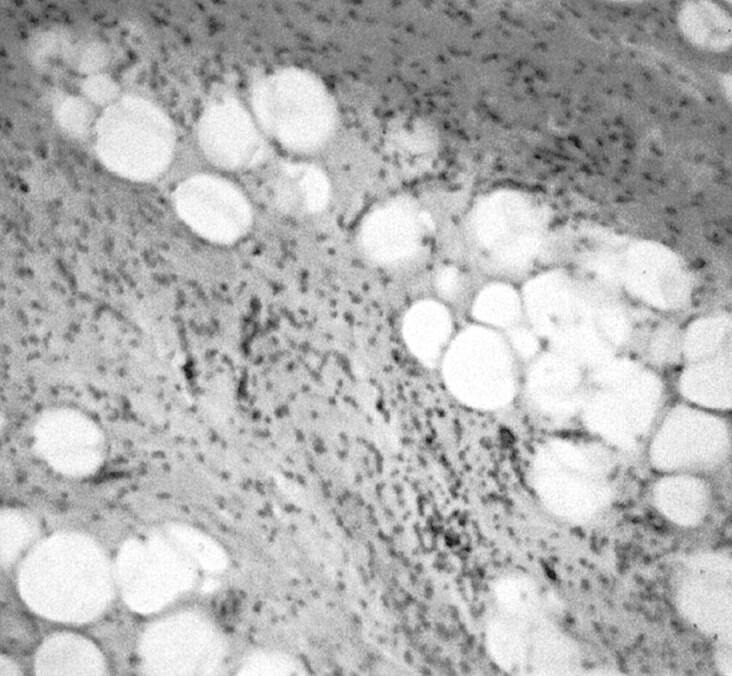
Pathologic specimen (hematoxylin and eosin; original magnification, ×400). The lesion is composed of uniform-appearing mature adipocytes, with the presence of myxoid hypocellular areas and infiltrates of inflammatory cells, especially lymphocytes. Diffuse infiltration of entrapped striated muscles can be seen; no evidence of lipoblasts, cellular atypism, or mitoses indicating liposarcoma is seen.
Discussion
Only approximately 25% of lipomas and their variants arise in the head and neck region (1), most commonly in the subcutaneous posterior neck (14). They also develop rarely in the anterior neck, infratemporal fossa, in or around the oral cavity (15, 16), larynx (17, 18), tonsillar area (19), parotid area (20), hypopharynx (21), nasopharynx (22), and retropharyngeal space (23).
Lipoma is a benign subcutaneous and submucosal tumor and usually is of little clinical concern. Most lipomas tend to grow insidiously large without any symptoms and cause few problems other than those of a localized mass and cosmetic concerns (15, 23). Typically, these tumors are well circumscribed, are encapsulated (often by a fibrous shell), tend to be smooth or lobulated, are easy to remove, and rarely recur. Lipomas are well vascularized, but the vascular network often is compressed by the distended lipocyte (24).
Occasionally, the lipoma may invade muscles or grow between them: the so-called infiltrating lipoma. The first convincing report of infiltrating benign lipoma was by Hoffman in 1941, but it was Regan who defined this entity in 1946. This lipomatous lesion is an uncommon neoplasm, usually appearing in a subcutaneous location in the extremities or trunk (10). Unlike the lipoma, it is not encapsulated, extensively involving the deep soft tissues, muscle, nerve, or synovium (2). The high rate of recurrence (≤60% of the reported head and neck cases) (25) is perhaps attributable to the difficulties in radical excision; no case of infiltrating lipoma undergoing malignant changes has been reported in the literature (10). Two varieties of deep-seated infiltrating lipomatous lesions have been described: lipoma (the present case) and angiolipoma. Angiolipoma is characterized by prominent vascular components, whereas infiltrating lipoma is composed of mature adipose cells, inconspicuous blood vessels, and delicate strands of connective tissue (2, 26).
Oral infiltrating lipoma may occur in any soft areas, but the cheek and tongue account for approximately half of reported cases (5, 7–9, 11–13). These lesions seem to be larger than ordinary oral lipomas and are generally painless masses that cause swelling and deformity (2).
Imaging evaluation of soft-tissue tumors has undergone a dramatic evolution with the advent of CT and MR imaging, which are very useful for definite differential diagnosis (27). Comprised of mature adipose tissue, classic lipomas have CT and MR imaging signal intensity characteristics similar to those of subcutaneous fat. The deep lesions tend to be variable in shape, likely because they tend to model themselves on the surrounding structures (28).
On CT scans, lipomas appear as homogeneous hypoattenuated masses (apart from the thin and wispy soft-tissue attenuated septa, although, on occasion, septa may be thick and nodular). They have a CT number ranging from −60 to −120 HU and do not typically show contrast enhancement. In some cases, centrally enhanced areas, corresponding to lipomatous lesions with inflammatory cell infiltration, have been identified (23).
On MR images, fat has a typical signal intensity. On T1-weighted images, lipomas tend to have high signal intensity that diminishes with progressive T2 weighting. Fat is also suppressed with the use of fat-suppression pulses.
MR imaging provides better tumor delineation because it has superior soft-tissue contrast resolution and clear definition of the location and longitudinal extent of the mass. Multiplanar capability, moreover, clearly shows planes of cleavage between the lipoma, muscle, and vessels. It is particularly important in the oral-facial region where the margins of lipoma are commonly ill defined, because these lesions often are surrounded by normal fat tissue and have a very thin capsule (15). IV administration of contrast medium better depicts the tumor margins and can detect irregular vascularization when sarcomatous degeneration is considered (15, 28).
Most lipomatous lesions do not present any particular diagnostic problems; nevertheless, a group of fatty tumors, including infiltrating lipoma, pleomorphic lipoma, spindle cell lipoma, and lipoblastoma, may cause considerable diagnostic difficulties and may be mistaken for liposarcoma (2). The appearance of tumor margins, the signal intensity homogeneity, the size, the peritumoral signal intensity, the apparent neurovascular bundle encasement or displacement, and the bone invasion are not always reliable features that differentiate benign from malignant masses, especially from well-differentiated liposarcomas (29). These tumors, containing a large amount of fat, usually >75% of their volume, resemble lipomas on both CT scans and MR images but present internal septa that may be broader and more nodular than those seen in lipomas. Thorough pathologic examination may be required to establish the diagnosis. In the reported case of giant infiltrating lipoma, some CT and MR imaging features (thin internal septa, no contrast enhancement, partial but homogeneous suppressed signal intensity of lesion, in fat-suppressed pulse sequences) were indicative of the benign nature of the mass. Myxoid liposarcomas, the most common variety of liposarcoma, and especially pleomorphic or round cell or dedifferentiated liposarcomas, contain little or no fat. Consequently, the imaging features can be easily differentiated from those of fatty benign lesions but not from those of many types of soft-tissue sarcoma.
Conclusion
In cases of infiltrating lipomas, complete surgical excision is mandatory because of the infiltrative nature and potentially high rate of recurrence after inadequate surgery (2). Because of the rarity of these lipomatous lesions of the head and neck region and, to our knowledge, the paucity of published analogous cases in the radiologic literature, we are reporting an additional case of infiltrating lipoma of the head region, with particular consideration of CT and MR imaging features.
References
- 1.Kransdorf MJ. Benign soft-tissue tumors in a large referral population: distribution of specific diagnoses by age, sex, and location. AJR Am J Roentgenol 1995;164:395–402 [DOI] [PubMed] [Google Scholar]
- 2.Piattelli A, Fioroni M, Rubini C. Intramuscular lipoma of the cheek: a case report. J Oral Maxillofac Surg 2000;58:817–819 [DOI] [PubMed] [Google Scholar]
- 3.Lacey MS, Craig I. Infiltrating lipoma of the face. Ann Plast Surg 1995;35:307–309 [DOI] [PubMed] [Google Scholar]
- 4.Pelissier A, Sawaf MH, Shabana AM. Infiltrating (intramuscular) benign lipoma of the head and neck. J Oral Maxillofac Surg 1991;49:1231–1236 [DOI] [PubMed] [Google Scholar]
- 5.Bennhoff DF, Wood JW. Infiltrating lipomata of the head and neck. Laryngoscope 1978;88:839–848 [DOI] [PubMed] [Google Scholar]
- 6.Scherl MP, Som PM, Biller HF, Shah K. Recurrent infiltrating lipoma of the head and neck: case report and literature review. Arch Otolaryngol Head Neck Surg 1986;112:1210–1212 [DOI] [PubMed] [Google Scholar]
- 7.Garavaglia J, Gnepp DR. Intramuscular (infiltrating) lipoma of the tongue. Oral Surg Oral Med Oral Pathol 1987;63:348–350 [DOI] [PubMed] [Google Scholar]
- 8.Takeda Y. Intramuscular lipoma of the tongue. Ann Dent 1989;48:22–24 [PubMed] [Google Scholar]
- 9.Shirasuna K, Saka M, Watatani K, Kogo M, Matsuya T. Infiltrating lipoma of the tongue. Int J Oral Maxillofac Surg 1989;18:68–69 [DOI] [PubMed] [Google Scholar]
- 10.Ayasaka N, Chino T Jr, Chino T, Antoh M, Kawakami T. Infiltrating lipoma of the mental region: report of a case. Br J Oral Maxillofac Surg 1993;31:388–390 [DOI] [PubMed] [Google Scholar]
- 11.Bataineh AB, Mansour MJ, Abalkhail A. Oral infiltrating lipomas. Br J Oral Maxillofac Surg 1996;31:520–523 [DOI] [PubMed] [Google Scholar]
- 12.Epivatianos A, Markopoulos AK, Papanayotou P. Benign tumors of adipose tissue of the oral cavity: a clinicopathologic study of 13 cases. J Oral Maxillofac Surg 2000;58:1113–1117 [DOI] [PubMed] [Google Scholar]
- 13.Ergün SS, Kurul S, Ulay M, BilgiÇ B. Infiltrating lipomatosis of the face. Ann Plast Surg 2001;47:346–348 [DOI] [PubMed] [Google Scholar]
- 14.Som PM, Scherl MP, Rao VM, Biller HF. Rare presentations of ordinary lipomas of the head and neck: a review. AJNR Am J Neuroradiol 1986;7:657–664 [PMC free article] [PubMed] [Google Scholar]
- 15.Abdullah BJ, Liam CK, Kaur H, Mathew KM. Parapharyngeal space lipoma causing sleep apnoea. Br J Radiol 1997;70:1063–1065 [DOI] [PubMed] [Google Scholar]
- 16.Ghandour K, Issa M. Lipoma of the floor of the mouth. Oral Surg Oral Med Oral Pathol 1992;73:59–60 [DOI] [PubMed] [Google Scholar]
- 17.Yoskovitch A, Cambronero E, Said S, Whiteman M, Goodwin WJ. Giant lipoma of the larynx: a case report and literature review. Ear Nose Throat J 1999;78:122–125 [PubMed] [Google Scholar]
- 18.Cauchois R, Laccourreye O, Rotenberg M, Carnot F, Menard M, Brasnu D. Intrinsic infiltrating intramuscular laryngeal lipoma. Otolaryngol Head Neck Surg 1995;112:777–779 [DOI] [PubMed] [Google Scholar]
- 19.Benson-Mitchell R, Tolley N, Croft CB, Roberts D. Lipoma of the left tonsillar fossa. J Laryngol Otol 1994;108:507–508 [DOI] [PubMed] [Google Scholar]
- 20.Fasig JH, Robinson RA, McCulloch TM, Fletcher MS, Miller CK. Spindle cell lipoma of the parotid: fine-needle aspiration and histologic findings. Arch Pathol Lab Med 2001;125:820–821 [DOI] [PubMed] [Google Scholar]
- 21.Eckel HE, Jungehulsing M. Lipoma of the hypopharynx: pre-operative diagnosis and transoral resection. J Laryngol Otol 1994;108:174–177 [DOI] [PubMed] [Google Scholar]
- 22.Chaudhry S, Sirpal YM. Lipoma: a rare tumour of nasopharyx. Indian J Cancer 1997;34:177–178 [PubMed] [Google Scholar]
- 23.Yoshihara T, Kawano K, Mita N. Retropharyngeal lipoma causing severe dysphagia and dyspnea. J Otolaryngol 1998;27:363–366 [PubMed] [Google Scholar]
- 24.Enzinger FM, Weiss SW. Benign lipomatous tumors. In: Enzinger FM, Weiss SW, eds. Soft Tissue Tumors. 2nd ed. St. Louis: Mosby;1988. :301–345
- 25.Dionne GP, Seemayer TA. Infiltrating lipomas and angiolipoma revisited. Cancer 1974;33:732–738 [DOI] [PubMed] [Google Scholar]
- 26.Sugiura J, Fujiwara K, Kurahashi I, Kimura Y. Infiltrating angiolipoma of the mucolabial fold: a case report and review of the literature. J Oral Maxillofac Surg 1999;57:446–448 [DOI] [PubMed] [Google Scholar]
- 27.Cappabianca S, Iscaro FM, Sirignano C, et al. The identification of the criteria of malignancy and the tissue characterization of expansive processes in periskeletal soft tissues: the current role of magnetic resonance [in Italian]. Radiol Med (Torino) 1999;98:127–132 [PubMed] [Google Scholar]
- 28.Munk PL, Lee MJ, Janzen DL, et al. Lipoma and liposarcoma: evaluation using CT and MR imaging. AJR Am J Roentgenol 1997;169:589–594 [DOI] [PubMed] [Google Scholar]
- 29.Crim JR, Seeger LL, Yao L, Chandnani V, Eckardt JJ. Diagnosis of soft-tissue masses with MR imaging: can benign masses be differentiated from malignant ones? Radiology 1992;185:581–586 [DOI] [PubMed] [Google Scholar]