Abstract
Summary: When evaluating vascular supply, a combined angiography and CT (angio-CT) system provides more accurate vascular anatomy than digital subtraction angiography. To the best of our knowledge, however, the application for intracranial tumors has not been described. We herein describe a technique of an angio-CT system for diagnosis of vascular anatomy of the feeding artery for preoperative embolization of meningeal tumors.
The usefulness of a combined angiography and CT (angio-CT) system for interventional procedures has been applied to abdominal, thoracic, and intracranial regions (1–4). To the best of our knowledge, however, no systematic studies have evaluated the utility of an angio-CT system for meningeal tumors. Knowledge of the precise vascular anatomy of the tumor-feeding artery with angio-CT may predict complications induced by infusion of embolic material into the normal tissues including the brain. The purpose of this study was to describe the technique of an angio-CT system for diagnosis of vascular anatomy of the feeding artery and to present its utility for preoperative embolization of meningeal tumors.
Patients and Techniques
Between February 1999 and May 2001, nine consecutive patients (eight women and one man, 49–84 years of age [mean, 67 years]) with meningiomas (n=8) or meningeal malignant lymphomas (n=1) underwent intraarterial digital subtraction angiography (DSA) and combined angiography and CT (angio-CT) examinations by using an angio-CT system (DFA-100 and W3000 AD; Hitachi, Tokyo, Japan). The angio-CT system allows movement of the patient in and out the two imaging units, on the same table. The time necessary to switch between examinations is a few minutes.
The tumors ranged from 20 to 75 mm in diameter. The tumors were located at the convexity in three, parasagittal in two, sphenoid ridge in two, and posterior fossa in two. One meningioma was recurrent after surgery. One patient with neurofibromatosis type 2 had three meningiomas in the convexity. All patients underwent surgical resection after embolization. Preoperative embolization was intended to prevent intraoperative blood loss. Informed consent was obtained from the patients or their relatives.
Intraarterial DSA was performed by using a 1024 × 1024 matrix with a DSA unit (DFA-100; Hitachi, Tokyo, Japan). All catheterizations were performed via a transfemoral approach by the Seldinger technique. In all patients, immediately after the insertion of the vascular sheath, 5000 U of heparin was injected transvenously to prevent thromboembolic complications related to the catheter placement. The angiographic procedure was routinely accomplished by using a standard diagnostic catheter (diameter 5F). Coaxial technique was used by placing a 2.7F microcatheter (Fastracker-18 catheter, Target Therapeutics, San Jose, CA) in the appropriate feeding artery. Continuous perfusion of saline was used between coaxial catheters. After an external carotid arterial DSA study, the tip of the catheter was placed at the proximal portion of the feeding artery, and superselective DSA and angio-CT were performed. For the superselective biplane DSA studies, a total of 4.0–6.0 mL of nonionic contrast material (Iopamiron 300 [300 mg I/mL]; Schering, Osaka, Japan) was injected through the catheter at a rate of 1.0–1.5 mL/s by using a power injector (Auto Enhance A-50; Nemoto Kyorindo, Tokyo, Japan). When parasitic supply from the internal carotid or vertebrobasilar arterial territories was suspected, biplane internal carotid or vertebrobasilar angiograms were obtained with a power injection of 6.0 mL of contrast material at a rate of 4.0 mL/s.
After the superselective DSA, angio-CT was performed with an injection of 3–15 mL of the same nonionic contrast material without dilution, through the catheter at an injection rate of 0.3–1.0 mL/s by using another power injector. The injection rate and dose were determined by the size of the selected artery and the scanning time. During the injection from the meningeal artery supplying the tumor, helical CT scans were performed in 1-second acquisition times, a 7-mm section thickness, a table speed of 1.2 mm/s (250 mAs; 120 kV), and a 512 × 512 matrix. The CT scanning was started at the proximal level of the selected artery and ended at the upper level of the tumor. When parasitic supply from the internal carotid or vertebrobasilar arterial territories was suspected, angio-CT was performed at the tumor site, with the same scanning conditions. A total of 10–20 mL of the same nonionic contrast material was injected at an injection rate of 1.0–2.0 mL/s.
When embolization was performed, the position of the tip of the catheter was determined according to the findings of DSA and angio-CT. The additional findings based on angio-CT to DSA were interpreted in consensus by two radiologists (T.H., K.O.).
Results
A total of 16 angio-CT examinations for 11 tumors were performed. Additional time required for the combined examination as compared with DSA alone was less than 10 minutes in all patients. The selected arteries for 16 examinations included the middle meningeal artery (n=10), internal carotid artery (n = 4), accessory meningeal artery (n=1), and occipital artery (n=1). All feeders of the external carotid arteries were successfully embolized, and no complications related to the interventions were observed in any patients.
In the evaluation of vascular supply within the tumor for each feeding artery, additional information was present in four cases. In one case, complicated vascular supply within the tumor with the mulifeeders was more clearly identified with angio-CT. In one, meningeal supply was more definitely delineated because the tumor had hypovascularity at DSA. Parasitic supply from the internal carotid arterial territory was seen in four cases. In three of four cases with parasitic supply, only angio-CT depicted it in one and more clearly demonstrated it than DSA in two.
With regard to the vascular supply to the normal tissues, four unexpected branches or stains derived from the feeding artery were identified at DSA. In one meningoophthalmic artery, the retinal vascular supply was identified on both images: retinal blush at DSA and retinal enhancement at angio-CT. In one meningoophthalmic branch of the middle meningeal artery, only angio-CT revealed vascular supply to the lacrimal gland (Fig 1). In stains from the accessory meningeal artery, only angio-CT images demonstrated vascular supply to the lateral pterygoid muscle (Fig 2). According to the finding of angio-CT, the tip of the catheter was advanced more distally to prevent unnecessary infusion of the embolic materials to the muscles.
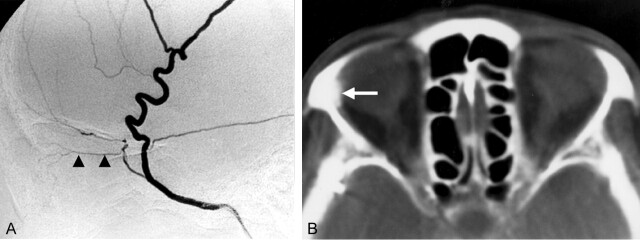
Fig 1.
A 64-year-old female patient with convexity meningioma.
A, Superselective angiogram of the right middle meningeal artery shows a small ophthalmic branch derived from the middle meningeal artery (arrowheads).
B, Angio-CT image from the same selected artery shows definite enhancement of the lacrimal gland (arrow). The wall of the right eye ball including the retina does not enhance.
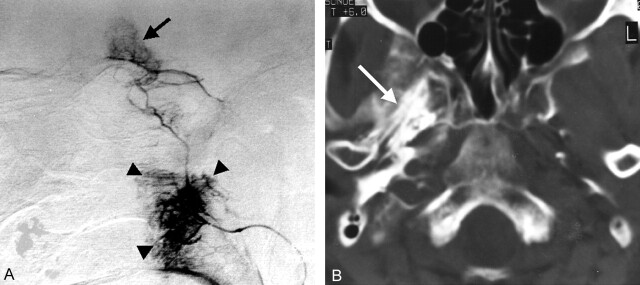
Fig 2.
A 60-year-old female patient with right sphenoid ridge meningioma.
A, Lateral superselective angiogram of the right accessory meningeal artery shows a stain of the tumor (arrow). A remarkable stain (arrowheads) is observed at the level of the proximal portion of the feeding artery.
B, Angio-CT image at the level of the proximal portion of the feeding artery shows marked enhancement of the lateral pterigoid muscle (arrow). Because angio-CT definitely showed blood supply to the masticatory muscle, the tip of the catheter was advanced more distally to prevent the muscle injury.
Discussion
Angio-CT has several advantages over DSA: having higher contrast and spatial resolutions and providing more anatomic detail by continuous two-dimensional images. In our study, angio-CT provided more definite visualization of tumor perfusion than DSA in nearly half of the cases. In one meningioma with multiple feeders, angio-CT provided more definite information of vascular supply for each feeder than DSA. This information may be useful for precise understanding of vascular territory of each feeder. Parasitic supply from the internal carotid arterial territory was more clearly identified with angio-CT in three of four cases. The findings may be valuable for the estimation of bleeding volume and site in surgical resection.
Several conditions added by angio-CT examinations are as follows. First, additional time required for the combined examination as compared with a DSA alone was less than 10 minutes. We believe that the added time is acceptable for routine interventional procedures. Second, the added radiation dose by the angio-CT is considered to be small because the section thickness was 7 mm and the extent of CT scanning was limited. The added dose for angio-CT may be less than that for conventional brain CT. Third, the added volume of contrast material was 3–20 mL. The volume is compatible with that of one to two DSA examinations. Fourth, the additional cost of the angio-CT is that of the added CT examination and the contrast material used.
Among the complications of external carotid artery embolization of a tumor, major concerns include devascularization of normal tissues such as the cranial nerve, eye, muscle, and skin and passage of embolic materials through anastomoses to produce ischemic damage of the brain (5–8). Use of angio-CT system for the external carotid artery embolization might be useful for preventing the complications related to preoperative embolization of meningeal tumors. The angio-CT system might also provide valuable information in following situations: chemoembolization of parenchymal tumors and embolization of the intracranial or extracranial arteriovenous malformation adjacent to functionally important structures.
In our study, angio-CT identified specific tissues fed by an unexpected branch that could not be completely understood by using DSA alone. In one case, angio-CT definitely showed vascular supply to the masticatory muscle, and we cautiously repositioned the tip of the catheter more distally. Although it was not known whether muscle injuries such as trismus could occur by infusion of embolic materials, the specific knowledge may be valuable in the following situations: first, embolization of the dangerous branches such as the ophthalmic branch could be avoided, because angio-CT would demonstrate definite enhancement of the retina; second, when catheterization into the distal portion of a feeding artery is difficult in spite of an unexpected branch of the feeding artery, angio-CT may provide specific information about the tissues fed by the unexpected branch and possible complication from devascularization of the tissues.
Conclusion
Angio-CT was able to provide information in addition to that provided by DSA when evaluating vascular supply to the tumor and/or the normal tissues for each feeding artery before embolization of meningeal tumors. This technique may also be applied to other types of interventional procedures such as chemoembolization of parenchymal tumors and embolization of vascular malformation. Further studies with larger series are needed to investigate the value of angio-CT. Section thickness of angio-CT used was relatively large for evaluation of small structures. Thinner sections obtained by multidetector CT may further increase the vertical resolution of this technique and provide more detailed information about the cross-sectional anatomy.
References
- 1.Görich J, Rilinger J, Sokiranski R, et al. CT-guided intraarterial chemotherapy in locally advanced tumors. Radiology 1996;199:567–570 [DOI] [PubMed] [Google Scholar]
- 2.Moteki T, Ohya N, Katsuya T. Bronchial arterial angio-CT: evaluation of intradural and oesophageal enhancement before bronchial arterial infusion. Br J Radiol 1998;71:834–839 [DOI] [PubMed] [Google Scholar]
- 3.Hirai T, Korogi Y, Ono K, et al. Intraarterial chemotherapy or chemoembolization for locally advanced and/or recurrent hepatic tumors: evaluation of the feeding artery with an interventional CT system. Cardiovasc Intervent Radiol 2001;24:176–179 [DOI] [PubMed] [Google Scholar]
- 4.Hirai T, Korogi Y, Ono K, et al. Preoperative evaluation of intracranial aneurysms: usefulness of intraarterial 3D CT angiography and conventional angiography with a combined unit-initial experience. Radiology 2001;220:499–505 [DOI] [PubMed] [Google Scholar]
- 5.Manelfe C, Lasjaunias P, Ruscalleda J. Preoperative embolization of intracranial meningiomas. AJNR Am J Neuroradiol 1986;7:963–972 [PMC free article] [PubMed] [Google Scholar]
- 6.Latchaw RE. Preoperative intracranial meningioma embolization: technical considerations affecting the risk-to-benefit ratio. AJNR Am J Neuroradiol 1993;14:583–586 [PMC free article] [PubMed] [Google Scholar]
- 7.Hu WY, TerBrugge KG. The role of angiography in the evaluation of vascular and neoplastic disease in the external carotid circulation. Neuroimag Clin North Am 1996;6:625–644 [PubMed] [Google Scholar]
- 8.Lasjaunias P, Berenstein A. Surgical Neuroangiography. Vol II. EndovascularTreatment of Craniofacial Lesions. 1st ed. New York: Springer-Verlag;1987. :57–99