Abstract
BACKGROUND AND PURPOSE: This study was designed to investigate the safety and efficacy of the Onyx liquid embolic system in treating a selected population of patients with intracranial aneurysms that presented difficulties for surgical or endovascular alternatives.
METHODS: A prospective observational study was conducted in 20 European centers enrolling a consecutive series of 119 patients with 123 aneurysms judged suitable for Onyx treatment. The series consists of findings collected in 97 of 119 patients with 100 of 123 aneurysms, because one center declined to provide data to the study sponsor or allow outside audit. Clinical and angiographic outcomes were recorded at discharge, 3 months, and 12 months. All adverse events and re-treatments were recorded. Seventy-nine aneurysms were large or giant.
RESULTS: Twelve-month follow-up angiography findings were available for 71 aneurysms. This angiographic follow-up showed complete occlusion in 56 (79%) aneurysms, subtotal occlusion in nine (13%), and incomplete occlusion in six (8%). Procedure- or device-related permanent neurologic morbidity at final follow-up was present in eight of 97 patients. Seven patients died: two deaths were procedure related; one, disease related; and four, unrelated causes. Seventy-five of the 82 patients alive and with follow-up at 12 months were at Rankin 2 or better status. Delayed occlusion of the parent vessel occurred in nine patients; delayed occlusion was asymptomatic in five and resulted in permanent neurologic deficit in two.
CONCLUSION: In selected patients with aneurysms that are unsuitable for coil treatment or in whom previous treatment has failed to occlude the aneurysm, Onyx treatment offers an endovascular alternative. Aneurysm occlusion rates are superior to reported rates of coil occlusion, and treatment morbidity is comparable to that of published prospective data on endovascular results for this subgroup of patients.
Onyx (Micro Therapeutics, Inc., Irvine, CA) is a liquid embolic material designed for endovascular use. It is an ethylene vinyl alcohol copolymer dissolved in the organic solvent dimethyl sulfoxide (DMSO). When the material comes into contact with an aqueous solution, it precipitates and forms a soft spongy polymer cast, initially with an outer layer, remaining semi-liquid centrally. As further material is injected into the cast, it fills the space into which it is injected, then additional material breaks out through the outer layer of the existing cast. In 1989, Taki et al (1) were the first to report on the use of a similar material (ethylene vinyl alcohol [EVAL]) in the treatment of brain vascular malformations. Onyx formulation subsequently underwent extensive preclinical testing for embolization in brain and other arteriovenous malformations and over the past 5 years has been adopted in clinical use in Europe (2–5).
In the treatment of intracranial aneurysms, the material, as currently used, is constrained by the placement of a balloon over the neck of the aneurysm. The material solidifies completely over a period of about 10 minutes with diffusion of the solvent DMSO. The application of the material to the treatment of intracranial aneurysms has been developed following experimental work (6), and clinical use was initiated in 1999 (7).
We report on the use of and results obtained by the Onyx system in a consecutive series of patients enrolled at study centers before and after European device approval (CE marking), in a case registry known as the Cerebral Aneurysm Multicenter European Onyx (CAMEO) trial. This study continued following device approval with further extension of the use of the device to new physicians. All physicians received laboratory training in the use of the material, and proctoring by a physician experienced in its use, for at least their first two cases, with a clinical specialist present for at least the next three cases. The objective of the study was to determine the safety and efficacy of the material in treating difficult intracranial aneurysms.
Methods
This prospective study is a consecutive series of patients with aneurysms treated by the Onyx system since its introduction at 21 European centers. The study enrolled 119 patients with 123 aneurysms. We were able to report on only 97 patients with 100 aneurysms, because one center declined to provide data to the sponsor or permit outside audit. The material received CE Marking in November 2000. The centers agreed to contribute data to the central registry of cases held by the company. Ethics committee approval (before CE Marking) and informed patient consent to the procedure and data collection were obtained. The data were audited by an independent clinical research organization. Baseline data were collected before the procedure, at the time of the procedure, at discharge, at 3-month follow-up, and at 12-month follow-up. Clinical data were collated and recorded on specifically designed case record forms, which included the collection of Glasgow outcome score, modified Rankin scale, cranial nerve deficits, any adverse events, and any change from baseline neurologic status, including cranial nerve palsies. It was recorded whether morbidity or mortality was device related, procedure related, disease related, or unrelated to the procedure.
Adverse events were defined as any clinical deviation from the patient’s baseline health. These sequelae were categorized as disease related, procedure related when judged as part of the procedure (eg, groin complications), device related when judged to be specific to the device, or of unrelated or unknown cause. Severity was categorized as mild, moderate, or severe or serious. A strict clinical trial and regulatory definition of conditions were used to define serious adverse outcomes: fatal or life-threatening state, persistent or significant disability; intervention necessitated to prevent permanent impairment or damage; or congenital anomaly, cancer, readmission, or prolongation of hospitalization.
All adverse events that occurred during the study period are included. The clinical results in relation to mass effect were recorded to determine whether the symptoms improved, remained the same, or worsened. Angiographic data were collected and forwarded to a core lab for independent assessment. Degree of occlusion was assessed both locally and at the core lab. Patients who reached 1 year after the last Onyx treatment or who refused further follow-up were deemed to have completed the study protocol.
Patient Selection
Patients in the study were selected on the basis of having an aneurysm that 1) was likely to be difficult to treat or presented high risk for conventional coil techniques or neurosurgical clip placement, 2) had recurred following previous coil embolization, or 3) had failed to respond to prior surgical or endovascular treatment.
The cases were initially selected by the treating physician for use of Onyx and were reviewed with a proctor (physician experienced in the use of Onyx). Both the treating physician and the proctor had to agree that Onyx treatment was appropriate. For experienced physicians who had performed more than five cases with the device, the indications were determined at the discretion of the physician.
As part of the evaluation for the use of Onyx during the procedure, a seal test was performed to determine whether the neck of the aneurysm could be satisfactorily occluded bythe balloon. A gentle injection of contrast material was made into the aneurysm via the microcatheter with the balloon inflated; stasis of contrast material was seen when the aneurysm neck could be controlled without significant leakage (Fig 1A and B). This also ensured that no adjacent side branches filled. If adequate control of the aneurysm neck could not be obtained with the balloon, the Onyx treatment was not used. In some circumstances of paraophthalmic artery aneurysms, some filling of the ophthalmic artery was accepted during the seal test at the discretion of the treating physician.
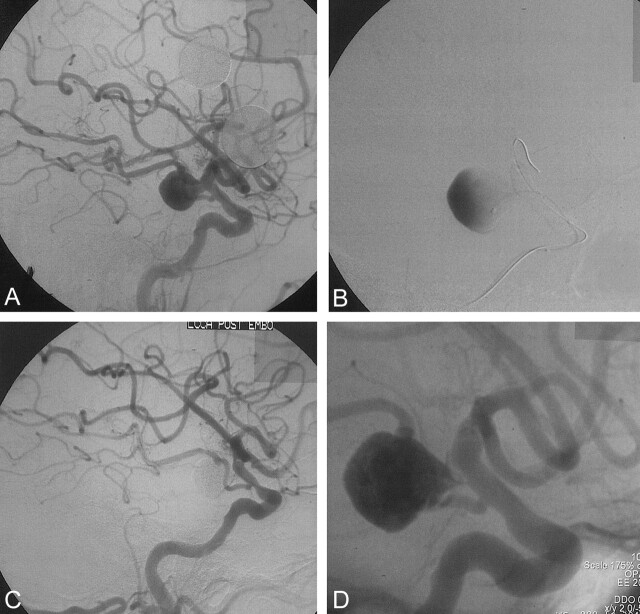
Fig 1.
60-year-old male patient who presented with headache and in whom a large unruptured internal carotid aneurysm was found. Pretreatment, treatment, and follow-up images are presented.
A, Large internal carotid aneurysm before treatment.
B, Seal test before treatment of the aneurysm with Onyx. Microcatheter and balloon are in place with gentle contrast material injection into the aneurysm
C, Angiographic result immediately after Onyx treatment.
D, Follow-up angiogram 6 months after treatment, showing complete occlusion and intervening soft thickened tissue between vessel lumen and Onyx cast in the aneurysm
The range of balloons available for this procedure evolved during the period of the study. Initially only 4 × 15-mm balloons were available on a nonbraided shaft (Equinox; Microtherapeutics, Inc.). Later, 20- and 30-mm braided-shaft balloons (Hyperglide; Micro Therapeutics, Inc.) were available, and most recently the highly compliant Hyperform balloon (Micro Therapeutics, Inc.), designed to occlude bifurcation aneurysms, became available. These new devices have improved the range of aneurysms in which the neck could be satisfactorily occluded.
During the period of study, several patients were also treated by use of a stent as an adjunct to Onyx. In most cases, the only available stents were balloon-expandable cardiac stents (SX 670; Medtronic AVE, Inc., Santa Rosa, CA) or the INX or Cerebrence stent (Medtronic AVE, Inc.). The use of stents varied and depended on the judgment of the treating physician. In some cases, an attempt was made to place a stent, but this failed because of the difficulties of maneuvering the relatively stiff stents to intracranial locations. In most of these cases, Onyx alone was used.
Seventy-nine percent of patients treated were female. The median age was 46 years, with a range of 6–76 years. Seventeen presented following subarachnoid hemorrhage (SAH). Of the 17, 10 were recent, within 1 month of treatment, and will be analyzed separately. In seven patients, the SAH was remote in time, and four had undergone previous coil placement in the aneurysms after the acute SAH, but the aneurysm had recurred.
In 29 patients, aneurysms were incidental, and in 46, presentation was associated with mass effect or headache thought to be due to the aneurysm. Twenty patients had undergone prior treatment, 15 with coils, two by craniotomy and wrapping, and in three stents had previously been placed. Table 1 presents patient demographics and aneurysm locations.
TABLE 1:
Patient demographics and aneurysm locations
| Sex | 79% Female |
| Age (y) | Median = 46 y, Mean = 45 y |
| (Range: 6–76 y) | |
| Presentation | |
| SAH: | |
| Recent (<1 mo) | 10 |
| Late (>1 mo) | 7 |
| Incidental | 29 |
| Mass Effect (including CN palsies) | 39 |
| Headache alone | 7 |
| Seizures | 2 |
| Other: | 6 |
| Nasal Bleeding | 3 |
| F/U of traumatic CCF | 2 |
| Previous SAH 1 y ago | 1 |
| Previously Treated | |
| Coil | 15 |
| Clip | 0 |
| Wrap | 2 |
| Stent | 3 |
Note.—SAH indicates subarachnoid hemorrhage; CN, cranial nerve; F/U, follow-up; and CCF, carotid cavernous fistula.
Table 2 shows the aneurysm sizes and locations with the recorded neck widths and lumen size at pretreatment angiography. Of the 100 aneurysms treated, 21 were small (<10-mm diameter), 60 were large (10–25-mm diameter), and 19 were giant (>25-mm diameter). Of the 21 small aneurysms, 15 had wide necks (≥4 mm) and 18 had a wide neck or a dome to neck ratio of <2. One aneurysm had a nearly fusiform neck.
TABLE 2:
Size and location of aneurysms
| Location | ||
| Carotid n = 93 | ||
| Petrous | 6 | |
| Cavernous | 25 | |
| Petrous/Cavernous | 2 | |
| Ophthalmic | 47 | |
| Other intracranial sites | 13 | |
| Posterior circulation n = 7 | ||
| Vertebral | 1 | |
| Vertebrobasilar | 1 | |
| Superior cerebellar | 1 | |
| Posterior cerebral | 2 | |
| Basilar tip | 2 | |
| Average aneurysm size (mm)* | ||
| Median | Range | |
| Dome height | 15 | 4–40 |
| Dome width | 14 | 3–44 |
| Neck width | 7 | 1–25 |
| Total | Neck <4 mm | Neck ≥4 mm | Neck ≥4 mm or D:N <2 | |
|---|---|---|---|---|
| Aneurysm sac (mm) | ||||
| Small (<10 mm) | 21 | 6 | 15 | 18 |
| Large (10–25 mm) | 60 | 3 | 57 | 57 |
| Giant (>25 mm) | 19 | 0 | 19 | 19 |
| n = 100† | 100 | 9 | 91 | 94 |
1 aneurysm nearly fusiform mc
Includes 1 fusiform neck.
Ninety-three aneurysms were in the carotid territory, with 33 in the petrous or cavernous segment. The single most common site was in the ophthalmic artery origin region, with 47 aneurysms. Seven posterior circulation aneurysms were treated.
Procedural Technique
The technique first involves the placement of a highly compliant DMSO-compatible occlusion balloon (Equinox or Hyperglide) in the parent vessel over the neck of the aneurysm. The balloon is left deflated while a DMSO-compatible microcatheter (Rebar, Micro Therapeutics, Inc.) is placed within the aneurysm. A slow test injection through the microcatheter is made with the balloon inflated to ensure that the neck is controlled and a satisfactory seal is achieved with stasis of contrast material within the aneurysm (Fig 1A and B). The microcatheter is then purged with saline, to clear any residue of contrast material, and primed with DMSO with a volume to match the catheter dead space. Onyx (HD 500) is then introduced into the microcatheter. Once sufficient volume (usually 0.2 mL) of the material has been injected, Onyx approaches the end of the microcatheter, and the balloon is inflated to the predetermined volume. Onyx is injected at a rate of about 0.1 mL per minute by using the specifically designed Cadence Precision Injector syringe (Micro Therapeutics, Inc.), which operates by a screw thread. Because of the viscosity of Onyx, it accumulates around the tip of the microcatheter and gradually enlarges to form a kernel that stays attached to the end of the microcatheter. After each injection, the balloon is left inflated for another 3 minutes and then deflated to allow cerebral reperfusion for at least 2 minutes; then the cycle is repeated.
With each injection, new portions of the aneurysm fill, and eventually the material flows down to the margins of the balloon and occludes the neck of the aneurysm. When the material is in contact with the balloon, injection is slowed or stopped with brief 15–30-second pauses to minimize the risk of leakage into the parent artery and beyond the balloon. It is important to ensure that material covers the aneurysm neck to achieve complete and durable occlusion and reduce the risk of aneurysm regrowth that is sometimes observed with wide-neck large and giant aneurysms. The microcatheter position is not adjusted at all once injection has started.
Following angiographic confirmation of the complete or satisfactory occlusion of the aneurysm, the catheter syringe is decompressed by aspiration of 0.2 mL and a 10-minute pause is taken to allow complete solidification of the polymer with the balloon deflated. The balloon is then reinflated and the microcatheter is removed by gentle traction.
Assessment of Angiographic Results
Degree of aneurysm occlusion was judged by the treating physician following the procedure, and this was recorded on the case review forms. All films were forwarded to a core lab for independent adjudication and review, and the results are shown in Table 3.
TABLE 3:
Angiographic outcomes assessed by core lab: immediate, 3 months, and 1 year
| Small <10 mm | Large 10–24 mm | Giant >25 mm | |
|---|---|---|---|
| Postembolization occlusion rates | |||
| n = 20 (%) | n = 60 (%) | n = 19 (%) | |
| Complete (100%) | 15 (75) | 33 (55) | 19 (47) |
| Subtotal (90–99%) | 5 (25) | 26 (43) | 19 (47) |
| Incomplete (<90%) | — | 1 (2) | 1 (5) |
| 3–6 month follow-up occlusion rates | |||
| n = 15 (%) | n = 51 (%) | n = 15 (%) | |
| Complete (100%) | 13 (86.7) | 31 (61) | 8 (53) |
| Subtotal (90–99%) | 1 (6.7) | 12 (23) | 4 (27) |
| Incomplete (<90%) | 1 (6.7) | 7 (14) | 2 (13) |
| Not determinable | 1 (2) | 1 (7) | |
| 12-month follow-up occlusion rates | |||
| After re-treatment, when applicable | |||
| n = 14 (%) | n = 39 (%) | n = 14 (%) | |
| Complete (100%) | 13 (93) | 30 (77) | 8 (57) |
| Subtotal (90–99%) | 0 | 5 (13) | 2 (14) |
| Incomplete (<90%) | 1 (7) | 2 (5) | 2 (14) |
| Not determinable | 2 (5) | 2 (14) |
Results
A total of 97 patients and 100 aneurysms were treated by 24 physicians in 20 centers during the period of the study. These centers and physicians are listed in the appendix, with number of patients per center cited. Ten patients were treated within 1 month of SAH. The remainder, 87 patients, were treated for unruptured aneurysms, recurrent aneurysms after prior endovascular treatment, or attempted surgical treatment or in the nonacute phase after SAH (>1 month). These two groups have been shown separately for clinical outcome to enable realistic comparison of results from other series of patients treated by endovascular and surgical means.
Procedural Information and Clinical Outcomes
A total of 108 Onyx procedures were performed in the 97 patients to treat 100 aneurysms during the study period. One patient underwent re-treatment with coils and one by parent artery occlusion (PAO). The duration of the procedure and volumes of material injected are shown in Table 4.
TABLE 4:
Procedural data
| Number of Procedures | 108 |
|---|---|
| Procedure time | |
| (Start time = time at which delivery catheter is filled with DSMO; Stop time = delivery catheter detachment from Oynx mass) | |
| Mean | 95 min |
| Range | 15 min–360 min |
| First 54 procedures | |
| Mean | 101 min |
| Range | 15–300 min |
| Second 54 procedures | |
| Mean | 90 min |
| Range | 20–360 min |
| Onyx volume | |
| Mean | 1.875 cc |
| Range | 0.07–10.25 cc |
| Treatment with Onyx + Stent | |
| Initial treatment | 17 |
| Re-treatment | 5 |
The procedure time reflects the time from commencement of the Onyx injection to its completion. It does not include the time required to place the balloon and position the microcatheter. There was a trend toward shorter procedure time as experience with the material improved.
An adjunctive stent was used in 17 patients during the first procedure and in five patients during a re-treatment procedure. Onyx treatment was performed immediately after stent placement in all cases.
The baseline clinical status of patients together with clinical outcome at 3- and 12-month follow-up is shown in Table 5. This is shown as those patients at Rankin 2 or better (independent); data were collected in a manner similar to that of the International Subarachnoid Aneurysm Trial (ISAT) (8) and the International Unruptured Aneurysm Study (ISUIA) studies (9, 10). It also shows those patients who had a worsened dependency score compared with their baseline assessment.
TABLE 5:
Baseline clinical and clinical outcome at 3 and 12 months
| Unruptured and Other | Recent SAH | |
|---|---|---|
| At baseline | n = 87 | n = 10 |
| Baseline Rankin ≥2 | 81 | — |
| Hunt & Hess grade | ||
| 1 or 2 | — | 7 |
| 4 | 3 | |
| At discharge* with including re-treatment as applicable | n = 86† | n = 10 |
| Rankin ≤2 | 76 (88%) | 5 |
| (95% CI 79–94) | ||
| Rankin Unchanged/improved | 75 | — |
| Rankin Worsened | 8 (9%) | — |
| Death at discharge | 3 | 1 |
| At 3–6 months including re-treatment as applicable | n = 82 | n = 7 |
| Rankin ≤2 | 74 (90%) | 6 |
| (95% CI 82–96) | ||
| Rankin Unchanged/improved | 74 | 7 |
| Rankin Worsened | 5 | 0 |
| Death at discharge to 3 months | 0 | 0 |
| 1 lost to f/u | ||
| 1 no data at 3 mths | ||
| At 12-Months or latest f/u, with re-treatment as applicable | n = 83† | n = 7 |
| Rankin ≤2 | 76 (91.5%) | 4 |
| (95% CI 83–96) | ||
| Rankin Unchanged/improved | 75 | 6 |
| Rankin Worsened | 3 | 0 |
| Death at 3 months to 12 months | 2 | 1 |
Discharge data missing in 1.
Includes four patients with no 3–6 month follow-up Rankin score.
Patients with unruptured or nonacutely ruptured aneurysms (87 patients) are shown separately from those with acute SAH (10 patients). At discharge in the former group, 76 of 86 with available data (88%, 95% CI 79–94) had a modified Rankin score (mRS) of 2 or better; and in 75 (87%), this was unchanged or improved. Three (3.5%) patients had died and eight (9.3%) had a worsened mRS.
At 3-month follow-up in this patient group, 74 of 82 patients (90%, 95% CI 82–96) with recorded Rankin scores had mRS of 2 or less. At 12-month follow-up, 76 of 83 patients (91.5%, 95% CI 83–96) with available Rankin scores had mRS of 2 or less. In four patients, the 3-month follow-up data were missing, but 12-month follow-up data were obtained. Two additional deaths occurred between 3 months and 12 months; they are described below.
Of the 10 patients treated acutely after SAH, seven had a good clinical grade (Hunt and Hess [H&H] grade 1 or 2) and three had an H&H grade of 4 at the time of treatment. At 12-month follow-up, 64 patients had an mRS of 2 or better, and two patients had an unchanged or improved, but greater than 2, mRS. In addition, one patient died during the first admission (a grade-4 H&H patient); one patient had been lost to follow-up; no data were available in one patient, but it was confirmed that this patient was alive at 16-month follow-up. One patient died at 8 months after treatment; cause of death could not be determined despite autopsy.
Serious Adverse Events and Case Fatality
Serious adverse events of some description were reported in 26 patients during the study period (based on the strict clinical trials definition and classification, described in the Methods section). The serious adverse events with neurologic consequences are listed in Table 6.
TABLE 6:
Serious adverse events with neurologic morbidity
| Patient Age (y)/Sex | Size and Location of Aneurysm | Description of Event and Cause of Event | Cause | Baseline Rankin or H& H | Outcome of Event and mRS at Last Follow-Up |
|---|---|---|---|---|---|
| Permanent morbidity | |||||
| 39/M | Large carotid ophthalmic | Ipsilateral visual loss due to leak in ophthalmic artery | Device | 0 | mRS = 1 |
| 42/F | Giant carotid cavernous | Worsened CN III, IV, V, and VI palsy, resolution of CN v aplsy | Procedure | 1 | mRS = 1 |
| 76/F | Small posterior communicating | Worsening of neurologic status (Grade, 2 H&H) | SAH | 2 | Lost to follow-up |
| 75/F | Giant carotid cavernous | Mild hemiparesis | Device (Onyx) | 1 | mRS = 1 |
| 44/M | Small carotid ophthalmic | Numbness in L leg caused by senosis of M3 MCA | Device (Onyx) | 0 | mRS = 1 |
| 56/M | Giant carotid ophthalmic | Onyx extravasation into subarachnoid space, SAH, severe hemiplegia | Device (Onyx) | 1 | Ongoing at 12 mnths, mRS = 4 |
| 45/F | Large carotid ophthalmic | Blindness in R eye post procedure with retinal infarct | Device (Onyx) | 0 | mRS = 1 |
| 55/F | Large carotid ophthalmic | Devloped delayed L MCA infarct 3 days afer retreatment with stent and Onyx caused aphasia and R hemiplegia | Device (Stent) | 2 | Ongoing at 3 months, mRS = 4 Partial resolution by 1 year |
| Transient neurologic morbidity | |||||
| 52/M | Large carotid ophthalmic | Developed symptomatic vasospasm with L hemiparesis; recent SAH | Disease | Grade 2 H&H | mRS = 0 Resolved |
| 47/F | Large superior | Developed transient hemiparesis | Device (also had stent placement) | 0 | mRS = 0 Resolved |
| 50/M | Large vertebro-basilar junction | Developed small SAH after catheter withdrawal; no neurologic deterioration; developed infected hematoma after 10 days retreatment procedure; required surgery | Procedure | ||
| 37/F | Small carotid cavernous | Developed confusion and ipsilateral hemiparesis headaches and nausea 1 week after treatment | Unknown | 1 | mRS = 1 Resolved by 6 months |
| 57/F | Large carotid cavernous | Procedural thrombus in left ICA; hemiparesis and aphasia; resolution of morbidity | Procedure | 0 | mRS = 1 Resolved by 2 days |
| 31/F | Large carotid ophthalmic | Transient hemiparesis | Procedure | 0 | mRS = 0 Resolved |
| 45/F | Large carotid ophthalmic | Developed worsened visual symptoms that subsequently improged | Device | 0 | mRS = 1 Complete resolution and visual improvement |
| 68/F | Recurrent basilar tip | Developed proximal brain stem stroke post procedure, probably thrombo-embolic, needed prolonged hospitalisation | Procedure | 1 | mRS = 2 Neurological symptoms fully resolved by 1 year |
Procedure-Related Adverse Events
In two patients, a serious groin complication occurred. One patient died as a consequence of a large groin hematoma, and one developed a delayed infected femoral artery pseudoaneurysm requiring surgery 10 days after treatment following the use of a closure device.
In nine patients, device-related adverse events occurred. Two of these were related to stent placement, one of which resolved. In five patients, there were serious adverse events related to Onyx, with clinical sequelae. In two of these five patients, the clinical complication resolved, and in three there was ongoing deficit. Table 6 lists all of the serious events with neurologic consequences occurring during the study period together with outcomes.
Altogether, procedure- and device-related adverse events resulted in permanent neurologic deficit in eight patients; in four patients this resulted in dependent survival (mAS 4) and four patients were scored at Rankin 2 or better (independent) status. There were two procedure-related deaths. In nine patients, neurologic sequelae resolved completely, and all were scored at Rankin 2 or less at final follow-up.
Follow-up CT performed after treatment showed no instances of remote distal migration of Onyx material from the main cast. There was one case of possible migration of a small fragment to a middle cerebral branch seen at angiography.
Case Fatality
A total of seven patients died during the period of study. Of the 87 patients treated for unruptured intracranial aneurysms (UIA), three died before discharge. Of those three, two were due to procedure-related events: one following a groin complication and one a delayed parenchymal and subdural hematoma probably secondary to vessel dissection. One was unrelated to the procedure, following a stroke in the contralateral hemisphere in a patient with atrial fibrillation. Of the 10 patients treated after recent SAH, one died before discharge; the cause of death was disease-related pulmonary complications.
There were three later deaths in the series: one due to myocardial infarction 11 months after treatment, one due to chest complications after a first SAH in an incompletely treated giant aneurysm 10 months after original Onyx treatment and 2 months after re-treatment with coils, and one due to unknown cause, despite autopsy, at 8 months.
Angiographic Results and Occlusion Rates at Follow-up
The angiographic outcomes are summarized in Table 3.
Ninety-nine of 100 aneurysms on local and 98 of 99 on core lab assessment were judged completely or subtotally occluded at the end of the procedure. Complete occlusion was judged to have been achieved in 64 of 100 by local assessment and 57 of 99 by core lab, with subtotal occlusion in 35 and 40, respectively. In two patients, core lab assessment judged occlusion to be incomplete.
At 3-month follow-up, the proportion of aneurysms with complete or subtotal occlusion was 90% and 89% on local and core lab assessments, respectively. Incomplete occlusion was seen in 10% of aneurysms at 3–6-month follow-up.
At 12 months, 71 of an expected 83 angiographic follow-up images were available with data from the case review forms: 56 (79%) showed complete occlusion; nine (13%), subtotal occlusion, and six (8%), incomplete occlusion. Nine patients had earlier been shown to have parent vessel occlusion and did not undergo 12-month intraarterial angiography, but instead underwent MR imaging. Thus, at 12-month follow-up, complete or subtotal aneurysm occlusion was judged to be present in 92% on the basis of case review form data and 87% from core lab data. Excellent correlation existed between the core lab and case review forms, with a Spearman correlation coefficient of 0.86 for 12-month follow-up results.
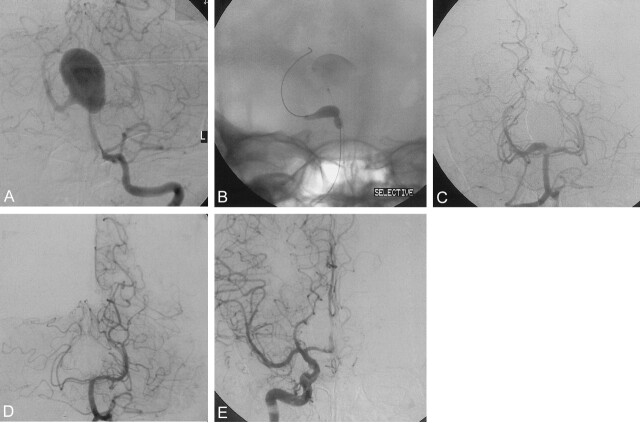
Figure parts 1C and D show the previously demonstrated aneurysm at follow-up 6 months after treatment. Healing intervening soft tissue between the vessel lumen and the Onyx cast is evident on the unsubtracted image. This is thought to be thickened fibrous tissue. Figure 2A–C shows a large basilar termination proximal posterior cerebral aneurysm in a 28-year-old hemophiliac patient with severe headaches. At 4-month follow-up angiography, the reconstructed segment of the proximal P1-segment vessel had occluded (Fig 2). MR imaging at 4 months suggested enhancing tissue in the occluded vessel, which implies that it was vascularized tissue rather than thrombus. No clinical ischemic events were reported by the patient, and no evidence of infarction was seen at MR imaging.
Fig 2.
28-year-old hemophiliac patient with severe headaches but no evidence of subarachnoid hemorrhage has a wide-neck basilar bifurcation aneurysm involving the proximal right postcerebral artery.
A, Large basilar bifurcation and proximal posterior cerebral aneurysms.
B, Seal test, showing highly compliant Equinox balloon inflated in the basilar tip and in the right posterior cerebral artery with the balloon protecting the aneurysm neck, which takes up most of the proximal P1-segment vessel.
C, Immediate posttreatment image, showing reconstruction of the posterior cerebral artery segment.
D, Three-month follow-up angiogram, showing occlusion of the proximal posterior cerebral artery and the aneurysm.
E, Three-month right carotid angiogram, showing posterior cerebral perfusion via the posterior communicating artery. (Images courtesy of Mike Nelson, Leeds.)
Aneurysm Recurrence and Re-treatment
Ten aneurysms (10%) required re-treatment between 3 and 12 months after initial treatment. One of 21 (5%) small aneurysms needed re-treatment; eight of 60 large (13%) and one of 19 (5%) giant aneurysms needed re-treatment. In three patients, Onyx alone was used; in five, a stent plus Onyx was used; in one, coils were used; and in one, parent vessel occlusion was performed. When recurrence of the aneurysm occurred, it was always seen at 3-month follow-up angiography. The incidence and implications for treatment strategy of the early recurrences that have been observed are addressed in the Discussion. Figure 3A–D shows a vertebrobasilar junction aneurysm that recurred and was subsequently re-treated with a stent and Onyx. Figure 3D was obtained at 6-month follow-up after the last treatment.
Fig 3.
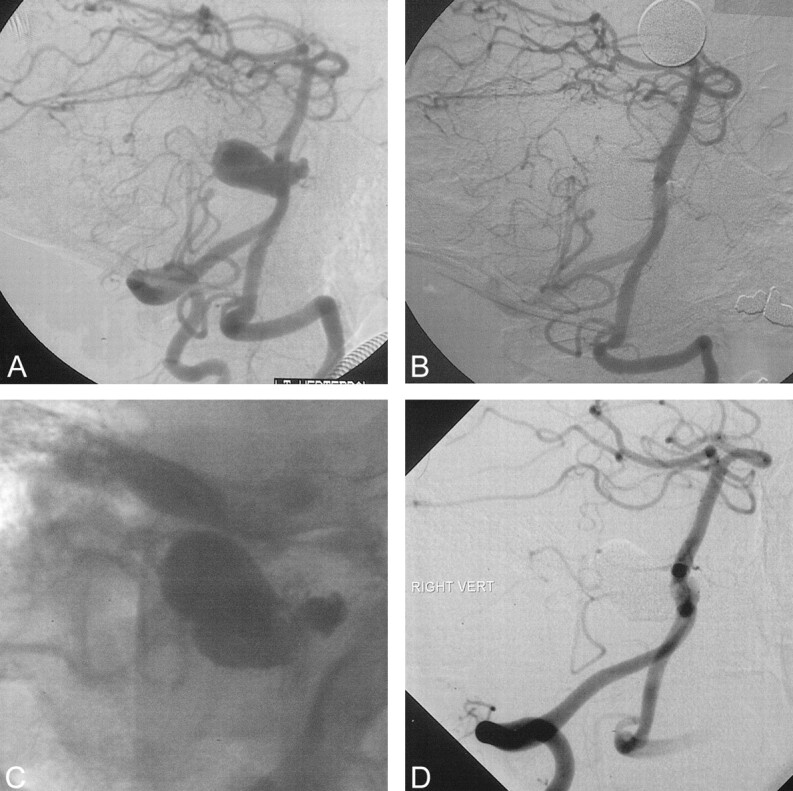
50-year-old male patient with leg weakness and a possible history of subarachnoid hemorrhage. This patient was found to have a vertebral basilar junction aneurysm compressing the medulla.
A, Pretreatment angiogram showing a large vertebrobasilar junction aneurysm treated on two occasions (treated with an INX stent at the second procedure after recurrence). Complete occlusion was noted at 6-month and 1-year follow-up after second procedure.
B, Angiogram obtained after second treatment at 3 months after early recurrence and after placement of an INX stent and re-treatment with Onyx.
C, Unsubtracted image obtained after second procedure, showing INX stent and second cast of Onyx in inferior recurrent aneurysm pocket.
D, Follow-up angiogram obtained 6 months after second treatment.
Mass Effect and Cranial Nerve Palsy
The results of aneurysm treatment on mass effect of the aneurysm and the outcome at follow-up are shown in Table 7.
TABLE 7:
Results of treatment on mass effect
| Optic nerve compression | |||
| Baseline | At Discharge | 12-Month or Latest Follow-up | |
| No. of patients | 14 | ||
| Improved/resolved | 2 | 6 | |
| Unchanged | 11 | 7 | |
| Worsened | 1 | 1 | |
| Additional patients | 1 | 0* | |
| *1 no follow up to date | |||
| Occulo-motor deficits | |||
| Baseline | At Discharge | 12-Month or Latest Follow-up | |
| No. of patients | 16 | ||
| Improved/resolved | 6 | 14 | |
| Unchanged | 8 | 1 | |
| Worsened | 1 | 1 | |
| 1 = died prior discharge | |||
| Hemiparesis or hemiplegia | |||
| Baseline | At Discharge | 12-Month or Latest Follow-up | |
| No. of patients | 8 | ||
| Improved/resolved | 1 | 5 | |
| Unchanged | 5 | 1 | |
| Worsened | 0 | 0 | |
| 2* = died | |||
| Headache (all), n = 57 at baseline | |||
| Baseline | At Discharge | 12-Month or Latest Follow-up | |
| Mild/moderate | |||
| No. of patients | 48 | ||
| Improved/resolved | 43 | 42 | |
| Unchanged | 2 | 1 | |
| Worsened | 0 | 2 | |
| 3 = died | |||
| At Discharge | 12-Month or Latest Follow-up | ||
| Severe | |||
| No. of patients | 9 | ||
| Improved/resolved | 8 | 8 | |
| Unchanged | 1 | 0 | |
| Worsened | 0 | 0 | |
| 1 = lost to follow up |
Of the 57 patients reporting headache at presentation, in 48, it was mild or moderate, and in nine, severe. Of the 48, 43 had improved or resolved at discharge, two were unchanged, and three patients had died. At 12-month follow-up, 42 were improved, one was unchanged, and in one, headaches worsened. Of the nine patients reporting severe headaches, eight had improved or resolved at discharge and eight had improved or resolved at 12-month follow-up (one patient was lost to follow-up).
Regarding cranial nerve palsies, 16 patients had oculomotor palsies at presentation. At 12-month follow-up, 14 had improved or resolved, one was unchanged, and one was worse. Fourteen patients had optic nerve compression before treatment. At 12-month follow-up, six had improved, seven were unchanged, and one patient was worse.
Parent Artery Occlusion
Of the 100 aneurysms treated, delayed PAO was observed in nine patients at follow-up angiography. This was present at 3-month follow-up angiography in all cases. Eight patients had been treated with Onyx alone, and one with a combination Onyx and stent. In five of the nine patients, Onyx entered either intentionally or unintentionally into the parent artery. One aneurysm had a small neck (<4 mm), but the remainder were wide necked with sac sizes ranging between 6 and 30 mm and neck sizes between 6 and 11 mm. Three of the nine patients were receiving extended antiplatelet therapy (aspirin and clopridogel). In five patients, the occlusion was asymptomatic. In two patients, symptoms were observed before discovery of the PAO: one patient with a giant cavernous aneurysm experienced worsening of her ophthalmoplegia, which had completely resolved by 3-month follow-up angiography, and one patient had several transient ischemic attacks, which responded to the antiplatelet regimen. In two patients, the occlusion resulted in significant permanent neurologic deficit. In the patient with the 4-mm-wide aneurysm neck, notable Onyx spill proximal to the balloon with a cuff in the parent artery was seen, and in one with a 6-mm neck, thrombosis at 48 hours was associated with the placement of a stent during the re-treatment.
PAOs appeared to occur in patients when a particularly wide aneurysm neck was present and when an extensive segment of vessel was reconstructed. Patients in the early phase of the study were not treated with an aggressive antiplatelet regimen. It was also observed if a significant spill of Onyx into the parent artery occurred in some instances beyond the balloon, thereby forming a cap over the balloon in the parent vessel. Technical improvements in the system have been introduced since this time and are elaborated in the Discussion.
Figures 3 and 4 show examples of patients with parent vessel occlusion. Figure 3 shows angiograms obtained in 28-year-old hemophiliac presenting with severe headaches and a distal basilar aneurysm involving the right posterior cerebral, in whom the posterior cerebral artery was reconstructed. Three-month follow-up showed occlusion of this segment of posterior cerebral and filling of the posterior cerebral territory from the posterior communicating artery. Figure 4 illustrates a case of a patient treated for a cavernous carotid aneurysm who originally presented with partial cranial nerve III palsy. This worsened after the procedure but had resolved by 3 months, when the follow-up angiogram showed the PAO. Both of these patients were asymptomatic at 12-month follow-up.
Fig 4.
45-year-old patient presenting with a partial cranial nerve III palsy and headache. No anterior cerebral artery was present on the left side and the carotid only supplied the left middle cerebral territory.
A, Lateral arterial phase carotid angiogram obtained immediately before treatment.
B, Final angiography obtained after Onyx treatment balloon catheter still present in vessel.
C, Follow-up angiography 3 months after procedure. Patient developed a complete ophthalomoplegia immediately after the procedure, which had resolved entirely by 3 months when she was asymptomatic. Note extensive orbital collaterals filling middle cerebral territory. (Images courtesy of Peter Flynn and Steven Mckinstry, Royal Victoria Hospital, Belfast.)
Discussion
The importance of endovascular treatment of ruptured intracranial aneurysms with detachable platinum coils has now been firmly established following the publication of the results of the ISAT (8). It has been shown to result in a better clinical outcome at 1 year than surgical treatment for patients with small ruptured anterior circulation aneurysms suitable for endovascular treatment. That study did not, however, address the issue of large, giant, or unruptured aneurysms, because such patients were not part of the trial.
The data from the prospective observational study, ISUIA, have recently been published (9, 10). These data have shown the outcomes of the surgical management of unruptured aneurysms to be surprisingly poor in terms of clinical outcome based on combined mRS 3–6 or the cognitive deficits seen at 1-year follow-up. This is particularly the case for large and giant aneurysms, for which the rates of poor outcome were 25% and 34%, respectively (10).
The frequency of poor clinical outcome at 1-year follow-up in the ISUIA study of the endovascular management of the large and giant aneurysms were 10% and 14%, respectively, by the endovascular techniques available at the time during the period of the study (1996–1999). This also included significant numbers of cases of balloon occlusion of the parent artery, usually for cavernous aneurysms, and was a relatively early experience with endovascular platinum coil placement. Subgroup analysis by aneurysm size showed that poor clinical outcomes were significantly higher for large and giant aneurysms than for small aneurysms, with a 10% rate of poor outcome for aneurysms 10–24 mm in diameter and 18% for giant aneurysms (although with inevitably wide CI). The angiographic occlusion rates obtained in this study, however, showed a complete occlusion rate of 50% at 1 year. Twenty-five percent of aneurysms were incompletely occluded, and an additional 25% were not at all occluded. There were far fewer endovascularly treated patients in this study (n = 451) than surgical patients (n = 1916). Many of the patients enrolled in the endovascular group were patients who had been rejected for surgery or had an aneurysm located in the cavernous carotid segment (19%) or in the posterior circulation (24%). Thus, because the populations of these two groups differed so much, it is not possible to draw accurate conclusions as to the relative risks of surgery and endovascular treatment on the basis of these data.
Since that time (1996–1999), there have been major improvements in the endovascular techniques available, with a much wider range of devices, including 3D coils, spherical coils, the TriSpan neck bridge device, and wider use of the balloon remodeling technique. These developments have widened the range of aneurysms that are regarded as suitable for endovascular treatment. Bioactive and hydrogel coils have recently been introduced to try and improve the healing of the aneurysm neck in both narrow and wide-neck aneurysms. Even with these devices, however, there remains a group of patients with aneurysms that are difficult or impossible to treat by coil placement, or based on the existing published experience, have a high likelihood of aneurysm recurrence. Many large and giant aneurysms treated with coils develop a significant recurrence and require further treatment. This is the patient group with the highest surgical risk.
As an aneurysm enlarges, the neck frequently takes up an increasing proportion of the circumference of the parent vessel wall. This makes closure of the neck and healing reconstruction of the vessel wall without some form of support problematic. This probably explains why the angiographic results of coil treatment get progressively worse as aneurysms get larger and necks wider, particularly when an aneurysm is more than 15–20 mm in diameter. For this reason, many interventionists decline to treat such aneurysms.
The results of coil treatment of large and giant aneurysms have recently been published in several series. Muryama et al (11) reported the long-term results of coil occlusion by using the Guglielmi detachable coil device from the series from the University of California, Los Angeles, Medical Center. In the patients in this series with large and giant aneurysms, the acute occlusion rates for large aneurysms were complete in 40% and incomplete with a neck remnant in 45%. At follow-up, however, the overall recurrence rates for large aneurysms was 35%, with 20% of completely occluded aneurysms recurring and 40% of those with a remnant.
For giant aneurysms, the results were worse, with recurrence rates of 59% if incompletely occluded at the time of treatment and 33% if completely occluded at treatment. A study by Sluzewski et al (12) of large and giant aneurysms treated by coils reported that, although 79% had a good clinical outcome, incomplete occlusion was seen in 20 of 29 aneurysms at follow-up and even with repeat endovascular treatment 12 of 29 aneurysms were incompletely occluded and required surgical treatment or parent vessel occlusion. Gruber et al (13) reported the need for multiple procedures in the endovascular treatment of large and giant aneurysms and achieved a complete or subtotal occlusion rate of 71%, but single treatment sufficed in only 12.5% of giant and 31% of large aneurysms.
Stents in association with coils (14) have been used to treat wide-neck aneurysms that cannot be treated by coils alone or with balloon assistance; however, the availability of stents that can be satisfactorily navigated into the intracranial circulation has, until recently, been limited because of the stiffness of the balloon devices (11). Newer, more flexible self-expanding stents that can be delivered via a microcatheter are now becoming available. These new devices may in part address this problem.
The use of a liquid agent that is able to completely obliterate the aneurysm sack and close the neck has significant attractions. The balloon protects the patency of the parent vessel during the procedure. It enables reconstruction of the missing vessel wall with the hope of permanent reconstitution of the vessel wall and permanent closure of the aneurysm. The disadvantage is that it increases the technical complexity of the procedure.
Technique and Technical Evolution
The introduction of any new device is inevitably accompanied by evolution of the technique as clinical experience grows, case selection improves, and the technology is refined. The results also must be seen in the context of the clinical options for individual patients and the results of alternative treatments if these are available. It is clear from the surgical results that the clinical outcomes of surgical treatment for large and giant aneurysms are relatively poor and that the endovascular results with coils have been unsatisfactory, mainly because of the poor occlusion rates that are obtained on a medium-term basis. The introduction of a new technique that seeks to deal with this patient group is bound to be applied to a very select and difficult population of patients. This applied to the introduction of the Guglielmi detachable coil device, which until recently was labeled for use only in high-risk and surgically unsuitable aneurysms (13). Thus, any new technology to be assessed must be done in the light of the options that are available to the patient and the likely outcomes of those options.
The technology also needs to be usable by most of the expert clinical community in the field following training in its use. If the new technology can only be used by a few people, it is not going to provide a commercially and clinically successful technique or device. Thus, the results of an evaluation carried out among a large number of centers with a diversity of clinicians is likely to provide a more representative reflection of what can be expected when a device is commercialized.
The technical challenges of the procedure have related primarily to the placement of the remodeling balloon over and beyond the aneurysm neck. It has been stated many times at scientific meetings that this technique is difficult. We do not believe this to be the case. It is a technique that requires training and contains a number of technical steps. The main technical challenge, however, is related to balloon placement. When the aneurysm neck is very wide, and particularly at the ophthalmic artery origin, balloon placement can be difficult. In a number of cases, catheterization beyond the aneurysm with a regular microcatheter and 0.014-inch wire enabled the necessary 0.010-inch exchange wire to be placed beyond the aneurysm and satisfactory balloon placement achieved.
Findings of This Study
Clinical and Angiographic Results
The 3- and 12-month clinical outcomes in patients treated for an UIA with nonacute or recurrent aneurysms show that about 90% of patients had a good Rankin outcome of 0–2. This compares very favorably with the clinical results after surgical treatment for patients with large and giant aneurysms and is comparable with the recently reported ISUIA results of endovascular treatment of large and giant aneurysm patients (10).
In addition, the aneurysm occlusion rates were substantially better than any other results reported for endovascular techniques in large and giant aneurysms. In a recently published study (11), the occlusion rate achieved in large and giant aneurysms by using coils, including re-treatments, was only 17 (59%) in 29 aneurysms. In some patients in this series, despite apparently good angiographic results, there was early reopening of the aneurysm that, in a number of cases, was quite sizable and required further treatment. Recurrence continues to be seen in a few patients with large and giant aneurysms and emphasizes the need to ensure that good neck coverage and occlusion is obtained at the first procedure. The reason for this recurrence is not known; however, Onyx, unlike cyanoacrylate, is nonadhesive. Because of the nonadhesive nature of Onyx, it is possible that, unless complete neck closure is obtained, particularly at the in-flow zone, blood in-flow can dissect between the Onyx cast and the vessel wall. Further, determining when complete neck occlusion has been achieved can be difficult. The adjunctive use of a stent may improve morphologic results, but this remains to be seen. Currently available stents for intracranial use present technical challenges of placement, particularly those that are balloon expandable. The risks of a delayed hemorrhage, particularly in patients with large or giant aneurysms, are not insignificant, and 10 of the 12 delayed rebleeds reported in the series by Muryama et al (11) occurred in patients with large or giant aneurysms, emphasizing the need to ensure satisfactory angiographic occlusion in this patient group, if possible. Significantly improved stent devices are now becoming available for treatment of wide-neck intracranial aneurysms. Thus, it is not clear at this time whether in some cases Onyx is best used in combination with a stent, particularly for difficult and wide-neck aneurysms and in the re-treatment of aneurysms following recurrence after Onyx treatment. Stents were used in 23 patients during the study, but only balloon-expandable stents were available for use in the intracranial circulation during the period of the study, thus limiting their use. It remains to be seen whether the new self-expanding and more flexible intracranial stents may be more appropriate and produce better morphologic results.
Parent Artery Occlusion
Understandably, there is concern regarding a significant incidence of delayed occlusion of the parent artery. This was particularly seen in earlier cases in the series when the material spilled into the parent artery, or when there was extensive reconstruction of the parent vessel in very wide-neck aneurysms. In addition, during this early period, no standard antiplatelet drug regimen was in use.
Later in the series, more aggressive antiplatelet therapy before and after the procedure was introduced. In addition, further system improvements have been introduced since the study was completed, including longer balloons (up to 30 mm), denser Onyx HD 500+ with better visibility, and the Quick Stop syringe (Micro Therapeutics, Inc.), which allows nearly immediate stopping of the injection. The Quick Stop syringe is an important improvement, because it permits immediate decompression of the material, thus stopping the toothpaste effect whereby the material continues to run after injection ceases. Since the introduction of these technical changes, unintended spill into the parent artery has largely been avoided, and no parent vessel occlusions have been observed by the authors or reported to the company in post-marketing surveillance of patients in this series. Data are insufficient to conclude whether or not this had an effect on its incidence.
Mass Effect
An important consideration, particularly when treating large and giant aneurysms, is the result treatment will have on mass effect and neurologic symptoms associated with such mass, especially when the aneurysm is not being removed, but rather is being filled with an inert polymer. The single-most common mass effect symptom associated with intracranial aneurysms is cranial nerve palsy, either oculomotor palsies or optic nerve compression. The anxiety concerning the replacement of the mass of an aneurysm with material that does not shrink significantly is that such symptoms may not resolve. It is therefore striking that nearly all patients with ophthalmoplegia showed complete or significant recovery of function. The results were less dramatic, as might be expected, with optic nerve compression. The effect on headache, while less easy to quantify, was significantly improved in almost all patients at both discharge and follow-up.
The results of this study suggest that Onyx HD500 can produce occlusion rates that are significantly better than the reported endovascular occlusion rates achieved with existing coil devices, in light of the difficult size and configuration of most of the aneurysms in this series. Patients were prospectively enrolled and data collected in a consecutive series of patients from several centers from the start of the experience. Nevertheless, the occlusion rates are excellent. The procedural complication rates and the clinical outcomes at 3 months and 12 months are comparable with the reported rates of clinical complications seen with coil treatment of unruptured aneurysms in the earlier series and compare very favorably with the complication rates reported following surgical treatment of large and giant aneurysms. As such, these results during the introductory phase of a new device are encouraging.
Conclusion
This study has provided the first reliable prospective data on the clinical and angiographic outcomes of patients with difficult intracranial aneurysms treated with a new liquid device, Onyx HD500. It has shown that Onyx can produce durable aneurysm occlusion in patients with difficult large and giant wide-neck intracranial aneurysms when other endovascular techniques are likely to fail and when surgery carries substantial morbidity. The clinical results and complication rates appear comparable with other endovascular techniques for similar patient populations, but the final occlusion rates appear significantly better than those reported for this type of aneurysm following coil treatment. In large aneurysms presenting with mass effect symptoms, the relief of these symptoms was seen in most patients.
Appendix
Participating Centers and Physicians
European CAMEO Study group providing data as described, with numbers enrolled given in parentheses (patients/aneurysms):
Günther Klein, Graz, Austria (2/2); Elisa Ciceri, Milan, Italy (1/1); James Dervin, Middlesborough, UK (1/1); Christophe Cognard, Toulouse, France (2/2); Soren Bakke, Oslo, Norway (2/2); Timothy Hodgson, Sheffield, UK (2/2); Christophe Groden, Hamburg, Germany (1/1); Alfredo Casasco, Madrid, Spain (1/1); David Hughes and Roger Laitt, Salford, UK (2/2); Ditmar Kuhne, Essen, Germany (2/2); Luis Lopez-Ibor, Alicante, Spain (2/2); Andrew Molyneux, Oxford, UK (15/15); Ralf Siekmann, Geissen, Germany (1/1); Gyula Gal and Metin Tovi, Uppsala, Sweden (9/10); Hans Nahser, Liverpool, UK (4/4); Istvan Szikora, Budapest, Hungary (3/3); Saruhan Cekirge and Isil Saatchi, Ankara, Turkey (36/38); Shelley Renowden, Bristol, UK (1/1); Edoardo Boccardi, Milan, Italy (3/3); Civan Islak and Naci Kocer, Istanbul, Turkey (7/7).
Acknowledgments
We wish to thank all of the investigators and staff in the participating centers for the hard work in assembling these data, especially Mary Sneade and Caroline Cowsill, at the Neurovascular Research Unit, Oxford. Also, thanks to the staff at Microtherapeutics, Inc., for the diligence with which they pursued this investigation, particularly Karen Davis and Anne Ainsworth of MTI, Anne Lenaghan of ev3, and d-Target who audited the data.
Footnotes
Supported by research grants from Microtherapeutics, Inc., Irvine, CA.
Presented at the 41st annual meeting of the American Society of Neuroradiology, Washington, DC, April 28–May 2, 2003.
A.J.M., S.C., and G.G. have consulting agreements with Microtherapeutics, Inc., to provide training and proctoring advice.
References
- 1.Taki W, Yonekawa Y, Iwata H, et al. A new liquid material for embolization of arteriovenous malformations. AJNR Am J Neuroradiol 1990;11:163–168 [PMC free article] [PubMed] [Google Scholar]
- 2.Muryama Y, Vinuela F, Ulhoa A, et al. Nonadhesive liquid embolic agent for cerebral arteriovenous malformations: preliminary histopathological studies in swine rete mirabile. Neurosurgery 1998;43:1164–1175 [DOI] [PubMed] [Google Scholar]
- 3.Chalouopka JC, Huddle DC, Alderman J, et al. A re-examination of the superselective injection of DMSO in swine rete mirabile embolization model. AJNR Am J Neuroradiol 1999;20:401–410 [PMC free article] [PubMed] [Google Scholar]
- 4.Jahan R, Murayama Y, Gobin YP, et al. Embolization of arteriovenous malformations with ONYX, clinico-pathological experience in 23 patients. Neurosurgery 2001;984–997 [DOI] [PubMed]
- 5.Molyneux AJ, Coley SC. Embolization of spinal cord arteriovenous malformations with ethyl vinyl alcohol coplolymer dissolved in DMSO (ONYX liquid embolic system): report of 2 cases. J Neurosurg (Spine) 2000;93:304–308 [DOI] [PubMed] [Google Scholar]
- 6.Mawad ME, Klucznik RP, Ciceri EF, et al. Endovascular treatment of cerebral aneurysms with the liquid polymer ONYX: initial clinical experience. Presented at the 39th annual meeting of the American Society of Neuroradiology, Boston, April 23–27,2001. :290 .
- 7.Moret J. One year experience and follow up of 18 intracranial aneurysms treated with ONYX injection: analysis of results. Presented at the 39th annual meeting of the American Society of Neuroradiology, Boston, April 23–27,2001. :291 .
- 8.International Subarachnoid Aneurysm Collaborative Group. International Subarachnoid Aneurysm Trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2,143 patients with ruptured intracranial aneurysms: a randomized trial. Lancet 2002;360:1267–1274 [DOI] [PubMed] [Google Scholar]
- 9.International Study of Unruptured Intracranial Aneurysms (ISUIA) Investigators. Unruptured intracranial aneurysms: risk of rupture and risks of surgical intervention. N Engl J Med 1998;339:1725–1733 [DOI] [PubMed] [Google Scholar]
- 10.International Study of Unruptured Intracranial Aneurysms (ISUIA) Investigators. Unruptured intracranial aneurysms: natural history, clinical outcome and risks of surgical and endovascular treatment. Lancet 2003;362:103–110 [DOI] [PubMed] [Google Scholar]
- 11.Muryama Y, Nien YL, Duckwiller G, et al. Gugliemi detachable coils embolisation of cerebral aneurysms: 11 years experience. J Neurosurg 2003;98:959–966 [DOI] [PubMed] [Google Scholar]
- 12.Sluzewski M, Menovsky T, van Rooij WJ, Wijnada D. Coiling of very large and giant aneurysm: long-term clinical and serial angiographic results. AJNR Am J Neuroradiol 2003;24:257–262 [PMC free article] [PubMed] [Google Scholar]
- 13.Gruber A, Killer M, Bavinzski G, Richling B. Clinical and angiographic results of endosaccular coiling treatment of giant and very large intracranial aneurysms: a 7-year, single-center experience. Neurosurgery 1999;45:793–803 [DOI] [PubMed] [Google Scholar]
- 14.Vanninen R, Manninem H, Ronkainen A. Broad-based intracranial aneurysms: thrombosis induced by stent placement. AJNR Am J Neuroradiol 2003;24:263–266 [PMC free article] [PubMed] [Google Scholar]