The 38th annual meeting of the ASNR was held at the Hyatt Regency Hotel in Atlanta from April 3 through April 8, 2000, under the direction of Eric Russell, the president and presiding officer. The meeting was preceded by a 2-day course on advanced imaging techniques that, along with the annual meeting, was organized by Bill Ball, the president-elect and program chairman. An increasingly important and well-attended portion of the meeting was the Electronic Learning Center, chaired by Hervey Segall. “How-to” sessions were well attended and continue to be an important part of the annual meeting. Of interest was the first use of the Electronic Learning Center for industry-sponsored programming with a focus on PACS. There was a total of eight sessions with hands-on use of PACS in the practice of neuroradiology.
As has been done in the recent past, each specialty society, the American Society of Interventional and Therapeutic Neuroradiology, the American Society of Spine Radiology, the American Society of Pediatric Neuroradiology, and the American Society of Head and Neck Radiology, developed their own segments of the meeting, integrating their material with the general programming. Bill Ball worked closely with the chairmen of the scientific committees of each society to build a meeting of clinical importance and state-of-the-art science and technology. Scientific exhibits, posters, computer-assisted exhibits, and technical exhibits were on display throughout the week. The awards for scientific exhibits are listed in this issue of the AJNR (page 1971). On Wednesday, Eric Russell gave the annual presidential address (page 1973), which was followed by the society's special presentations. The Gold Medal was presented to Bud Baker, and the Cornelius G. Dyke Memorial Award went to William Marx for his work entitled Endovascular Treatment of Experimental Aneurysms using Biologically Modified Embolic Devices: Coil-mediated Intraaneurysmal Delivery of Fibroblast Tissue Allografts. Berlex/ASNR fellowships were awarded to John Port and Eric Schwartz, and the ASNR Foundation Health Services Research Fellowship was awarded to Melanie B. Fukui. Awards for the best presentations at the 1999 ASNR annual meeting in San Diego were given in six different categories: general neuroradiology, pediatric neuroradiology (the Derek Harwood-Nash Award), interventional neuroradiology (the Michael Brothers Award), spine radiology, head and neck radiology, and the Berlex Outstanding Presentation; the winners are listed in this issue of the AJNR (page 1970). At the annual Business Meeting, Marco Leonardi received honorary membership in the ASNR. Brief biosketches of Dr. Baker, the Gold Medal recipient, and Dr. Leonardi, the newest honorary member of our society, appear in this issue (page 1969).
Prior to the start of the annual meeting, a 2-day symposium entitled Advanced Imaging Symposium: Preparing the Neuroradiologist for the New Millennium was held. The concept behind this symposium was that the upcoming decade will be one of change for neuroradiologists as new technologies emerge and are applied to the care of the central and peripheral nervous systems in children and adults. Because neuroimaging will gradually switch from a primarily anatomic-based approach to one of understanding the basic functional pathophysiology of a disorder through advanced neuroimaging, the symposium focused on MR spectroscopy (MRS), functional MR (fMR) imaging, diffusion-weighted imaging, and perfusion-weighted imaging. Each topic included core lectures in brain pathophysiology, technical performance, and interpretation of these examinations, as well as current clinical applications.
The core scientific lectures were combined with presentations to place these challenges in perspective with respect to economic and political issues. Discussions on who should perform and interpret advanced imaging methods, and the future of departmental structure for neuroradiologists gave many in the audience time to reflect on their own organizational structure. A lecture on how to incorporate advanced imaging into the daily practice of neuroradiology was a clear indication that the goal of using advanced techniques is applicable to both universities and private practices.
The annual meeting spanned 6 days, and time was apportioned so that papers and lectures dealing with vascular/interventional and spine imaging were presented in the first half of the meeting, and papers and lectures in head and neck radiology and pediatric neuroradiology were presented in the second half of the meeting. Interspersed throughout the meeting were topics of economic and political interest to the membership, including updates on standards of practice, credentialling, CPT activities, healthcare economics, and balancing neuroimaging quality with cost. In parallel with these lectures were presentations on a variety of topics, including how to write and review a scientific paper, funding opportunities for neuroimaging researchers, grant structure and composition, and biostatistics. Sessions dedicated to research techniques and opportunities will be emphasized more fully at future ASNR meetings.
Excellent presentations were given throughout the week; the following were some highlights of the ASNR annual meeting. During the time devoted to interventional techniques, invited speakers reviewed and discussed new developments and their experiences in the treatment of ischemic and hemorrhagic stroke, extracranial atherosclerotic occlusive disorders, and spinal disease. Indicative of its importance, three focus sessions were devoted largely to the role of advanced CT and MR techniques in the assessment of stroke patients. Although it is not yet certain whether CT or MR will ultimately assume the dominant position for stroke, it was clear that by using combinations of contrast-enhanced CT, CT angiography, CT perfusion, or MR with diffusion/perfusion imaging, there is now a greater ability to identify more accurately those patients who are most likely to benefit from or to be harmed by interventional therapy.
New advances in the treatment of aneurysms, arteriovenous malformations, and vasospasms were discussed, and a session was devoted to new developments in angioplasty and stenting. New imaging capabilities such as 3D X-ray and CT angiography, along with improvement in devices available to the interventionalist, are improving the safety and efficacy of these procedures. Scientific papers reported noteworthy experiences in the use of stents for the treatment of intracranial aneurysms and carotid vascular disease. In one prospective study conducted over a 7-year period, in which the efficacy and morbidity related to the endovascular treatment of unruptured intracranial aneurysms was determined, only five of 116 patients suffered a neurologic deficit as the result of treatment. All of those were minor, and all patients had a good outcome. It was concluded that even though recent studies suggest that a natural history of unruptured asymptomatic aneurysms may be more benign than had been previously thought, endovascular treatment still may offer a realistic alternative to conservative management of patients with such lesions. In a retrospective analysis of 14 consecutive patients who presented with an acute ischemic stroke, and were treated using a combination of intravenous and local intraarterial recombinant tissue plasminogen activator, there appeared to be an improvement in patient outcome.
New techniques in spine imaging and a widening experience in spine intervention dominated the spine portion of the meeting. There is continued interest in applying diffusion-weighted imaging to the spine. In a report in which 12 patients with 17 spinal lesions and with suspected spinal metastasis were examined with a fast spin-echo technique using a b value of 250, apparent diffusion coefficient (ADC) maps helped to improve specificity by eliminating the T2 component of the bright signal observed on the diffusion images. The authors showed that metastasis had a lower ADC value than benign lesions such as hemangiomas, although some overlap did exist. In another spine diffusion-weighted imaging presentation, 25 patients with metastasis were evaluated to determine the usefulness of diffusion-weighted MR imaging for monitoring the response of therapy. Diffusion-weighted imaging appeared to reflect a change in the signal intensity earlier than conventional imaging sequences after radiation therapy. The change in signal intensity on diffusion-weighted imaging in the bone marrow of patients with metastasis was seen 2 months after therapy. Also, diffusion-weighted MR imaging using a steady-state free precession sequence was performed for differentiating benign from malignant compression fractures. It was found in 58 patients that all hypointense foci were benign, and of the hyperintense lesions, false-positive results occurred in eight (38%) of 29 lesions.
To identify and better characterize spinal arteriovenous malformations (AVMs), CT myelography in patients with suspected AVMs was correlated with spinal angiography. A negative CT myelogram was found to be unreliable in excluding an AVM, and a positive CT myelogram was always followed by a spinal angiogram; therefore, it was felt that CT myelography was not useful in the diagnosis and management of spinal AVMs. To determine the level of arterial feeders in spinal dural AVMs, one group described the use of a sagittal, 3D, centrally-encoded, contrasted-enhanced MR angiographic sequence. The sequence was automatically triggered by a bolus tracking technique. With evaluation prior to conventional spinal angiography, the authors were able to identify the location of the spinal dural AVM and its feeders.
As evidenced by a focus session and a lecture on interventional radiology in cases of cervical disk herniation, spinal interventions are assuming an increasingly important role in neuroradiology practices. New concepts and devices using minimally invasive techniques offer promise for improvement in the ability to treat effectively many of the conditions that cause neck and back pain. Interventional spine techniques also centered on vertebroplasty, facet/foraminal injections, and spine biopsies. One study prospectively evaluated the efficacy of percutaneous polymethacrylate vertebroplasty in patients with osteoporotic vertebral compression fractures. The Musculoskeletal Outcomes Data Evaluation and Management and System Scale was used in the determination of procedural efficacy 2 weeks after vertebroplasty. In 54 treated compression fractures in 30 patients, significant postoperative clinical improvement related to pain and disability was demonstrated. This study revealed the efficacy of vertebroplasty performed under fluoroscopic control in a prospective manner using a pre- and postprocedural questionnaire. In the discussion that followed this presentation, the need for long-term clinical outcome follow-up was stressed. The ability to depict spinal facet arthropathy and perifacet abnormalities better by use of a fat-suppression technique was described; it was felt that significant facet symptomatology could not be shown by MR unless a fat-suppression technique was used. The efficacy of a percutaneous, CT-guided, transpedicular approach to obtain biopsy specimens from vertebral-body lesions was stressed in another paper.
Continued society interest in the basic science of spinal cord injury (SCI), and strategies for the eventual treatment of patients with SCI, was stressed in a focus session on this subject. The potential of mild hypothermia and various pharmacologic therapies (eg, fibroblastic growth factor, cytokines, and interleukin-10) were mentioned, but it is probable that such approaches may be of benefit only during specific limited periods following an SCI. Although there has been some experimental success in axonal regeneration using Schwann cells and olfactory ensheathing glial cells, physical and perhaps chemical barriers have led to limited neural regeneration. Various strategies including growth-promoting factors have been used with some success to help the regeneration process. Drug treatment studies for SCI were also reviewed in this focus session; specifically, it was noted that GM1 is a promising drug that can lead to more rapid neurologic recovery. Because neurologic recovery plateaued in patients receiving GM1 when the drug was discontinued, it was suggested that continued use of GM1 might result in further neurologic improvement. A demonstration of the use of multislice spiral CT in the evaluation of injuries at the craniocervical junction led to the inevitable conclusion that multislice, reformatted, spiral thin-slice (0.5 mm) CT can be used effectively to replace plain radiographs in spine trauma. The discussion following the presentation emphasized in part how to deal with the large number of images generated by this technique.
The means of obtaining high-quality images of the brachial plexus was the topic of a presentation in which a dedicated surface coil and specific pulse sequences were described. It was stressed that it is necessary to saturate the signal from fat, and in this regard short-inversion-time inversion recovery imaging was judged superior to fat-suppressed fast spin-echo imaging. To visualize the fasicular pattern of the nerves, a dedicated coil is necessary.
A paper on the possible relationship between arachnoid webs and the development of syringomyelia engendered considerable discussion. Although resection of these bands was associated with good clinical outcome, the question was raised whether these findings were, in fact, most consistent with focal arachnoid cysts rather than arachnoid webs. Whatever the explanation, alteration in CSF flow dynamics resulted in syrinx formation.
Techniques devoted to assessing cerebral blood flow (CBF) were presented in a number of sessions devoted to brain imaging. Acetazolamide challenge using an arterial spin-tagging technique was found to be reproducible in eight individuals, and a cerebral stress test in two instances showed increased CBF to the cortex and thalami. Although the data are limited, this technique may be promising in assessing the influence that carotid artery stenosis has on CBF and, possibly, in determining which patients need surgery. Another presentation evaluated arterial spin-tagging MR perfusion in patients with acute cerebral infarctions. All infarctions showed decreased CBF and, in one patient treated with intravenous thrombolysis, perfusion was increased despite restricted diffusion on diffusion-weighted imaging; thus, perfusion studies are needed in addition to diffusion-weighted imaging. Other authors used CT to assess cerebral perfusion in patients with subarachnoid hemorrhage, and found that CT was able to detect differences in cerebral blood volume (CBV) and CBF in patients with significant vasospasm when compared to those with absent/minimal vasospasm. Because CT is commonly obtained in these patients, this may be helpful in identifying patients in need of therapy and in appraising the influence of various pharmaceutical and invasive therapies for treatment of vasopasm. In a retrospective analysis of 15 patients with cerebral infarctions, the area of abnormal perfusion by CT in combination with the patients' clinical status predicted the final volume of infarction. Thus, CT perfusion may be helpful in both the diagnosis of acute cerebral infarction and in patient outcome assessment. The use of gadolinium perfusion MR revealed a difference in relative CBV between high-grade gliomas and cerebral metastases, particularly in the peritumoral regions; the authors suggested that this technique may be promising in patients presenting with solitary brain lesions. Similarly, another presentation showed that gadolinium perfusion MR allowed differentiation between tumor progression and radiation treatment sequelae. The observations of these latter two papers are promising, but they need to be reevaluated in larger patient groups.
Diffusion-weighted imaging of the brain remains a topic of great interest, particularly when it is applied to diseases other than cerebral ischemia, for which its effectiveness is well-known. Two presentations showed that high-grade tumors have higher ADCs than benign brain tumors, but that classification of high-grade tumors according to their ADC determinations may not be accurate; thus, the utility of diffusion-weighted imaging in the assessment of some brain tumors is still questionable. Diffusion-weighted imaging was used to evaluate patients within 2 hours of carotid endarterectomy, and in 14 patients the authors found no abnormalities to suggest acute infarctions. Although they concluded that the data supported the safety of this type of surgery, there were a limited number of patients studied. Conversely, another presentation described 15 patients imaged 12 hours after carotid endarterectomy, and two of them showed new, single, clinically silent infarctions involving the cortex. In a presentation in which MR perfusion was used in patients who underwent carotid endarterectomy, CBV and CBF were found to be increased after surgery. MR offers the possibility of evaluating the anatomy and physiologic results of such surgery. Patients who undergo heart surgery for artificial valve placement may show susceptibility artifacts on brain MR images, a finding observed with both prosthetic and metallic valves; minute metallic seeding from the valve or from surgical instruments is believed to be responsible.
Techniques in diffusion-weighted imaging were scrutinized in a number of presentations. The use of high b values (3000 s/mm2) resulted in lower signal-to-noise and contrast-to-noise ratios in acute cerebral infarctions, an observation that needs to be confirmed in acute infarctions. Similar observations were presented in a poster in which the brain was imaged with diffusion-weighted imaging using b values up to 5000 s/mm2. It was found that the increasing contrast may potentially limit identification of infarctions, but may be useful for white matter abnormalities. In a series of 26 subacute infarcts (with a mean of 4 days) all infarcts were hyperintense on b = 1000 and b = 3000 s/mm2 images. Lesion-to-brain contrast was higher at b = 3000 s/mm2 (29%), but the signal-to-noise and contrast-to-noise ratios were much lower. It was pointed out that biological systems have barriers to the movement of water (eg, semipermeable cell membranes), and diffusion-weighted imaging is in some sense a measure of these barriers. Increasing b values allow for the sensitization of the image to decreasing amounts of water molecule movement and, therefore, to smaller microscopic structures. In order to study intracellular structures, extremely high b values would be necessary, and this might be feasible in the future. These results suggest that perhaps in the future, different b values may be found to be helpful in the study of specific diseases.
In diffusion tensor imaging (DTI), the anisotropy of water motion is studied rather than negated. In order to be able to measure this anisotropy, the diffusion gradient in at least six (rather than three) directions must be obtained. This is accomplished by turning on the sensitizing gradients in various combinations. DTI data take longer to collect and require more postprocessing, but this technique was used in a number of presentations at this year's meeting. DTI can be used to measure the degree to which the normal microscopic order of white matter tracks is preserved. It was reported that in 12 patients with amyotrophic lateral sclerosis the degree of anisotropy in the posterior limb of the internal capsule was decreased from 0.20 to 0.15. This decrease was most marked in the region containing the corticospinal track (the anterior 1/3 of the posterior limb of the internal capsule). Pulse sequence parameters may affect quantitative information obtained from DTI. The ADC was affected by both the maximum strength and number of b values, whereas fractional anisotropy was not affected by these sequence parameters. Standard deviations were variably affected. This information may prove important when comparison of data from different studies is attempted.
Means of improving MR angiography (MRA) are always topics of great interest because of the desire to assess accurately, but noninvasively, extra- and intracranial vessels. With fluoroscopically triggered gadolinium-enhanced MR, angiography images were obtained in 50 patients; the authors concluded that when the underlying stenoses are greater than 70% by sonography, this MR technique is very sensitive and specific in the assessment of vessels. The possibility of performing such studies is becoming widespread because many MR vendors now offer units with higher strength (40 mT) gradients. In another study, the size of the artifact induced by titanium aneurysm clips was quantified. The authors concluded that residual or regrowth of aneurysms must be larger than 5.2 mm in diameter before they become visible on standard MR angiograms.
Characterizing brain tumors by newer MR techniques was a topic of a number of papers. Most studies are performed at 1.5 T, although diagnostic spectra obtained at 0.5 T were shown at the meeting. Results obtained at higher field strength (33–34 T) should be valuable because of an improved signal-to-noise ratio, better separation of peaks, and the potential for imaging other nuclei. With MRS, myo-inositol on short TE proton MRS was shown to correlate well with the grade of malignancy (higher myo-inositol in low-grade gliomas, lower myo-inositol in high-grade gliomas). This observation may be particularly helpful in tumors such as pilocytic astrocytomas, which have elevated metabolites (eg, choline and lactate) despite their benign nature. In another presentation, brain tumor growth was reflected by an elevation of choline, a decrease in the ADC, and increased perfusion. The combination of these techniques may allow better monitoring of the effects of therapy on brain tumors, and probably is better than any single technique. Other authors found high ADC and CBV values in high-grade gliomas, observations that may be important in planning biopsy targets, resection, and focused radiation therapy. The use of diffusion-weighted imaging to monitor the response of brain lymphoma to chemotherapy showed that ADC changes preceded changes on contrast-enhanced images; however, the study of a larger number of patients is required for validation of this observation. With the use of MRS to evaluate patients who had received whole-brain radiation as part of their treatment for leukemia, it was found that even after 10 years, metabolic abnormalities were still present. An attempt to differentiate lymphoma and toxoplasmosis in patients with AIDS revealed that toxoplasma regions were bright on diffusion-weighted images, whereas the necrotic components of several lymphomas were of low signal intensity; this finding is similar to that reported in malignant brain tumors versus cerebral abscesses.
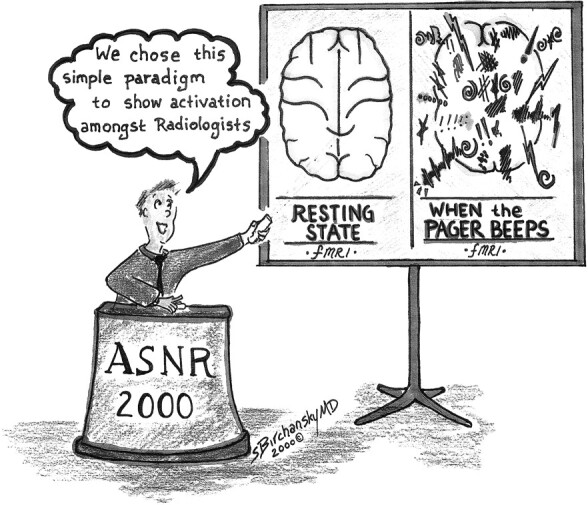
Increasing interest in fMR imaging, along with the number of papers dealing with fMR, clearly showed the power of this emerging technique. Blood oxygenation level–dependent fMR imaging is still the most commonly used technique for performance activation studies, although flow-sensitive alternating inversion-recovery imaging has been used to evaluate changes in tissue perfusion as well. The resting perfusion of the superior temporal gyrus was measured in 26 deaf patients and compared to 15 hearing patients. There was evidence of perfusion (and therefore presumed electrical activity) in the superior temporal gyrus in both groups, and differences between the groups did not reach statistical significance. A phantom study revealed that small amounts of motion (submillimeter) that are only modestly correlated with a simulated activation study (r > 67) produced false activation in nearly all experiments. Brain stem nucleus activation could be identified on coronal images, sagittal images, or both, with motor and sensory paradigms (eg, eye movement, face brushing, taste) in six healthy volunteers. fMR imaging, used to assess the visual cortex as a function of luminance in patients with multiple sclerosis, showed less visual cortex activation in patients with multiple sclerosis than in control subjects, an observation reflecting the predilection of this disease to involve the optic radiations. Again, using visual activation, it was shown that specific areas of the optic apparatus are involved in different visual deficits, ie, patients with amblyopia showed ipsilateral prechiasmal optic nerve atrophy, whereas patients with retinal degeneration showed pericalcarinee, chiasmatic, and optic nerve atrophy. Similar observations have been reported in patients with anophthalmos and microphthalmos, and it is possible that injuries at the level of the globe result in diffuse transneuronal degeneration of the optic apparatus. In fMR imaging studies of the mesial temporal lobes, it was shown that these regions play major roles in visual memory and navigation; this information may be critical for temporal lobectomies and may become important in assessing patients with diseases that preferentially involve this region, such as Alzheimer's disease.
The head and neck portion of the meeting included a symposium featuring cranial nerve anatomy and disease, and the skull base and clivus. The audience was treated to a detailed description of the normal anatomy of the trigeminal nerve, including its distal branches within the oral cavity and mandible. The images were some of the most impressive ever shown at a national meeting, and clearly illustrated that distal branches of the nerve could be visualized with the proper surface coil imaging technique. The anatomy and pathologic abnormalities of cranial nerves VIII through XII were presented in detail. Note was made of the “double eagle” sign of the hypoglossal canal, as seen in the coronal plane. The approach to evaluation of patients with cranial nerve VIII dysfunction was presented, and lesions that produce facial palsy and may be easily overlooked, such as temporal bone hemangioma, were stressed. The important issue of perineural spread of tumors from head and neck malignancies was reviewed, and the use of contrast-enhanced MR imaging in detecting subtle spread of tumor beyond the primary tumor site was shown.
The opening session of the pediatric portion of the meeting dealt with the care and management of the pediatric patient undergoing neuroimaging procedures. The challenge of successful imaging augmented by safe sedation practices was emphasized. A safe pediatric sedation program requiring advanced planning to assure adequate site requirements, availability of pediatric resuscitation equipment and medications, and continual supervision by trained physicians and nursing staff was stressed. The components of a complete sedation program, proper monitoring, staff education in basic and advanced life support, and pharmacologic practices were discussed.
Scientific sessions focused in part on advanced imaging methods in pediatric neuroimaging. A study of MRS ratios in healthy children using stimulated-echo acquisition mode sequences found significantly lower N-acetylaspartate/creatine (NAA/Cr) ratios, and higher choline (Cho)/Cr and myo-inositol/Cr ratios from the temporal lobe allocortex voxels than from the parietal or frontal lobe isocortex. Other studies found similar long-TE point-resolved MRS ratios in healthy and developmentally delayed children younger than 2 years. Older developmentally delayed children with normal MR imaging had ratios like those of younger children, including lower NAA/Cr and elevated Cho/Cr ratios. This study indicated that MRS may be a sensitive marker for developmental delay. A study of long-TE point-resolved MRS ratios in children with and without mitochondrial disease, who underwent an intravenous challenge with 5 mL/kg of Ringer's lactate, found increased lactate in those children whose baseline MRS study revealed lactate. Thus, it was felt that a Ringer's lactate challenge might aid diagnosis of mitochondrial disease apart from other causes of lactic acidosis. Another study illustrated exquisite anatomic detail by use of fast MR for fetal CNS anomalies indicated by sonography. A study of line-scan diffusion imaging of spinal lesions revealed diagnostic image quality without the magnetic susceptibility and motion artifacts that are problematic with other diffusion techniques.
A symposium on cerebrovascular disease reviewed the complex risk factors and presentation of children with stroke. With a thorough evaluation, which often includes noninvasive imaging and angiography, the underlying source can be identified in about 75% of patients. Although symptomatic cerebral aneurysms do not often arise in childhood, genetic factors such as mutation and polymorphism are now implicated in aneurysm development. Other factors include abnormal expression of angiogenetic factors, especially in saccular aneurysms. Familial patterns of intracranial aneurysm with early rupture and continuing development of new lesions have recently been described. Immune deficiencies predispose to fusiform vasculopathy in childhood. Advanced imaging techniques including diffusion, perfusion, MRA, and MRS were shown to be of value in the diagnosis and monitoring of treatment of children with cerebrovascular disease, although technique modifications are required for infants and young children. Demonstration of focal lactate in areas of signal abnormality on MRS images favors anaerobic metabolism and infarction. In young infants and children, diffusion imaging abnormalities caused by global brain injury from hypoxia-asphyxia may not appear for 18–24 hours after the event. Whether this represents masking of early diffusion changes by immature myelination, vasogenic edema, or delayed cellular injury is uncertain. If this finding represents delayed development of irreversible cellular injury, then a longer therapeutic window for intervention is a possibility. Focal cerebrovascular lesions in children follow a similar pattern and time course as seen in adults. Early data suggest that higher b value diffusion imaging offers greater lesion-to-brain contrast and a reduced signal-to-noise ratio, and does not offer earlier lesion detection.
Additional presentations on cerebrovascular disease in children included a prospective study of silent infarction in sickle cell disease from infancy into childhood. The prevalence of silent infarction was 58/249 cases or 23.3%; an average of 12.1% of silent infarction subjects had a new or progressive lesion within 2 years. Another study in infants with hypoxia found similar sensitivity but superior specificity for MRS compared to diffusion-weighted imaging. Patterns of hypoxic-ischemic injury were diffuse white matter, diffuse gray matter, diffuse gray and white matter, and patchy multifocal lesions. Investigators reported pilot results of a perfusion-sensitive, noncontrast MR technique using acquisition of four diffusion image sets with varied low-value b factors, based on the idea that low b factors map perfusion, whereas high b values reveal diffusing protons. Diffusion imaging may have a role in assessing interstitial edema in obstructive hydrocephalus; specifically, a comparison of average diffusion constants in periventricular white matter prior to and after therapy found increased values at preshunting and decreased values after surgery (n = 10). This technique may prove helpful in monitoring results of surgery.
The scientific session on congenital and metabolic disorders included a retrospective study of 42 patients with holoprosencephaly. Varying degrees of noncleavage of the caudate and hypothalamus were nearly universal, whereas noncleavage of the lentiform nuclei and thalami was less common (64%). A computerized technique for callosal measurement and morphometry in children with periventricular leukomalacia identified a smaller callosum than in control subjects, with the posterior callosum most severely affected. In children with the most severe motor impairment, the posterior callosum was significantly smaller than in those with mild impairment, suggesting that callosal morphometric analysis may serve as a marker of the severity of clinical impairment. A study of the presence of contrast enhancement and disease progression in patients with x-linked adrenoleukodystrophy showed a disease progression rate of 86% in patients with contrast enhancement, whereas 82% of patients without enhancement were stable. A study of 14 patients with early-onset combined methylmalonic aciduria and homocystinuria reported three diverse patterns of MR findings: supratentorial atrophy, infarction, and gliosis in the lenticulostriate area with MRA-revealed arteriopathy and tetraventricular hydrocephalus. Two studies suggested a role for diffusion imaging in mapping the loss of anisotropy and pathologic white matter lesions in adrenoleukodystrophy.
Neurocognitive disorders in childhood were discussed in a morning focus session. Structural imaging in autism showed cerebellar, cerebral, and limbic developmental abnormalities, and in combination with fMR imaging, demonstrable aberrant motor and cognitive activation patterns may help in understanding this disorder. The developing field of fMR imaging for assessment of children with language and reading impairment suggests that we may soon have an objective tool for the evaluation and classification of children with learning and language disorders.
The final scientific session focussed on pediatric functional imaging, epilepsy, and general pediatric neuroradiology topics. Short-TE MR spectra from tubers in tuberous sclerosis patients were reported to have elevated myo-inositol, macromolecules, and amino acids with slight NAA reduction. Children with acute onset of seizures may have hippocampal abnormalities on diffusion-weighted images that may not be apparent on T2-weighted or fluid-attenuated inversion-recovery images. Whether this finding reflects seizure-associated hypoxia or a hippocampal metabolic abnormality resulting in seizures was uncertain. A series of four young children with seizures who had coexisting cortical dysplasia and low-grade neoplasia was reported. A prospective MRS study of children with bipolar affective disorder found elevated glutamate in both frontal lobes and basal ganglia compared to healthy children, raising the possibility of an MRS signature for this disease.
The annual meeting was adjourned at noon on April 8th by President Bill Ball. The society looks forward to its 39th annual meeting, which will be held from April 21 through April 27, 2001 at the Hynes Convention Center in Boston, Massachusetts.