Abstract
Diabetic nephropathy (DN) is a common chronic complication of diabetes, for which acute glucose fluctuation (AGF) is a potential risk factor. Fluctuating hyperglycemia has been confirmed to induce more serious kidney damage than hyperglycemia in diabetic rats; however, the mechanism remains unknown. The purpose of this study was to explore the potential role of AGF in the progression of DN. Viability of rat podocytes following 72-h AGF treatment was detected using Cell Counting-Kit-8. The rates of apoptosis and the level of reactive oxygen species (ROS) in rat podocytes were assessed by flow cytometry. Western blotting and reverse transcription-quantitative PCR were performed to measure relative protein and mRNA expression levels, respectively. Transfection with an mRFP-GFP-LC3 adenoviral vector was used to track autophagic flux under confocal microscopy. The results indicated that AGF could inhibit cell proliferation, promote TNF-α, interleukin-1β (IL-1β), and reactive oxygen species (ROS) generation, and increase autophagy in rat podocytes. Moreover, AGF upregulated receptor for advanced glycation end products (RAGE) expression via activation of NF-κB/p65 and IκBα. Pretreatment with 5 mM N-Acetyl-L-cysteine or 10 µM pyrrolidine dithiocarbamate effectively reduced cellular damage and inhibited activation of the NF-κB/RAGE signaling pathway. Thus, AGF induces rat podocyte injury by aggravating oxidative stress, promoting the inflammatory response, and regulating ROS-mediated NF-κB/RAGE activation.
Keywords: diabetes, acute glucose fluctuation, diabetic nephropathy, autophagy, RAGE, oxidative stress
Introduction
Diabetes mellitus is a common disease characterized by dysregulated blood glucose homeostasis, and has reached pandemic-proportion levels worldwide (1). Diabetic nephropathy (DN), identified as a life-threatening microvascular complication of diabetes, is the leading cause of end-stage renal disease (ESRD) (2). DN is caused by excessive precipitation of extracellular matrix (ECM) proteins, which results in glomerular hypertrophy and expansion, effacement of podocyte foot processes, and inflammatory cell infiltration (3). Podocytes are highly differentiated epithelial cells with extensive foot processes, and their progressive injury plays a vital role in the deterioration of glomerular function and albuminuria (4,5).
Emerging evidence shows that different mechanisms contribute to the pathogenic progression of DN, including oxidative stress, excessive accumulation of advanced glycation end-products (AGEs), and inflammation (6). AGE induces tissue injury through alterations in the extracellular matrix architecture and interactions with the receptor for advanced glycation end products (RAGE) (7). RAGE is expressed on normal podocytes; however, its expression is abnormally upregulated in DN. Excessive ROS generation is implicated in the activation of NF-κB, which upregulates RAGE expression, resulting in chronic inflammation, aggravation of cellular dysfunction, and increased tissue damage (8,9). The transcription and production of pro-inflammatory cytokines (such as TNF-α and IL-1β) in podocytes contribute to the development of DN.
Autophagy is the major mechanism by which podocytes regulate cellular homeostasis, enabling the cells to degrade oxidatively damaged or surplus organelles in autolysosomes (10). Autophagy disorders play a critical role in a wide range of human pathologies. Moreover, autophagy plays a dual function in maintaining cellular homeostasis, as both defective autophagy and excessive autophagy are associated with cellular dysfunctions preceding cell death (11). Various detrimental factors, including oxidative stress, mitochondrial dysfunction, and inflammatory reactions can lead to autophagic cell injury (12). In addition, podocytes have higher basal levels of autophagy under physiological conditions, suggesting that autophagy is an important mechanism by which podocytes maintain homeostasis (13). Although several cell types demonstrate a basal level of autophagy, autophagy can be further activated to promote cellular survival in response to various forms of cellular stress, such as oxidative stress or hypoxia (14).
Glucose variability represents a novel latent risk factor for diabetes mellitus that consists of two aspects, namely, the extent of blood glucose fluctuations and the time intervals during which these fluctuations occur (15). Evidence suggests that acute glucose fluctuation (AGF) may be more harmful than sustained hyperglycemia regarding the risk of developing diabetic complications (16). Moreover, studies have shown that intermittent hyperglycemia exposure induces more severe oxidative stress than constant exposure to hyperglycemia (17,18). AGF has been confirmed to accelerate renal damage in diabetic rats (19). However, its impact on rat podocytes is poorly understood.
Although our previous study revealed that fluctuating hyperglycemia induces more severe inflammatory damage than hyperglycemia in diabetic rats, the associated mechanism remains unknown (20). In this study, the effects of AGF were evaluated in rat podocytes in order to elucidate further potential mechanisms of injury caused by glucose variability.
Materials and methods
Cell culture and treatment
A rat podocyte cell line was obtained from Beijing Wormhole Space Information Technology Co., Ltd. Rat podocytes were cultured in DMEM/F12 culture medium (Hyclone; Cytiva) supplemented with 10% FBS (Gibco; Thermo Fisher Scientific, Inc.) at 37°C in a humidified incubator with 5% CO2.
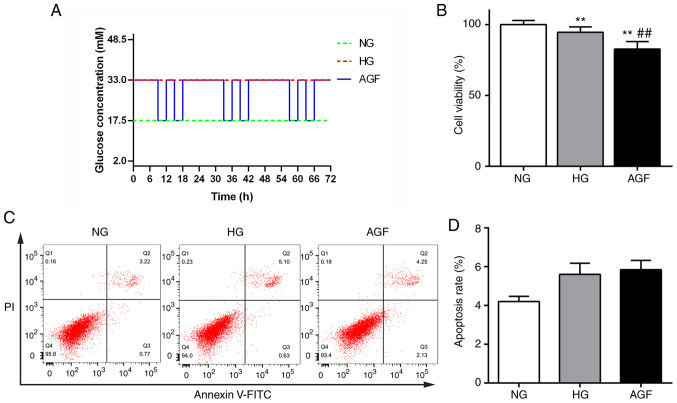
Cells were divided into three groups: i) Normal glucose group (NG), cells incubated in culture medium with 17.5 mM D-glucose; ii) high-glucose group (HG), cells incubated in culture medium with 33 mM D-glucose; and iii) AGF, 17.5 and 33 mM D-glucose culture medium were alternated every 3 h twice daily, with the final incubation carried out overnight in 33 mM D-glucose culture medium. The cells were maintained at the required conditions for 72 h, as shown in Fig. 1A.
Figure 1.
Effect of acute blood fluctuation on rat podocyte proliferation and apoptosis. (A) Schematic diagram showing the experimental design for acute glucose fluctuation treatment in vitro. Rat podocytes were maintained under the required conditions for 72 h. (B) Cell viability was measured using a Cell Counting Kit-8 assay. (C and D) Apoptosis rate of the rat podocytes was assessed using flow cytometry using an Annexin-V/PI apoptosis kit. Data are presented as the mean ± SD. n=3. **P<0.01 vs. NG group; ##P<0.01 vs. HG group. AGF, acute glucose fluctuation; NG, normal glucose; HG, high glucose; FITC, fluorescein isothiocyanate; PI, propidium iodide.
In a separate experiment, rat podocytes were pre-treated with 5 mM N-Acetyl-L-cysteine (NAC) or 10 µM pyrrolidine dithiocarbamate (PDTC) (both Beyotime Institute of Biotechnology) for 30 min and then treated with the aforementioned conditions for 72 h, as shown in Fig. 1A.
Cell viability assays
The effects of AGF treatment on cell viability were measured using a Cell Counting Kit-8 (Beyotime Institute of Biotechnology). Rat podocytes were seeded into 96-well plates (Corning, Inc.) at a density of 3×104 cells/ml with 100 µl culture medium per well, then cultured for 24 h. After 72 h of NG, HG or AGF treatment, the culture medium was replaced with 100 µl fresh culture medium, and 10 µl CCK-8 solution was added to each well. After incubating the cells for 1 h, the absorbance was detected at 450 nm.
Cell apoptosis
Cell apoptosis was assessed with an Annexin V-fluorescein isothiocyanate (FITC)/propidium iodide (PI) detection kit (Dojindo Molecular Technologies, Inc.). Rat podocytes were plated in six-well plates (Corning, Inc.) at a density of 3×105 cells/ml with 1 ml culture medium per well, then cultured for 24 h. After 72 h of treatment, the rat podocytes were digested with 0.25% trypsin and gently washed with PBS. The single-cell suspension was incubated with 5 µl Annexin V-FITC and 5 µl PI in 100 µl binding buffer solution for 15 min at room temperature in the dark. Next, 400 µl Annexin V binding buffer was added, and apoptotic cells were detected using a FACSCanto II flow cytometer (BD Biosciences) within 1 h. The apoptosis rates were analyzed using FlowJo software (version 10.0.7r2; FlowJo LLC).
MRFP-GFP-LC3 assay
The adenovirus encoding mRFP-GFP-LC3 was purchased from Hanbio Biotechnology Co., Ltd. (cat. no. HBAD-1007). To monitor autophagic flux, rat podocytes were grown to 80% confluence, and transfected with adenoviral particles at 50 MOI in serum-free medium at 37°C for 24 h. After 72-h NG, HG or AGF treatment, the cells were fixed with 4% paraformaldehyde for 30 min and the cell nuclei was stained with DAPI solution for 10 min at room temperature. Fluorescent images were captured with a confocal microscope (Carl Zeiss, Inc.). Images were acquired using a microscopic system (magnification, ×630). GFP fluorescence is quenched under acidic conditions, and an increase in both yellow and red spots represent enhanced autophagic flux. The number of autolysosomes (red dots) and autophagosomes (yellow dots) was quantified to evaluate autophagic flux using Image-J software (version 1.51j8; National Institutes of Health).
Measurement of cellular ROS levels
The level of intracellular ROS in the rat podocytes was assessed using a 2′,7′-Dichlorofluorescin diacetate (DCFH-DA) fluorescent probe (cat. no. D6470; Beijing Solarbio Science & Technology Co., Ltd.). Following 72 h NG, HG or AGF treatment, the podocytes were stained with 10 µM DCFH-DA for 60 min at room temperature in the dark. The rat podocytes were digested with 0.25% pancreatin and washed with PBS. The mean fluorescence intensity was analyzed by FACSCanto II flow cytometry (BD Biosciences, Inc.). A total of 10,000 events were collected for each group, and the relative ROS levels were analyzed using FlowJo software (version 10.0.7r2; FlowJo LLC).
Western blotting
The cells were resuspended in RIPA lysis buffer (Beyotime Institute of Biotechnology). The protein concentrations were determined using a BCA kit (Beyotime Institute of Biotechnology) and an equal amount of total protein (30 µg) was separated by 10 or 12% SDS-PAGE and transferred to PVDF membranes (EMD Millipore). The membranes were blocked in 5% non-fat milk in TBST buffer for 30 min and incubated with the primary antibodies overnight at 4°C. The following primary antibodies were used: anti-TNF-α antibody (1:500; cat. no. 11948T; Cell Signaling Technology, Inc.), anti-LC3B antibody (1:1,000; cat. no. 3868s; Cell Signaling Technology, Inc.), anti-Beclin-1 antibody (1:1,000; cat. no. 3495s; Cell Signaling Technology, Inc.), anti-RAGE antibody (1:1,000; cat. no. sc-80652; Santa Cruz Biotechnology, Inc.), anti-phosphorylated (p)-NF-κB p65 antibody (1:1,000; cat. no. 3033; Cell Signaling Technology, Inc.), anti-NF-κB p65 antibody (1:1,000; cat. no. 4765; Cell Signaling Technology, Inc.), anti-p-IκB-α antibody (1:1,000; cat. no. 9246s; Cell Signaling Technology, Inc.), anti-IκB-α antibody (1:1,000; cat. no. 9242s; Cell Signaling Technology, Inc.), anti-IL-1β antibody (1:500; cat. no. 12703T; Cell Signaling Technology, Inc.), and anti-GAPDH antibody (1:1,000; cat. no. 5174; Cell Signaling Technology Inc.). The next day, the membranes were then probed with corresponding HRP-conjugated goat anti-rabbit IgG (1:2,000; cat. no. 14708; Cell Signaling Technology, Inc.) and anti-mouse IgG (1:2,000; cat. no. 7076; Cell Signaling Technology, Inc.) secondary antibodies for 90 min at room temperature. The bands were visualized using an ECL reagent (Biological Industries, Inc.) and recorded on X-ray film. The densitometry of each band was analyzed using ImageJ software (version 1.51j8; National Institutes of Health).
Reverse transcription-quantitative PCR (RT-qPCR)
Total RNA was isolated from rat podocytes from each group using RNAiso reagent (Beijing Solarbio Science & Technology Co., Ltd.). The concentration of total RNA was quantified using a NanoDrop™ 2000 spectrometer (NanoDrop Technologies; Thermo Fisher Scientific, Inc.). The RNA was reverse transcribed to synthesize cDNA using a PrimeScript™ RT reagent kit (Takara Bio, Inc.; 16°C for 30 min, 42°C for 30 min and 85°C for 5 min). The amplification of cDNA was performed with a TB Green PCR kit (Beijing Solarbio Science & Technology Co., Ltd.). qPCR was carried out on a LightCycler® 480 system (Roche Diagnostics). The primers were designed by Sangon Biotech Co. Ltd. The reaction conditions included an initial denaturation at 95°C for 10 min, followed by 40 cycles at 95°C for 15 sec and at 60°C for 60 sec. The primer sequences were as follows: GAPDH forward, 5′-GACATGCCGCCTGGAGAAAC-3′ and reverse, 5′-AGCCCAGGATGCCCTTTAGT-3′; IL-1β forward, 5′-CTCACAGCAGCATCTCGACAAGAG-3′ and reverse, 5′-TCCACGGGCAAGACATAGGTAGC-3′; TNF-α forward, 5′-TCCACGGGCAAGACATAGGTAGC-3′ and reverse, 5′-GCTCCTCCGCTTGGTGGTTTG-3′; RAGE forward, 5′-CTGCCTCTGAACTCACAGCCAATG-3′ and reverse, 5′-TCCTGGTCTCCTCCTTCACAACTG-3′. GAPDH was used as a housekeeping gene control. Relative gene expression were measured using the 2−∆∆Cq method (21).
Statistical analysis
Data are presented as the mean ± standard deviation. Comparisons between two groups were analyzed using Student's t-test, and multiple comparisons were analyzed using one-way ANOVA followed by Tukey's post hoc test. All graphs in this study were generated with GraphPad Prism 6.0 (GraphPad Software. Inc.). P<0.05 was considered to indicate the final version of the manuscript.
Results
Impact of acute glucose fluctuations on rat podocyte viability and apoptosis
The effect of AGF treatment on cell viability was measured using a CCK-8 kit. The viability of cells in the HG group significantly decreased compared with that of the NG group (P<0.01). Moreover, cell viability in the AGF group was significantly reduced compared with the NG and HG groups (P<0.01). These data indicated that AGF significantly inhibited the viability of rat podocytes (Fig. 1B). Changes in apoptosis were detected by flow cytometry, and no significant difference between the groups was observed (P>0.05; Fig. 1C and D).
Acute glucose fluctuation promotes rat podocyte autophagy
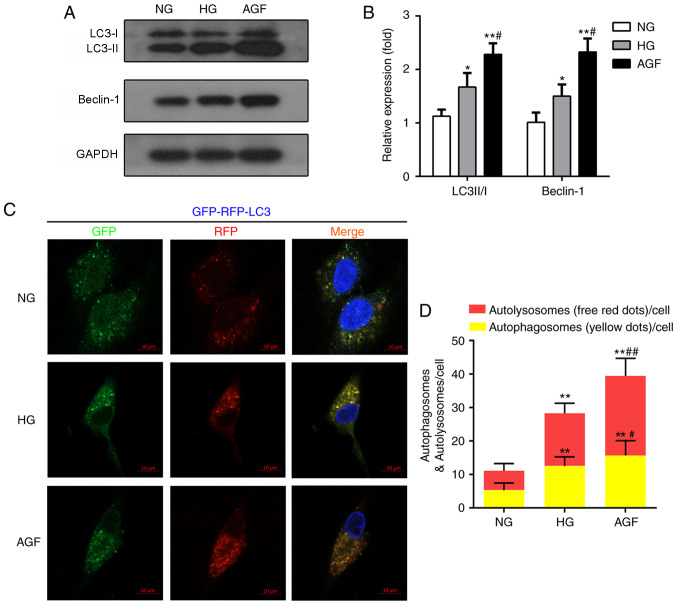
Autophagy is also involved in the maintenance of podocyte function and cell homeostasis (22). To define the AGF-induced alterations in autophagy, the expression levels of autophagy biomarkers (LC3II/I and Beclin-1) were evaluated by western blotting. The AGF group exhibited enhanced LC3II/I and Beclin-1 expression levels, compared with the NG (P<0.01) and HG groups (P<0.05; Fig. 2A and B). To further confirm the effects of AGF on autophagy flux, rat podocytes were transfected with an mRFP-GFP-LC3B adenovirus vector, then treated with NG, HG or AGF and observed by confocal microscopy. Compared with the NG group, HG group exhibited a significant increase in the abundance of yellow and red puncta (P<0.01), suggesting an increase in autophagy in HG-treated cells. The number of yellow and red puncta was further enhanced by AGF compared with the HG group (P<0.05; Fig. 2C and D).
Figure 2.
AGF induces autophagy in rat podocytes. (A and B) Protein levels of LC3II/I and beclin-1 expression was examined by western blotting. (C and D) Representative fluorescence images of mRFP-LC3 (autolysosomes) and merged RFP-GFP-LC3 (autophagosomes). In green and red-merged images, autophagosomes are shown as yellow puncta (GFP+ mRFP+), autolysosomes are shown as red puncta (GFP− mRFP+), and blue fluorescence represents DAPI-treated nuclei. (D) Image analysis of red puncta (autolysosomes) and yellow puncta (autophagosomes). n=3. *P<0.05; **P<0.01 vs. NG; #P<0.05; ##P<0.01 vs. HG. AGF, acute glucose fluctuation; NG, normal glucose; HG, high glucose; GFP, green fluorescence protein; RFP, red fluorescence protein.
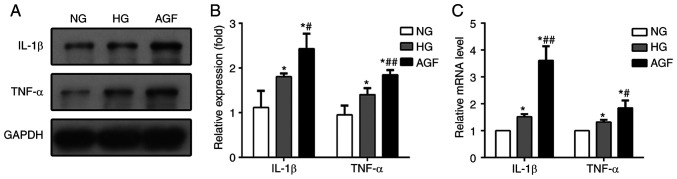
Acute glucose fluctuation promotes IL-1β and TNF-α generation in rat podocytes
In our previous study, AGF aggravated inflammatory lesions in diabetic rats (19). To test whether AGF could elevate the generation of inflammatory lesions in vitro, we determined the mRNA and protein expression of levels of TNF-α and IL-1β in treated rat podocytes. The expression of both of these pro-inflammatory cytokines were higher in the HG and AGF group compared with the NG group (P<0.05), and significantly increased in the AGF group compared with the HG group, both at the mRNA and protein levels (P<0.05; Fig. 3). These results indicated that AGF aggravated the inflammatory response in rat podocytes.
Figure 3.
AGF promotes pro-inflammatory cytokine generation. (A and B) Protein and (C) mRNA expression levels of TNF-α and IL-1β. Data are presented as the mean ± SD. n=3. *P<0.05 vs. NG; #P<0.05, ##P<0.01 vs. HG. AGF, acute glucose fluctuation; NG, normal glucose; HG, high glucose.
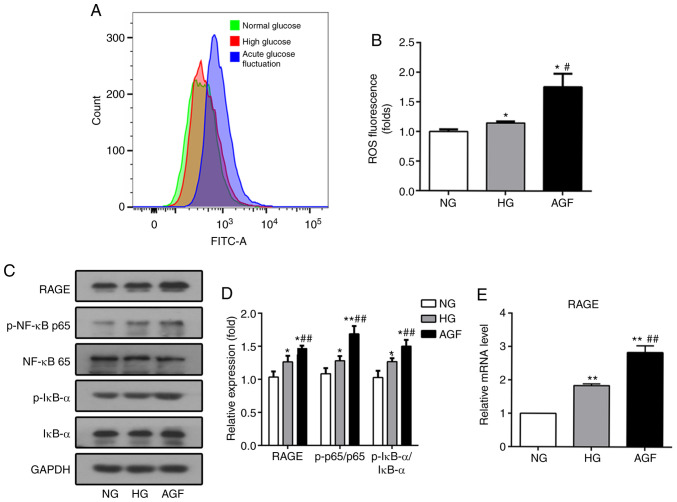
Acute glucose fluctuation increases ROS levels and activates the RAGE/NF-κB signaling pathway in rat podocytes
TNF-α plays a central role in mediating renal injury though the induction of ROS production (14). After 72 h of AGF treatment, the levels of intracellular ROS in rat podocytes was significantly increased, compared with the NG and HG groups (P<0.05; Fig. 4A and B).
Figure 4.
AGF increases the level of intracellular ROS and RAGE expression, as well as enhances the phosphorylation of p-NF-κB p65 and p-IκB-α expression in rat podocytes. (A and B) Flow cytometry analysis of intracellular ROS production. (C and D) The level of RAGE, p-NF-κB p65, NF-κB p65, p-IκB-α, and IκB-α were examined by western blotting. (E) The level of RAGE mRNA was examined by qRT-PCR. Data are presented as the mean ± SD. n=3. *P<0.05; **P<0.01 vs. NG; #P<0.05, ##P<0.01 vs. HG. AGF, acute glucose fluctuation; NG, normal glucose; HG, high glucose; FITC, fluorescein isothiocyanate; RAGE, receptor for advanced glycation end products.
In addition, inflammatory stimulation can increase the levels of RAGE transcription via the binding of NF-κB to the RAGE promoter region, which results in increased RAGE expression (23). To confirm whether AGF can regulate the RAGE/NF-κB signaling pathway, the expression levels of RAGE, p-NF-κB p65, NF-κB p65, p-IκBα, and IκBα were determined. AGF induced a significant increase in RAGE expression compared with the NG or HG group (P<0.05; Fig. 4C and E). Phosphorylation of NF-κB p65 and IκBα was significantly upregulated following AGF treatment compared with the NG or HG groups (P<0.05; Fig. 4C and D). This finding suggested that could AGF activate the NF-κB signaling pathway in rat podocytes.
Downregulation of intracellular ROS levels inhibits the NF-κB/RAGE signaling pathway in rat podocytes
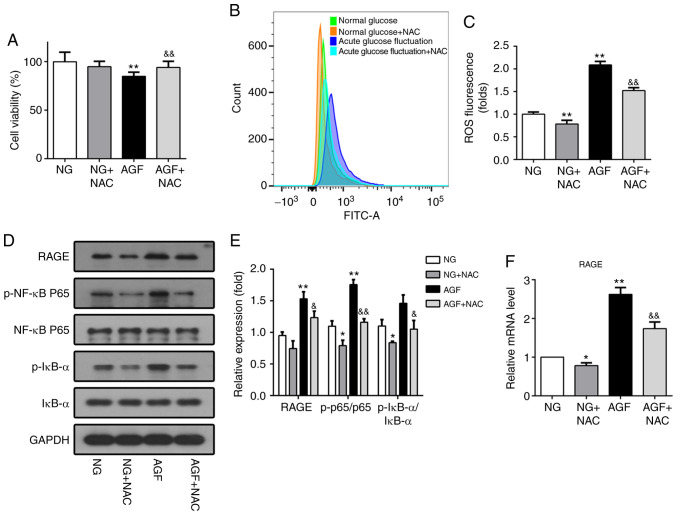
NAC, a ROS inhibitor, was used to further confirm whether ROS affects the NF-κB/RAGE signaling pathway in response to AGF. NAC pretreatment reversed the effect of AGF treatment, as cell viability was found to be significantly higher compared with that of the AGF group (P<0.01; Fig. 5A). Moreover, the level of AGF-induced intracellular ROS was significantly reduced following pretreatment with NAC (P<0.01; Fig 5B and C). Subsequent western blot and RT-qPCR analysis demonstrated that NAC significantly inhibited the phosphorylation of NF-κB p65 and IκBα (P<0.05) and decreased RAGE expression induced by AGF (P<0.05; Fig. 5D-F). These results confirm the role of ROS in the NF-κB/RAGE signaling pathway.
Figure 5.
Downregulation of intracellular ROS levels inhibits activation of the NF-κB/RAGE signaling pathway in rat podocytes. (A) Cell viability was measured using a Cell-Counting-Kit-8 assay. (B and C) ROS generation induced by AGF in rat podocytes with or without 5 mM NAC pretreatment. (D and E) Protein levels of RAGE, p-NF-κB p65, NF-κB p65, p-IκB-α, and IκB-α. (F) mRNA levels of RAGE. Data are presented as the mean ± SD. n=3. *P<0.05, **P<0.01 vs. NG; &P<0.05, &&P<0.01 vs. HG. AGF, acute glucose fluctuation; NG, normal glucose; HG, high glucose; FITC, fluorescein isothiocyanate; RAGE, receptor for advanced glycation end products; ROS, reactive oxygen species; NAC, N-Acetyl-L-cysteine; p, phosphorylated.
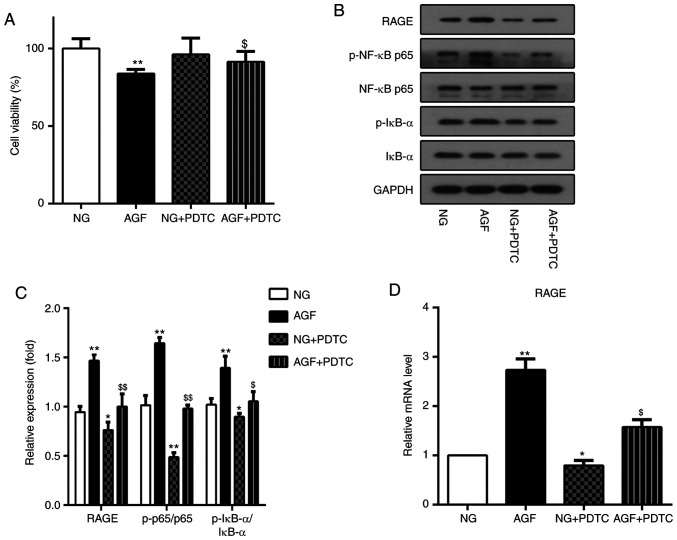
Inhibition of NF-κB by PDTC reduces the AGF-induced increase in RAGE expression in rat podocytes. PDTC is an inhibitor of the NF-κB signaling pathway. To further investigate the relationship between AGF-induced increases in RAGE expression and activation of the NF-κB signal pathway, PDTC was used to inhibit the NF-κB signal pathway in rat podocytes. The effect of PDTC on cell viability was first measured. The AGF+PDTC group exhibited significantly improved cell viability compared with that of the AGF group (P<0.05; Fig. 6A). Next, the level of RAGE expression, as well as the ratio of p-NF-κB p65/NF-κB p65 and p-IκB-a/IκBα were measured. The results showed that PDTC significantly inhibited the phosphorylation of NF-κB p65 and IκB-α (P<0.05), as well as the upregulation of RAGE protein expression induced by AGF (P<0.05; Fig. 6B-D). These data indicated that activation of the NF-κB signaling pathway was required for AGF-induced cell damage and increased RAGE expression levels in rat podocytes.
Figure 6.
Inhibition of NF-κB by PDTC reduced acute glucose fluctuation-induced increases in RAGE expression in rat podocytes. (A) Cell viability was measured using a CCK-8 assay. (B and C) Protein levels of RAGE, p-NF-κB p65, NF-κB p65, p-IκB-α and IκB-α. (D) mRNA levels of RAGE. Data are presented as the mean ± SD. n=3. *P<0.05, **P<0.01 vs. NG group; $P<0.05, $$P<0.01 vs. AGF. AGF, acute glucose fluctuation; NG, normal glucose; HG, high glucose; FITC, fluorescein isothiocyanate; RAGE, receptor for advanced glycation end products; PTDC, pyrrolidinedithiocarbamate; p, phosphorylated.
Discussion
DN pathogenesis is highly complex and poorly understood. Hyperglycemia represents a major contributor in the occurrence of DN; however, current therapies remain limited and cannot completely prevent DN progression. Increasing evidence suggests that AGF induces more severe renal damage than sustained hyperglycemia (19,24). To confirm the role of AGF experimentally, our previous study involved changing the blood glucose levels of diabetic rats acutely through the injection of glucose and insulin (20). In this study, an in vitro model of AGF-induced podocyte injury. To simulate changes in the blood glucose of diabetic rat podocytes in vitro, the glucose concentration of the culture medium was altered at different time points.
Podocytes play an important role in the maintenance of the glomerular filtration barrier, and the decrease in podocyte number is associated with the progression of proteinuria (25). Therefore, the effect of glucose fluctuation on cell proliferation and apoptosis was examined. The results showed that there was a significant inhibition in cellular proliferation following AGF treatment. A decrease in viable cells was observed after 72 h of exposure to changes in the glucose concentration in the culture medium. However, the apoptosis rate measured by flow cytometry was not statistically significant, which is similar to the results of a study using human umbilical vein endothelial cells, which found that AGF failed to induce cell apoptosis (26). Extensive studies have indicated that apoptosis and proliferation are mediated by increased levels of ROS (27). ROS plays a dual role in tissue injury, as moderate levels of ROS promote cell survival and proliferation, whereas excessive ROS production can directly induce necrocytosis (28). In the present study, AGF generated more severe oxidative stress with increased level of intracellular ROS compared to hyperglycemia (Fig. 4).
Current evidence suggests that autophagy may mediate resistance to apoptosis (29). Similar to apoptosis, autophagy also plays a vital role in cellular proliferation and survival, and dysregulated autophagy activation has been described in several diseases (30). It is well-established that Beclin-1 and LC3 are important proteins in autophagy (31). The present results indicated that hyperglycemia caused an increase in the LC3-II/LC3-I ratio and a significant increase in the level of Beclin-1, demonstrating enhanced autophagy. As a cytoprotective function, autophagy is accompanied by ROS production (32). Podocytes may respond to higher ROS levels resulting from AGF by triggering autophagy protective mechanisms to prevent apoptosis. Therefore, AGF induces more autophagy in rat podocytes.
Additionally, various inflammatory responses were involved in AGF-induced podocyte injury. AGF significantly increased the generation of inflammatory lesions, including the production of IL-1β and TNF-α, consistent with the findings of our previous study (20). TNF-α has been confirmed to induce intracellular ROS production, but the detailed mechanisms remain unclear (33). A previous study indicated that an increase in ROS and TNF-α, in addition to inducing tissue damage, also contributes to the activation of NF-κB (34). An increase in the NADPH oxidase complex through NF-κB activation ultimately leads to enhanced ROS production and further NF-κB activation (35). Ultimately, such activation generates a vicious cycle that contributes to the progressive loss of renal function (36). AGF could also augment inflammatory responses through the activation of the NF-κB signaling pathway.
RAGE, the specific receptor for AGEs, plays a vital role in oxidative stress. Interactions between RAGE and AGEs activate various signaling pathways and subsequently induce oxidative stress and an inflammatory response, which leads to the pathological development of DN (37). Due to long-term hyperglycemia, diabetic patients accumulate a larger number of AGEs in vivo, and an excessive amount can increase RAGE expression. In addition, TNF-α is potent inducer of RAGE expression, and ROS-mediated RAGE induction occurs via NF-κB activation (38). Thus, we investigated whether AGF could upregulate RAGE expression. As expected, hyperglycemia increased the level of RAGE expression in rat podocytes, which was further promoted by AGF. This effect is likely related to higher levels of ROS, and the downstream transcription factor, NF-κB.
In conclusion, the present study demonstrates that acute glucose fluctuation induces rat podocyte injury by aggravating oxidative stress, enhancing the inflammatory response, and activating the RAGE/NF-κB signaling pathway. Therefore, the maintenance of a stable range of blood glucose fluctuation may help delay the development of DN.
Acknowledgements
Not applicable.
Funding Statement
This work was supported by The National Natural Science Foundation of China (grant no. 81973767).
Funding
This work was supported by The National Natural Science Foundation of China (grant no. 81973767).
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Authors' contributions
ZH and HW developed the aim of the study, participated in its design and coordination, and helped draft the manuscript. WF, YL, and HL contributed to the acquisition and interpretation of the data. WC provided critical review and substantially revised the manuscript. ZH and HW had seen all the raw data and confirmed the authenticity of data shown in the present manuscript. All authors read and approved the final manuscript.
Ethics approval and consent to participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Raja P, Maxwell AP, Brazil DP. The Potential of Albuminuria as a Biomarker of Diabetic Complications. Cardiovasc Drugs Ther. 2020 Jul 17; doi: 10.1007/s10557-020-07035-4. (Epub ahead of print). doi: 10.1007/s10557-020-07035-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lagies S, Pichler R, Bork T, Kaminski MM, Troendle K, Zimmermann S, Huber TB, Walz G, Lienkamp SS, Kammerer B. Impact of Diabetic Stress Conditions on Renal Cell Metabolome. Cells. 2019;8:8. doi: 10.3390/cells8101141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kato M, Natarajan R. Epigenetics and epigenomics in diabetic kidney disease and metabolic memory. Nat Rev Nephrol. 2019;15:327–345. doi: 10.1038/s41581-019-0135-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bork T, Liang W, Yamahara K, Lee P, Tian Z, Liu S, Schell C, Thedieck K, Hartleben B, Patel K, et al. Podocytes maintain high basal levels of autophagy independent of mtor signaling. Autophagy. 2020;16:1932–1948. doi: 10.1080/15548627.2019.1705007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nishi H, Nangaku M. Podocyte lipotoxicity in diabetic kidney disease. Kidney Int. 2019;96:809–812. doi: 10.1016/j.kint.2019.07.013. [DOI] [PubMed] [Google Scholar]
- 6.Wang X, Antony V, Wang Y, Wu G, Liang G. Pattern recognition receptor-mediated inflammation in diabetic vascular complications. Med Res Rev. 2020;40:2466–2484. doi: 10.1002/med.21711. [DOI] [PubMed] [Google Scholar]
- 7.Hsieh CF, Liu CK, Lee CT, Yu LE, Wang JY. Acute glucose fluctuation impacts microglial activity, leading to inflammatory activation or self-degradation. Sci Rep. 2019;9:840. doi: 10.1038/s41598-018-37215-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kang R, Loux T, Tang D, Schapiro NE, Vernon P, Livesey KM, Krasinskas A, Lotze MT, Zeh HJ., III The expression of the receptor for advanced glycation endproducts (RAGE) is permissive for early pancreatic neoplasia. Proc Natl Acad Sci USA. 2012;109:7031–7036. doi: 10.1073/pnas.1113865109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chtourou Y, Aouey B, Kebieche M, Fetoui H. Protective role of naringin against cisplatin induced oxidative stress, inflammatory response and apoptosis in rat striatum via suppressing ROS-mediated NF-κB and P53 signaling pathways. Chem Biol Interact. 2015;239:76–86. doi: 10.1016/j.cbi.2015.06.036. [DOI] [PubMed] [Google Scholar]
- 10.Huang Q, Zhan L, Cao H, Li J, Lyu Y, Guo X, Zhang J, Ji L, Ren T, An J, et al. Increased mitochondrial fission promotes autophagy and hepatocellular carcinoma cell survival through the ROS-modulated coordinated regulation of the NFκB and TP53 pathways. Autophagy. 2016;12:999–1014. doi: 10.1080/15548627.2016.1166318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kim KA, Shin YJ, Akram M, Kim ES, Choi KW, Suh H, Lee CH, Bae ON. High glucose condition induces autophagy in endothelial progenitor cells contributing to angiogenic impairment. Biol Pharm Bull. 2014;37:1248–1252. doi: 10.1248/bpb.b14-00172. [DOI] [PubMed] [Google Scholar]
- 12.Saha S, Panigrahi DP, Patil S, Bhutia SK. Autophagy in health and disease: A comprehensive review. Biomed Pharmacother. 2018;104:485–495. doi: 10.1016/j.biopha.2018.05.007. [DOI] [PubMed] [Google Scholar]
- 13.Lenoir O, Jasiek M, Hénique C, Guyonnet L, Hartleben B, Bork T, Chipont A, Flosseau K, Bensaada I, Schmitt A, et al. Endothelial cell and podocyte autophagy synergistically protect from diabetes-induced glomerulosclerosis. Autophagy. 2015;11:1130–1145. doi: 10.1080/15548627.2015.1049799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nishida K, Watanabe H, Ogaki S, Kodama A, Tanaka R, Imafuku T, Ishima Y, Chuang VT, Toyoda M, Kondoh M, et al. Renoprotective effect of long acting thioredoxin by modulating oxidative stress and macrophage migration inhibitory factor against rhabdomyolysis-associated acute kidney injury. Sci Rep. 2015;5:14471. doi: 10.1038/srep14471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhou Z, Sun B, Huang S, Zhu C, Bian M. Glycemic variability: Adverse clinical outcomes and how to improve it? Cardiovasc Diabetol. 2020;19:102. doi: 10.1186/s12933-020-01085-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Monnier L, Colette C, Owens DR. Glycemic variability: The third component of the dysglycemia in diabetes. Is it important? How to measure it? J Diabetes Sci Technol. 2008;2:1094–1100. doi: 10.1177/193229680800200618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ceriello A, Esposito K, Piconi L, Ihnat MA, Thorpe JE, Testa R, Boemi M, Giugliano D. Oscillating glucose is more deleterious to endothelial function and oxidative stress than mean glucose in normal and type 2 diabetic patients. Diabetes. 2008;57:1349–1354. doi: 10.2337/db08-0063. [DOI] [PubMed] [Google Scholar]
- 18.Ying C, Wang S, Lu Y, Chen L, Mao Y, Ling H, Cheng X, Zhou X. Glucose fluctuation increased mesangial cell apoptosis related to AKT signal pathway. Arch Med Sci. 2019;15:730–737. doi: 10.5114/aoms.2019.84739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ying C, Zhou X, Chang Z, Ling H, Cheng X, Li W. Blood glucose fluctuation accelerates renal injury involved to inhibit the AKT signaling pathway in diabetic rats. Endocrine. 2016;53:81–96. doi: 10.1007/s12020-016-0867-z. [DOI] [PubMed] [Google Scholar]
- 20.Wang H, Deng J, Chen L, Ding K, Wang Y. Acute glucose fluctuation induces inflammation and neurons apoptosis in hippocampal tissues of diabetic rats. J Cell Biochem jcb. 2019;29523 doi: 10.1002/jcb.29523. [DOI] [PubMed] [Google Scholar]
- 21.Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) Method. Methods. 2001;25:402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 22.Li X, Zhu Q, Zheng R, Yan J, Wei M, Fan Y, Deng Y, Zhong Y. Puerarin Attenuates Diabetic Nephropathy by Promoting Autophagy in Podocytes. Front Physiol. 2020;11:73. doi: 10.3389/fphys.2020.00073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Uchida T, Shirasawa M, Ware LB, Kojima K, Hata Y, Makita K, Mednick G, Matthay ZA, Matthay MA. Receptor for advanced glycation end-products is a marker of type I cell injury in acute lung injury. Am J Respir Crit Care Med. 2006;173:1008–1015. doi: 10.1164/rccm.200509-1477OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhang ZY, Miao LF, Qian LL, Wang N, Qi MM, Zhang YM, Dang SP, Wu Y, Wang RX. Molecular Mechanisms of Glucose Fluctuations on Diabetic Complications. Front Endocrinol (Lausanne) 2019;10:640. doi: 10.3389/fendo.2019.00640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nicholas SB, Basgen JM, Sinha S. Using stereologic techniques for podocyte counting in the mouse: Shifting the paradigm. Am J Nephrol. 2011;33(Suppl 1):1–7. doi: 10.1159/000327564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Guo J, Sang Y, Yin T, Wang B, Yang W, Li X, Li H, Kang Y. miR-1273g-3p participates in acute glucose fluctuation-induced autophagy, dysfunction, and proliferation attenuation in human umbilical vein endothelial cells. Am J Physiol Endocrinol Metab. 2016;310:E734–E743. doi: 10.1152/ajpendo.00444.2015. [DOI] [PubMed] [Google Scholar]
- 27.Amidi S, Hashemi Z, Motallebi A, Nazemi M, Farrokhpayam H, Seydi E, Pourahmad J. Identification of (Z)-2,3-Diphenylacrylonitrileas Anti-Cancer Molecule in Persian Gulf Sea Cucumber Holothuria parva. Mar Drugs. 2017;15:15. doi: 10.3390/md15100314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tang S, Hou Y, Zhang H, Tu G, Yang L, Sun Y, Lang L, Tang X, Du YE, Zhou M, et al. Oxidized ATM promotes abnormal proliferation of breast CAFs through maintaining intracellular redox homeostasis and activating the PI3K-AKT, MEK-ERK, and Wnt-β-catenin signaling pathways. Cell Cycle. 2015;14:1908–1924. doi: 10.1080/15384101.2015.1041685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ma H, Su L, Yue H, Yin X, Zhao J, Zhang S, Kung H, Xu Z, Miao J. HMBOX1 interacts with MT2A to regulate autophagy and apoptosis in vascular endothelial cells. Sci Rep. 2015;5:15121. doi: 10.1038/srep15121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Irace C, Misso G, Capuozzo A, Piccolo M, Riccardi C, Luchini A, Caraglia M, Paduano L, Montesarchio D, Santamaria R. Antiproliferative effects of ruthenium-based nucleolipidic nanoaggregates in human models of breast cancer in vitro: Insights into their mode of action. Sci Rep. 2017;7:45236. doi: 10.1038/srep45236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Liu T, Xia Y, Li J, Li S, Feng J, Wu L, Zhang R, Xu S, Cheng K, Zhou Y, et al. Shikonin Attenuates Concanavalin A-Induced Acute Liver Injury in Mice via Inhibition of the JNK Pathway. Mediators Inflamm. 2016;2016:2748367. doi: 10.1155/2016/2748367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Li P, Zheng X, Shou K, Niu Y, Jian C, Zhao Y, Yi W, Hu X, Yu A. The iron chelator Dp44mT suppresses osteosarcoma's proliferation, invasion and migration: In vitro and in vivo. Am J Transl Res. 2016;8:5370–5385. [PMC free article] [PubMed] [Google Scholar]
- 33.Zhao W, Feng H, Guo S, Han Y, Chen X. Danshenol A inhibits TNF-α-induced expression of intercellular adhesion molecule-1 (ICAM-1) mediated by NOX4 in endothelial cells. Sci Rep. 2017;7:12953. doi: 10.1038/s41598-017-13072-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Amaral LSB, Souza CS, Volpini RA, Shimizu MHM, de Bragança AC, Canale D, Seguro AC, Coimbra TM, de Magalhães ACM, Soares TJ. Previous Exercise Training Reduces Markers of Renal Oxidative Stress and Inflammation in Streptozotocin-Induced Diabetic Female Rats. J Diabetes Res. 2018;2018:6170352. doi: 10.1155/2018/6170352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schmelzer C, Lorenz G, Rimbach G, Döring F. In Vitro Effects of the Reduced Form of Coenzyme Q(10) on Secretion Levels of TNF-alpha and Chemokines in Response to LPS in the Human Monocytic Cell Line THP-1. J Clin Biochem Nutr. 2009;44:62–66. doi: 10.3164/jcbn.08-182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Guijarro C, Egido J. Transcription factor-kappa B (NF-kappa B) and renal disease. Kidney Int. 2001;59:415–424. doi: 10.1046/j.1523-1755.2001.059002415.x. [DOI] [PubMed] [Google Scholar]
- 37.Cai W, Li J, Xu JX, Liu Y, Zhang W, Xiao JR, Zhu LY, Liu JY. Association of 2184AG Polymorphism in the RAGE Gene with Diabetic Nephropathy in Chinese Patients with Type 2 Diabetes. J Diabetes Res. 2015;2015:310237. doi: 10.1155/2015/310237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mukherjee TK, Mukhopadhyay S, Hoidal JR. The role of reactive oxygen species in TNFalpha-dependent expression of the receptor for advanced glycation end products in human umbilical vein endothelial cells. Biochim Biophys Acta. 2005;1744:213–223. doi: 10.1016/j.bbamcr.2005.03.007. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.