Abstract
Summary: Vascular malformations arising from the wall of the external jugular vein are rare. This case series discusses the sonographic and MR imaging appearances of four such cases and reviews the literature. The diagnosis should be suggested preoperatively particularly because of the close relationship such malformations to the external jugular vein, as this helps surgeons to plan the operative procedure. The imaging appearances are similar to those of other vascular malformations elsewhere in the head and neck.
Mulliken and Glowacki, in 1982, proposed a classification of vascular lesions based on endothelial characteristics (1) that gained wide acceptance. In this scheme, vascular lesions were separated into two major groups: infantile hemangiomas and vascular malformations. Hemangiomas are characterized by endothelial cellular hyperplasia and proliferation, characteristically grow rapidly for 6–8 months after birth, and then regress to a variable extent. On the other hand, vascular malformations have a normal endothelial cell cycle and do not involute.
Intrinsic vascular lesions arising from the wall of the external jugular vein are very rare. This case series discusses the sonographic and MR imaging appearances of four cases of vascular malformations of external jugular venous wall, highlighting the imaging appearances that help to make the preoperative diagnosis. The differential diagnosis and clinical appearances are discussed and the literature reviewed.
Case Reports
Case 1
A 31-year-old Indonesian woman presented with a left neck mass that progressively increased in size for 3 years. No fever or other constitutional symptoms existed. On physical examination, there was a 2-cm soft, nontender mass in the left posterior triangle. It was mobile and not attached to overlying skin or underlying muscle. No pulsation or thrill was demonstrated. There was no other palpable mass or lymph node detected in the rest of the neck. The suggested clinical diagnosis was lipoma or enlarged cervical lymph node.
Sonography showed an elliptical, solid, hypoechoic 21-mm noncalcified mass inseparable from the left external jugular vein. On gray-scale sonography, the mass demonstrated hypoechoic vascular spaces with slow flow within them. Power Doppler sonography demonstrated color flow within the mass (Fig 1A).
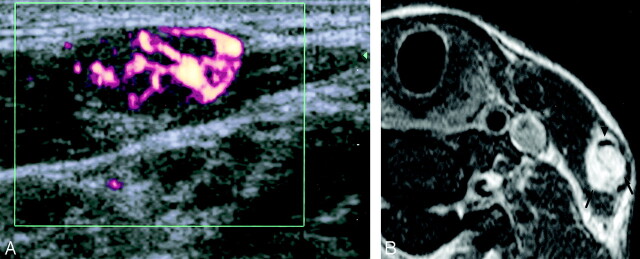
Fig 1.
Case 1. Sonographic and MR images obtained in a 31-year-old Indonesian woman with a vascular malformation of the left external jugular vein.
A, Transverse power Doppler sonography shows vascularity within a well-defined, hypoechoic, heterogeneous mass.
B, Axial T1-weighed fat-suppressed contrast-enhanced MR imaging image (TR/TE, 450/15) shows intense enhancement of the mass (arrows) and its relationship to the left external jugular vein (arrowhead).
MR imaging demonstrated a well-defined 25-mm ovoid mass arising from the left external jugular vein. This mass showed intermediate signal intensity on T1-weighted images and very high signal intensity on T2-weighed images, with serpinginous regions of flow void suggestive of vessels. After intravenous administration of gadolinium, the mass was homogeneously hyperintense (Fig 1B). The left external jugular vein showed normal signal intensity void, and its patency was further confirmed by postgadolinium MR venography.
A preoperative imaging diagnosis of a vascular malformation inseparable from the left external jugular venous wall was made. Intraoperatively, a vascular lump arising from the external jugular vein was identified. The proximal and distal ends of feeding vessels were ligated, and the mass was completely excised.
Histologic analysis showed a lobular vascular malformation composed of central feeding vessels with peripherally situated lobular aggregates of capillary sized vessels. No evidence of malignancy was detected.
Case 2
A 21-year-old Chinese woman presented with a left neck mass that had been present for 6 weeks. The size of the mass fluctuated, and there was intermittent tenderness on palpation. On physical examination, there was a soft, nontender 1.5-cm nodule in the left lower posterior triangle. The overlying skin was normal, with no erythema or thickening. The mass flattened upon pressure and filled up again upon release. No other palpable mass or lymph node was detected in the rest of the neck. The suggested clinical diagnosis was vascular malformation.
Sonography showed a 25-mm mass in the left posterior triangle with heterogeneous internal echoes, septae, calcifications, and slow-flowing vascular spaces that was inseparable from the posterior wall of the left external jugular vein (Fig 2A and B). On the basis of the sonographic appearances, a diagnosis of venous vascular malformation inseparable from the left external jugular vein was made.
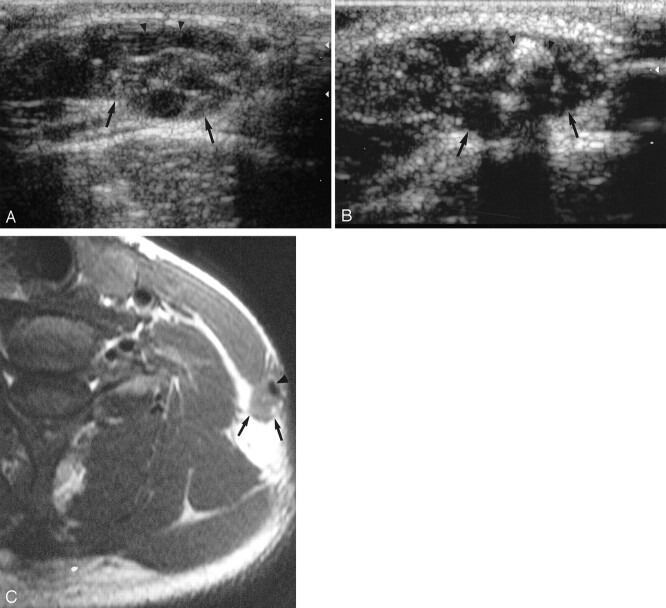
Fig 2.
Case 2. Sonographic and MR images obtained in a 21-year-old woman with a left external jugular vein vascular malformation.
A, Transverse gray-scale sonography shows a hypoechoic heterogeneous mass (arrows) closely related to the external jugular vein (arrowheads).
B, Longitudinal gray-scale sonography shows a phlebolith (arrowheads) within the mass (arrows).
C, Axial T1-weighed spin-echo MR imaging image (TR/TE, 425/12) shows an isointense mass (arrows) closely related to the left external jugular vein (arrowhead). It is closely abutting the posterior edge of the left sternocleidomastoid muscle (asterisk).
MR imaging demonstrated a well-defined, 25-mm soft-tissue mass inseparable from the left external jugular vein. This mass showed intermediate signal intensity on T1-weighed images, heterogeneous high signal intensity on T2-weighed images, and mild enhancement after intravenous administration of gadolinium (Fig 2C). The left external jugular vein showed normal signal intensity void and was patent.
Intraoperatively, a vascular lesion arising from the external jugular vein was found. The proximal and distal venous channels were clearly identified and ligated. The lesion was peeled off the sternocleidomastoid and posterior triangle quite easily.
Macroscopically, the excised lesion was a well-circumscribed dark brown nodule (Fig 3A). The cut surface revealed brownish tissue with soft consistency and focal calcifications. Microscopically, the nodule was composed of ectatic vascular spaces with a thin wall and lined by a layer of endothelium (Fig 3B). Smooth muscle was found in the wall of some vessels. An organized thrombus and calcification were noted focally within the vascular lumens. The pathologic diagnosis was consistent with venous vascular malformation.
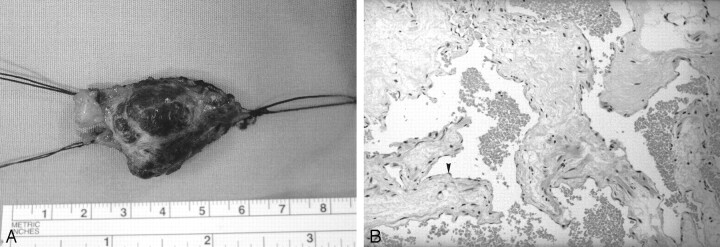
Fig 3.
Case 2. Pathologic and histologic sections of a specimen obtained by excision of the left external jugular vein vascular malformation.
A, Gross specimen of the excised lesion shows a well-circumscribed mass with the proximal and distal vascular stumps of the external jugular vein.
B, High-power histologic view of the vascular channels. Note the lining flattened endothelial cells (arrowhead) and the red cells inside the lumens. (Hematoxylin-eosin stain, original magnification, ×120.)
Case 3
A 37-year-old man presented with right upper neck mass of 8-year duration. During this period, the mass fluctuated in size. He was otherwise well, with no constitutional symptoms. On examination, there was soft, nontender 3-cm mass in the right upper neck close to the sternocleidomastoid muscle. It was completely compressible. Neither overlying skin change nor other neck mass was detected. The clinical diagnosis was vascular malformation.
Sonography showed a 3-cm hypoechoic mass in the right neck superficial to the sternocleidomastoid muscle. There were vascular spaces and slow flow on gray-scale imaging (Fig 4A). It was closely related to and inseparable from the wall of the adjacent right external jugular vein. No calcified phlebolith was detected within this lesion. On the basis of the sonographic appearance, vascular malformation inseparable from the external jugular vein was suspected.
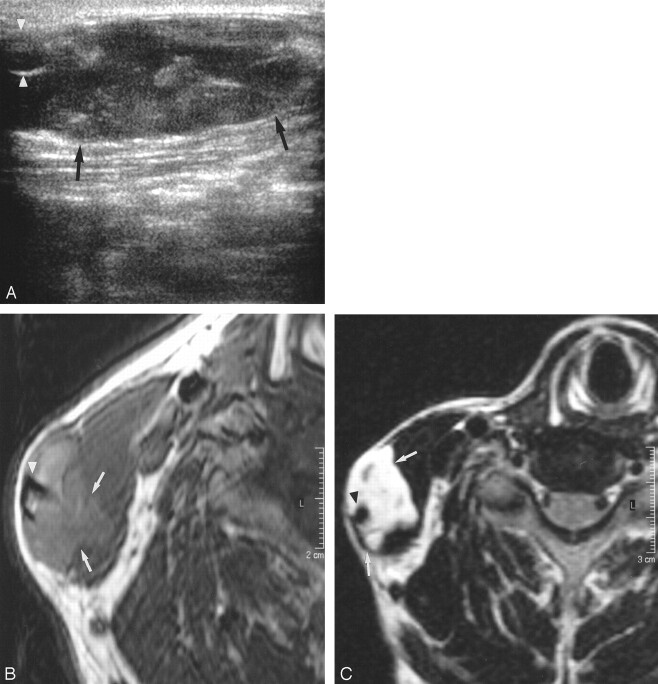
Fig 4.
Case 3. Sonographic and MR images obtained in a 37-year-old man with right external jugular vein vascular malformation.
A, Transverse gray-scale sonography shows an ill-defined, hypoechoic, heterogeneous mass (arrows) inseparable from the external jugular vein (arrowheads).
B, Axial T1-weighed spin-echo MR imaging image (TR/TE, 425/18) shows a slightly hyperintense mass (arrows) with ill-defined edges closely related to the right external jugular vein (arrowhead).
C, Axial fat-suppressed T2-weighed MR imaging image (TR/TE, 2500/108) shows a hyperintense mass (arrows) closely related to and inseparable from the right external jugular vein (arrowhead). Note its infiltration into the adjacent sternocleidomastoid muscle.
MR imaging demonstrated a well-defined, slightly lobulated 3-cm lesion in the right neck superficial to and infiltrating the right sternocleidomastoid muscle. On its posterolateral aspect, this lesion was inseparable from the right external jugular vein. The lesion showed intermediate signal intensity on T1-weighted images, very high signal intensity on T2-weighted images, and enhanced avidly after intravenous gadolinium injection (Fig 4B and C). The right external jugular vein showed normal signal intensity void and was patent. The preoperative imaging diagnosis was vascular malformation likely arising from the right external jugular vein.
A vascular lesion arising from the external jugular vein infiltrating the sternocleidomastoid muscle was found at surgery. The right great auricular nerve penetrated the lesion. The mass was dissected off the sternocleidomastoid muscle, and the right auricular nerve was sacrificed.
Microscopic examination of the excised specimen showed irregular aggregates of muscular vessels without elastic layer (not shown). The vessels had variable thickness in various portions of vessel wall. Some dilated vascular spaces lined by endothelium were present, with focally organized thrombus within the lumen. Histologic features were compatible with vascular malformation.
Case 4
A 61-year-old man presented with left neck mass of 6-month duration. Clinical examination suggested a dilated left neck vessel. There was no associated pain or ulceration. He had no other local or systemic sign or symptom.
Sonography showed a 25-mm mass with internal slow turbulent flow arising from the left external jugular vein. It had heterogeneous internal echoes, vascular spaces with slow flow at gray-scale sonography. Doppler sonography confirmed vascularity within the mass.
MR imaging demonstrated a lobulated mass surrounding the lower portion of the left external jugular vein. The mass showed intermediate T1 signal intensity, high T2 signal intensity, and moderate enhancement after intravenous administration of gadolinium. The left external jugular vein was patent with normal signal intensity void.
An imaging diagnosis of a vascular malformation inseparable from the left external jugular venous wall was made. This patient refused surgical treatment, as he considered the symptom trivial and the lesion cosmetically acceptable. He has now been followed up for 2 years, and follow-up sonography has shown the left external jugular venous wall lesion to be static in size with no evidence of infiltration.
Discussion
The nomenclature of cutaneous vascular lesions in the past had always been perplexing, with no consensus until 1982, when Mulliken and Glowacki (1) proposed their revolutionary classification scheme. This scheme, based on endothelial cellular characteristics, correlates well with the biologic behavior of such cutaneous vascular lesions. Vascular lesions can be divided into two major types with distinct clinical characteristics.
The first type is designated as hemangiomas. These lesions are present at birth 40% of the time, usually appearing as a small red mark, with a female predilection of 5:1. They typically show rapid neonatal growth characterized by endothelial cellular hyperplasia and proliferation in the proliferative phase, followed by slow regression to a variable extent characterized by diminished cellularity and fibrofatty deposition in the involuting phase.
The second type is designated as vascular malformations. These lesions are recognized at birth 90% of the time with no sex predilection. They grow commensurately with the child and do not regress. Histologically they are characterized by “mature” endothelium that are not hypercellular and show a normal endothelial cell cycle. They may have any combination of capillary, venous, arterial, and lymphatic components, with or without fistulas, although most of these lesions are predominantly venous in type. This cell-oriented analysis has since gained wide acceptance because of its diagnostic applicability, which helps in planning therapy.
Intrinsic vascular malformations arising from the wall of the external jugular vein are very rare. To the best of our knowledge, only two such cases have been described in the English-language literature (2, 3). In both these cases, the diagnosis of external jugular vein “hemangioma” was made after surgery. Under the classification scheme of Mulliken and Glowacki, these two cases seem more appropriate to be designated as external jugular vein vascular malformations. We describe a further four cases of external jugular vein vascular malformation in which the diagnosis was suggested preoperatively by imaging features and confirmed by surgery in three patients.
In 1999, Sarteschi et al (3) first reported a case of right external jugular vein “hemangioma” occurring as a lateral neck mass in which color-coded duplex sonography contributed significantly to the diagnosis. The venous wall “hemangioma” appeared as a well-defined, solid, hypoechoic nodule with endoluminal involvement. There was no sign of infiltration of surrounding structures. Gray-scale imaging features were similar to those of intravascular thrombus adherent to the venous wall, but on compression, the venous lumen was collapsible, whereas the lesion was firm. Pulsed Doppler, color Doppler, and power Doppler revealed the proliferative nature of the lesion by demonstrating a close net of microvessels inside, thereby clarifying the nature of the lesion as a neoplasm rather than a thrombus.
Gold et al (4), in an analysis of six cases of maxillofacial vascular or suspected vascular anomalies in 2003, also reported that only sonography or Doppler capability can differentiate venous and arterial malformations and flow characteristics. They found, however, that a single imaging technique is frequently unable to provide sufficient diagnostic information to allow confident clinical management and thus propose the use of nonenhanced MR imaging with sonography or color Doppler to provide the best diagnostic information.
The sonographic and MR imaging appearances of head and neck hemangiomas or vascular malformations are well documented (5, 6).
In all the cases in the present study, the external jugular venous wall vascular malformations showed similar sonographic features. The venous wall vascular malformations appeared as well-defined, ovoid, heterogeneous hypoechoic nodules with internal flow signals arising from the venous wall with endoluminal extension but no adjacent soft tissue infiltration. We were able to identify phleboliths within the lesion in one case, which enabled us to make a confident diagnosis of venous vascular malformation (7). In all patients in this series, the presenting symptoms, clinical examination findings, location, and imaging appearances were identical (except for phleboliths in one of the cases).
The sonographic and MR imaging appearances of external jugular vein vascular malformations in this series were typical of those demonstrated by other vascular malformations in the head and neck region; ie, well-defined, hypoechoic masses with heterogeneous echotexture, cystic or sinusoidal spaces, and possible phleboliths (5). Head and neck vascular malformations typically show intermediate signal intensity (slightly higher than that of muscles) on T1-weighed images, very high signal intensity on T2-weighed images, and variable enhancement after intravenous gadolinium administration (6, 7). Signal intensity void due to high flow and phleboliths may also be demonstrated at MR imaging in the form of serpiginous and nodular configuration, respectively. To our knowledge, no previous report of MR imaging features of external jugular venous wall vascular malformations exists in the literature. This series is the first one to show that these jugular venous wall vascular malformations demonstrate similar sonographic and MR imaging features to those arising in other soft tissues and muscles in the head and neck region. The distinguishing feature to suggest the diagnosis is their close relationship to the external jugular vein. Accurate preoperative diagnosis of external jugular vein vascular malformations is important to plan surgical treatment. The external jugular vein and its major tributaries have to be identified and ligated during surgery to prevent excessive bleeding.
The differential diagnosis includes other primary tumors of vessels (ie, low-grade malignant hemangioendothelioma and hemangiopericytoma, and the frankly malignant hemangiosarcoma and leiomyosarcoma). These tumors are all very rare but may enter the differential list if the lesion shows evidence of enlargement or local infiltration clinically or on imaging studies.
Conclusion
The sonographic and MR imaging appearances of vascular malformation of the external jugular vein are similar to other vascular malformations of the head and neck. The key imaging feature for correct preoperative diagnosis is its close relationship to adjacent external jugular vein. Because its location and relationship to the external jugular vein affect surgical management, radiologists should be aware of this rare disease entity.
References
- 1.Mulliken JB, Glowacki J Hemangiomas and vascular malformations in infants and children: a classification based on endothelial characteristics. Plast Reconstr Surg 1982;69:412–422 [DOI] [PubMed] [Google Scholar]
- 2.Meyers MA. Hemangioma of the external jugular vein. Radiology 1967;89:483–485 [DOI] [PubMed] [Google Scholar]
- 3.Sarteschi LM, Bonanomi G, Mosca F, Ferrari M. External jugular vein hemangioma occuring as a lateral neck mass. J Ultrasound Med 1999;18:719–721 [DOI] [PubMed] [Google Scholar]
- 4.Gold L, Nazarian LN, Johar AS, Rao VM. Characterization of maxillofacial soft tissue vascular anomalies by ultrasound and color Doppler imaging: an adjuvant to computed tomography and magnetic resonance imaging. J Oral Maxillofac Surg 2003;61:19–31 [DOI] [PubMed] [Google Scholar]
- 5.Yang WT, Ahuja AT, Metreweli C. Sonographic features of head and neck hemangiomas and vascular malformations: review of 23 patients. J Ultrasound Med 1997;16:39–44 [DOI] [PubMed] [Google Scholar]
- 6.Baker LL, Dillon WP, Hieshima GB, et al. Hemangiomas and vascular malformations of the head and neck: MR characterization. AJNR Am J Neuroradiol 1993;14:307–314 [PMC free article] [PubMed] [Google Scholar]
- 7.Fordham LA, Chung CJ, Donnelly LF. Imaging of congenital vascular and lymphatic anomalies of the head and neck. Neuroimaging Clin N Am 2000;10:117–136 [Review]. [PubMed] [Google Scholar]