Abstract
Summary: Radiologic findings of a case with scalp plexiform schwannoma—an unusual variant of the benign, solitary schwannoma in the skin—are reported. T2-weighted MR imaging exhibited the most specific features: a multinodular pattern and hypointense capsule that separated the tumor from surrounding soft tissue. A surgical specimen was histologically confirmed as schwannoma. The MR imaging findings reported herein may aid in the preoperative diagnosis of this relatively rare scalp tumor.
Plexiform schwannoma (PS) (1–3) is an unusual variant of the benign, solitary schwannoma that can be located either in the deep soft tissues or in the cutis (4, 5). The primary location is the trunk, followed by the head, neck, and extremities (4). PS is a tumor of adulthood with a slight male predominance (7:5) (4) that can mimic plexiform neurofibroma both clinically and histologically; however, to our knowledge no increased association with von Recklinghausen disease or a higher risk for malignant transformation has been reported (1–5). The tumor grows slowly in a plexifrom or multinodular pattern (3, 6) and usually manifests as a soft movable nodule with an average size of 3 cm (4).
Previous studies have focused on histopathologic and immunohistochemical characteristics of this unusual tumor; however, to our knowledge no radiologic data to aid in the preoperative diagnosis are currently available. We now report CT and MR imaging findings in a patient with a solitary PS of the scalp.
Case Report
A 31-year-old generally healthy male patient presented at Kumamoto Neurosurgical Hospital on September 25, 2002 with a left retroauricular scalp tumor. Since he first noticed a small subcutaneous mass about 5 years earlier, it had grown gradually to more than 5 cm in diameter (Fig 1). The skin over the tumor was mildly discolored with partial alopecia (Fig 1). The mass was elastic, hard, and movable. The patient reported no spontaneous pain. Physical examination did not reveal café-au-lait spots, Lisch nodules, or axillaries freckling suggestive of neurofibromatosis. A CT scan revealed an isoattenuated, round to oval mass under the skin (Fig 2A). There was erosion of the left occipital and mastoid bones because of the tumor (Fig 2B, arrow). T1- and T2-weighted MR imaging demonstrated a subcutaneous mass that was well demarcated from surrounding soft tissue by a hypointense capsule (Fig 3). T2-weighted MR images (Fig 3B and D) showed that the tumor was composed of many small, hyperintense nodules separated by relatively hypointense internodular structures. CT and MR imaging revealed no intracranial abnormalities. The patient underwent tumor removal under local infiltrative anesthesia on September 27, 2002. An elastic hard mass covered by a smooth capsule was located immediately under a thin layer of skin. The parent nerve was not evident. The tumor was easily dissected from the surrounding adipose tissue and was removed en bloc (Fig 4A). No complications ensued, and the patient was discharged on the day of surgery.
Fig 1.
Photograph showing a large scalp tumor in the left retroauricular portion. The surface of the skin presents mild discoloration and partial alopecia.
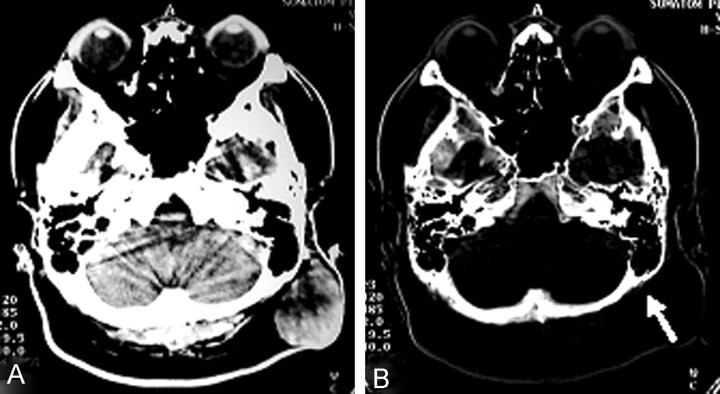
Fig 2.
CT scan depicting a left subcutaneous mass exhibiting low isoattenuation (A) and bone image CT (B) showing erosion of the occipitomastoid bones (arrow); no evidence of tumor invasion into the skull is evident.
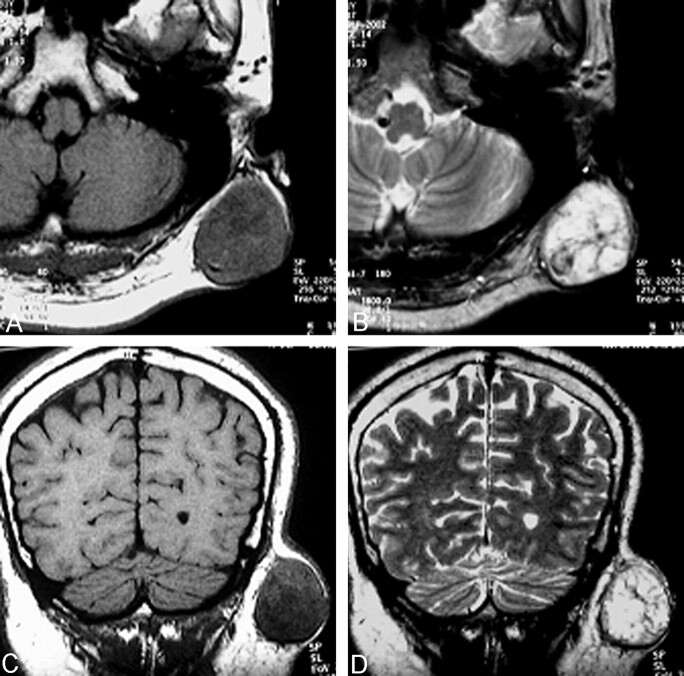
Fig 3.
Axial (A and B) and coronal (C and D) MR images. The mass (4 × 5 cm in diameter) is seated within the subcutaneous adipose tissue. The tumor is heterogeneously hypoisointense and surrounded by a hypointense thin capsule on T1-weighted images (A and C). The multiple, hyperintense nodules are separated by a hypointense, internodular structure on T2-weighted images (B and D).
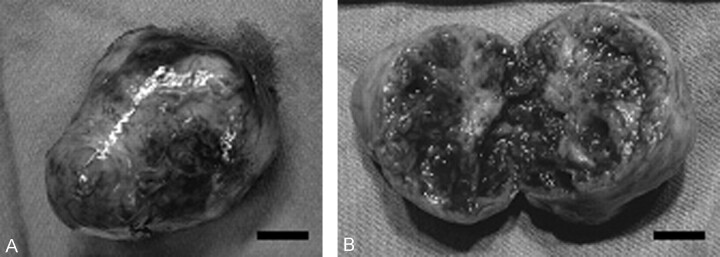
Fig 4.
Gross specimen of the removed tumor. The tumor is covered by smooth fibrous capsule (A) and composed of well-circumscribed, soft to rubbery-firm nodules (B). The cut surface of the tumor is grayish white to yellow and there are scattered macroscopic hemorrhages (B). Scale bars: 1 cm in both A and B.
Macroscopic Findings
The cut surface of the solid tumor was grayish white to yellow, and scattered hemorrhagic foci were present. Multiple small nodules were packed and covered with a thin, fibrous capsule (Fig 4).
Microscopic Findings
Histopathologic study revealed fascicles and multiple, interconnecting nodules arranged in a plexiform pattern. The tumor was encased by a thin, fibrous capsule and separated from surrounding dermis. Constituent cells were spindled with irregular, generally elongated nuclei and wavy, ill-defined, eosinophilic cytoplasm. Nuclear palisading and Verocay bodies were evident. The fascicles and nodules were hypercellular and exhibited the Antoni-A features of a solitary schwannoma (Fig 5A). There were foci of Antoni-B areas with hypocellularity and myxoid or fibrous stroma with degenerative changes. The specimens showed increased vascularity and scattered hemorrhages. Nuclear pleomorphism existed, but mitotic figures were absent. Sections stained by Klüver-Barrela revealed no myelinated fibers. Hyalinization, suggestive of chronic degeneration, was evident in the center of the specimen. There was no extensive tumoral necrosis, and no invasive pattern was observed.
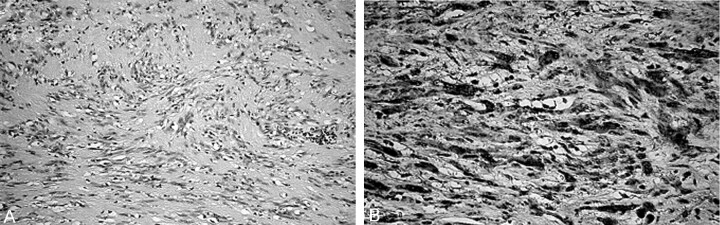
Fig 5.
Photomicrographs of the tumor. A, The constituent cells are spindle-shaped with irregular, generally elongated nuclei and wavy, ill-defined, eosinophilic cytoplasm. (Hematoxylin-eosin, original magnification ×100) B, The tumor cells exhibit strong immunoreactivity for S-100 protein. (Original magnification ×200)
Immunohistochemical Studies
Antibodies to bovine S-100 protein (1:400; Dako; Glostrup, Denmark), neurofilament (1:100; Dako), α-SMA (1:400; Sigma, St. Louis, MO), and muscle actin (1:50; Dako) were used. Tumor cells were strongly immunoreactive for S-100 protein (Fig 5B). Neurofilament-positive fibrous indicating residual axons, however, were not prominent in the specimens examined. The cells were not stained by α-SMA or muscle actin.
Discussion
As currently understood, PS is a morphologic variant of schwannoma that involves superficially situated dermal or subcutaneous nerves or both (6). Although the parent nerve is not always evident macroscopically, Burger et al (6) have reported that residual axons can be confirmed by immunohistochemical staining for neurofilament protein. In the patient reported herein, however, residual axons were not evident. Although most cases of PS are sporadic, some occur in the setting of schwannomatosis (6–9), and a small proportion recur after incomplete excision (5, 6, 10).
To our knowledge, the present study is the first to depict the radiologic findings of a case of solitary PS. Signal intensity characteristics (ie, heterogeneous hypo- or isointensity on T1-weighted images and hyperintensity on T2-weighted images) seemed to be almost identical to those found in patients with intracranial schwannoma. Previous studies reporting MR imaging findings of peripheral nerve sheath tumors also described the relatively consistent pattern: iso- or hypointense lesions relative to skeletal muscle on T1-weighted images and iso- or hyperintense lesions relative to subcutaneous fat on T2-weighted images (11–13). In the present study, however, we note a hyperintense multinodular pattern of PS on T2-weighted MR images, which may aid in the radiologic diagnosis of this relatively rare scalp tumor. On both T1- and T2-weighted MR images, we observed a smooth tumor capsule visualized as a hypointense thin wall.
The histopathologic differential diagnosis includes plexiform neurofibroma, plexiform fibrohistiocytic tumor (PFHT), and, in rare cases, malignant peripheral nerve sheath tumors. Plexiform neurofibroma may exhibit features that superficially resemble PS, although it usually does not show distinct nuclear palisading or Verocay bodies (14) and cells are cytologically more uniform and arranged in a fine fibrillary pattern. PFHT is similar to plexiform neurofibroma and can mimic PS clinically and histopathologically (15). This tumor has a high local recurrence rate (37%) and a tendency for regional metastasis (6.2%) (4). Immunohistochemically, PFHT cells do not stain for S-100 protein but are variably positive for markers suggesting myofibroblastic differentiation rather than Schwann cells (16). These findings are very different from those made in the case of our patient: the tumor cells were strongly immunoreactive for S-100 and absolutely negative for α-SMA and muscle actin.
Conclusion
We present the radiologic findings in a patient with a PS of the scalp that exhibited a hyperintense multinodular pattern on T2-weighted MR images. Findings documented herein may aid in the preoperative radiologic diagnosis of this relatively rare scalp tumor.
References
- 1.Fletcher CDM, Davies SE. Benign plexifrom (multinodular) schwannoma: a rare tumour unassociated with neurofibromatosis. Histopathol 1986;10:971–980 [DOI] [PubMed] [Google Scholar]
- 2.Harkin JC, Arrington JH, Reed RJ. Benign plexifrom schwannoma: a lesion distinct from plexifrom neurofibroma. J Neuropathol Exp Neurol 1978;37:622 [Google Scholar]
- 3.Woodruff JM, Marshall ML, Godwin TA, et a;. Plexiform (multinodular) schwannoma: A tumor simulating the plexifrom neurofibraoma. Am J Surg Pathol 1983;7:691–697 [DOI] [PubMed] [Google Scholar]
- 4.Argenyi ZB. Recent developments in cutaneous neural neoplasms. J Cutan Pathol 1993;20:97–108 [DOI] [PubMed] [Google Scholar]
- 5.Kao GF, Laskin WB, Olsen TG. Solitary cutanous plexifrom neurilemmoma (schwannoma): a clinicopathologic, immunohistochemical, and ultrastructural study of 11 cases. Mod Pathol 1989;2:22–26 [PubMed] [Google Scholar]
- 6.Burger PC, Scheithauer BW, Vogel FS. The peripheral nervous system. In: Burger PC, Scheithauer BW, Vogel FS, eds. Surgical Pathology of the Nervous System and Its Coverings. 4th ed. Philadelphia: Churchill Livingstone;2002;579–648
- 7.MacCollin M, Woodfin W, Kronn D, Short MP. Schwannomatosis: a clinical and pathologic study. Neurology 1996;46:1072–1079 [DOI] [PubMed] [Google Scholar]
- 8.Reith JD, Goldblum JR. Multiple cutaneous plexifrom schwannomas: report of a case and review of the literature with particular reference to the association with types 1 and 2 neurofibromatosis and schwannomatosis. Arch Pathol Lab Med 1996;120:399–401 [PubMed] [Google Scholar]
- 9.Val-Bernal JF, Figols J, Vazquez-Barquero A. Cutaneous plexiform schwannoma associated with neurofibromatosis type 2. Cancer 1995;76:1181–1186 [DOI] [PubMed] [Google Scholar]
- 10.Iwashita T, Enjoji M. Plexiform neurilemoma: a clinicopathological and immnohistochemical analysis of 23 tumours from 20 patients. Virchows Arch A 1987;411:305–309 [DOI] [PubMed] [Google Scholar]
- 11.Ahmed AR, Watanabe H, Aoki J, et al. Schwannoma of the extremities: the role of PET in preoperative planning. Eur J Nucl Med 2001;28:1541–1551 [DOI] [PubMed] [Google Scholar]
- 12.Kobayashi H, Kotoura Y, Sakahara H, et al. Schwannoma of the extremities: comparison of MRI and pentavalent technetium-99m-dimercaptosuccinic acid and gallium-67-citrate scintigraphy. J Nucl Med 1994;35:1174–1178 [PubMed] [Google Scholar]
- 13.Soderlund V, Goranson H, Bauer HC. MR imaging of benign peripheral nerve sheath tumors. Acta Radiol 1994;35:282–286 [PubMed] [Google Scholar]
- 14.Jurecka W. Plexiforme neurofibroma of the skin. Am J Dermatopathol 1988;10:209–217 [DOI] [PubMed] [Google Scholar]
- 15.Enzinger FM, Zhang R. Plexiform fibrohistiocytic tumor presenting in children and young adults. Am J Surg Pathol 1988;12:818–826 [DOI] [PubMed] [Google Scholar]
- 16.Hollowood K, Holley MP, Fletcher CDM. Plexiform fibrohistiocytic tumour: clinicopathological, immunohistochemical and ultrastructural analysis in favour of a myofibroblastic lesion. Histopathol 1991;19:503–513 [DOI] [PubMed] [Google Scholar]