Abstract
BACKGROUND AND PURPOSE: Percutaneous ethanol sclerotherapy has been reported to be efficacious for head and neck venous malformations. We sought to evaluate the safety and efficacy of percutaneous sclerotherapy by using ethanol for treatment of symptomatic venous malformations of the tongue.
METHODS: Eleven sclerotherapy procedures were performed in seven patients from January 1995 to February 2001. Patient age ranged from 19 months to 57 years (mean age, 32 years). Four patients were male and three were female. Mean follow-up was 36 months. The volume of ethanol used per treatment session ranged from 2 to 32 cc (mean, 16 cc).
RESULTS: Sclerotherapy provided significant improvement or resolution of symptoms for all patients. There were no major complications. One patient had a small (3 × 2 cm) area of skin blistering at the injection site. All patients experienced pain and swelling to a variable degree. Sclerotherapy resulted in resolution of symptoms in six of seven patients. Three patients had resolution of symptoms after one procedure. Four patients each underwent two sclerotherapy procedures. One patient who remained symptomatic but improved after undergoing two procedures underwent an anterior glossectomy and is now asymptomatic.
CONCLUSION: Percutaneous ethanol sclerotherapy is a safe and effective method of treating symptomatic venous malformations of the tongue.
Venous malformations of the tongue are low flow vascular malformations that can cause significant clinical problems and are challenging to treat. These malformations are congenital, although they are not always evident at birth. They grow proportionately with age and do not regress. At the histologic level, these malformations are composed of thin walled channels, deficient in smooth muscle and lined by a single layer of flat endothelium (1). By contrast, hemangiomas are usually not present at birth, grow rapidly during infancy, and typically involute during childhood. Treatment of symptomatic hemangiomas is aimed at controlling symptoms until the lesion involutes, whereas treatment of symptomatic venous malformations is directed at eliminating or reducing the lesion. Venous malformations have a propensity for the head and neck region, and lesions of the tongue are not rare (Fig 1). Symptoms are related to the size and location of the venous malformation. Lesions of the tongue may bleed, ulcerate, cause pain, interfere with speech and swallowing, and obstruct the airway. Percutaneous ethanol sclerotherapy of venous malformations has been reported to be efficacious for venous malformations of the head and neck region (2–6). We report our experience treating venous malformations of the tongue by percutaneous injection using ethanol.
Fig 1.

Image of a 42-year-old man with extensive venous malformation of the tongue.
Methods
From January 1995 to February 2001, 11 percutaneous ethanol sclerotherapy procedures were performed in seven patients with symptomatic venous malformations of the tongue. A retrospective analysis and radiographic review were performed at the University of Kansas Medical Center. Each patient was evaluated and followed by a member of the Department of Otolaryngology, Head and Neck Surgery (D.A.G., T.T.T.). The diagnosis was established on clinical grounds, and MR imaging was performed for all patients to define the initial extent of the lesion. Ethanol sclerotherapy was performed in the interventional radiology suite under the direction of a neurointerventional radiologist (P.L.J., D.A.E.). Four patients with venous malformations involving the tongue base underwent tracheotomy before the procedure to protect the airway, because these lesions can swell dramatically after treatment. Tracheotomy was not performed in patients with anterior tongue lesions that were not thought to be a threat to the airway. Eight procedures were performed with the patient under general anesthesia and endotracheal intubation. The remaining procedures were performed with the patient under conscious sedation using midazolam (Versed; Roche Laboratories, Nutley, NJ) and fentanyl (Abbott Laboratories, North Chicago, IL).
Arteriography was not performed in any patient. During the procedure, the patient’s tongue was grasped using dry gauze and retracted to allow for better visualization of the venous malformation and to facilitate placement of the needles. If a portion of the venous malformation was too posterior to reach via an oral approach, the lesion was percutaneously punctured through the floor of the mouth. Percutaneous injection of contrat material was performed on all lesions to define the volume, morphology, and draining veins of each lesion (Fig 2). Multiple ethanol injections were administered to all patients. The venous malformations were injected using 23-gauge butterfly needles attached to a three-way stopcock. At the time of the free return of blood, contrast material was injected and digital subtraction angiography (one frame/s) was performed. When draining veins were identified, they were manually compressed if possible. The volume of contrast material used to fill the venous malformation was determined, and the same volume of ethanol was injected under direct fluoroscopic visualization. The volume of ethanol used per treatment session ranged from 2 to 32 cc (mean, 17 cc). Ethanol injections were performed until thrombosis of the venous malformation occurred. Thrombosis was determined by development of a hard consistency to the venous malformation and a lack of free return of blood during needle puncture. The predetermined maximum dose of ethanol injected per session was 1 mL/kg. Care was taken not to over inject the venous malformation with alcohol and to avoid extravasation into the adjacent soft tissues. All patients received antibiotics and steroids, although the regimens varied according to patient age and physician preference. The most common antibiotic regimen was 1.5 g of IV administered Unasyn (ampicillin sodium/sulfbactam sodium; Pfizer, New York, NY) every 6 hours during hospitalization and 500 mg of Augmentin (amoxicillin/clavulanate; GlaxoSmithKline, Research Triangle Park, NC) every 8 hours after discharge for a total of 5 to 7 days. Most patients received a single IV administered dose of 100 mg of hydrocortisone succinate (Merck, West Point, PA) or 8 mg of decadron phospate (Merck). One patient who had a large posterior tongue venous malformation and significant post-procedural swelling received 4 mg of IV administered decadron every 6 hours for 24 hours after the procedure. The steroids were then gradually tapered off during the next 5 days. All patients received IV administered fluids during the procedure and for at least 4 hours after the procedure, and all patients were admitted at least overnight for observation. Follow-up examinations were performed at 2 months, 6 months, and annually (sooner if any problems developed). Follow-up MR images were obtained of those patients who had lesions that were difficult to assess by direct visualization.
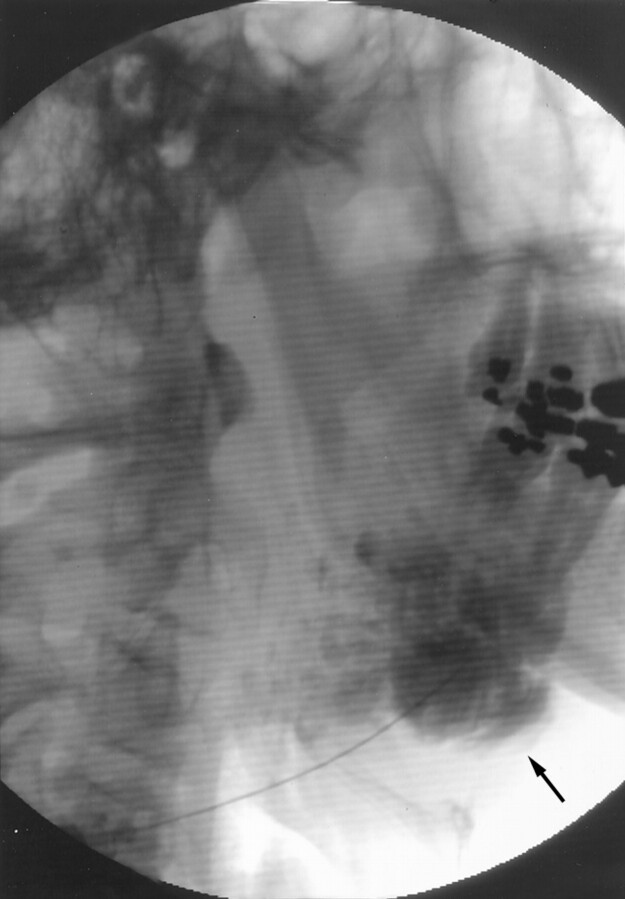
Fig 2.
Direct puncture venogram, obtained through the floor of the mouth, shows opacification of a multilobular mass (arrow) deep within the tongue, with an appearance typical of that of venous malformation.
Results
Patient age ranged from 19 months to 57 years (mean age, 32 years). Four patients were male and three were female. Most patients had multiple presenting symptoms. The most common symptom was breathing difficulty (including sleep apnea), with the next most common being swelling and difficulty with speech (Table). Four patients underwent ethanol sclerotherapy alone. One patient had undergone multiple previous operations before undergoing sclerotherapy. One patient underwent sclerotherapy and then surgery. Two patients received intralesional steroid injections, and one of the two had also undergone surgery several years before undergoing percutaneous sclerotherapy.
Presenting symptoms of patients with venous malformations of the tongue
| Symptom | Number of Patients |
|---|---|
| Difficulty breathing | 4 |
| Swelling | 3 |
| Difficulty with speech | 3 |
| Pain | 2 |
| Bleeding | 2 |
| Dizziness | 1 |
Percutaneous ethanol sclerotherapy resulted in improvement or resolution of symptoms in all patients. The mean follow-up duration was 36 months (range, 1–68 months). Sclerotherapy resulted in resolution of symptoms in six of the seven patients. Each of three patients experienced resolution of symptoms after undergoing a single procedure. Four patients each underwent two sclerotherapy procedures. The average time between procedures was 11 months (range, 2–22 months). One patient who experienced resolution of symptoms and a 50% decrease in lesion size after the initial procedure underwent a second sclerotherapy procedure while an existing tracheotomy was in place. Each of three patients who underwent two procedures experienced improvement in symptoms after the initial procedure but had some persistent symptoms (ie, recurrent swelling, problems with speech, or minor bleeding). Two of these three patients experienced resolution of the symptoms after the second procedure. The third patient, who continued to experience intermittent minor bleeding, underwent anterior glossectomy and became asymptomatic. There were no major complications with percutaneous sclerotherapy and few immediate post-procedural side effects. One patient experienced swelling that interfered with swallowing and required a nasogastric tube for 2 days. Another patient whose lesion caused breathing difficulties before the procedure experienced significant swelling after sclerotherapy, requiring intubation for 5 days (the patient was initially intubated for general anesthesia for the procedure). One patient developed a 3 × 2 cm area of blistering and ulceration over the venous malformation that resolved after 10 days.
Discussion
Venous malformations are common vascular malformations that can occur in any location, although they have a propensity to occur in the head and neck region, including the tongue. They can be localized or diffuse. Histologically, venous malformations are composed of thin walled channels, deficient in smooth muscle and lined by a single layer of endothelium (1).
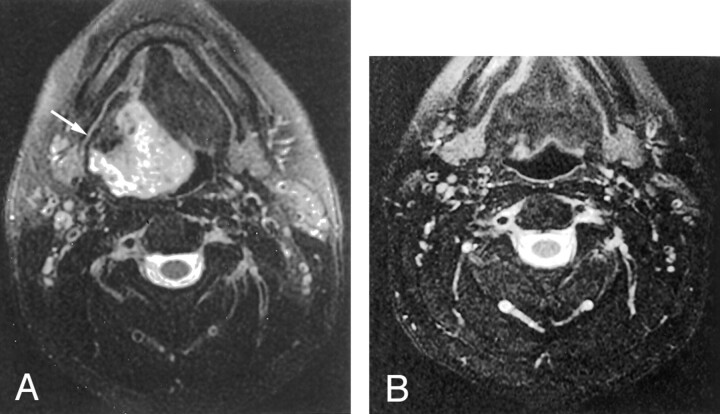
These lesions are low flow vascular malformations, and because they are by definition malformations of the venous system, they usually are not seen on arteriograms, even during the late venous phase. Occasionally, a faint blush may be seen during the late venous phase. Arteriography has little if any role in the workup and treatment of these lesions. MR imaging and direct injection venography provide the most useful information. MR imaging is also useful for following lesions in the tongue base, which are more difficult to assess by direct visualization. Venous malformations show high signal intensity on MR images (Fig 3).
Fig 3.
MR images show high signal intensity for venous malformations.
A, Axial T2-weighted MR image shows a heterogenous hyperintense mass within the right base of the tongue (arrow).
B, Follow-up axial T2-weighted MR image, obtained 6 months after percutaneous ethanol sclerotherapy, reveals near complete resolution of the tongue base venous malformation.
Venous malformations are present at birth, although they may not be evident until later in life. Most venous malformations show progressive enlargement, perhaps due to hormonal influences or trauma (1). These malformations do not regress the way hemangiomas of infancy typically do. Venous malformations are generally soft with a bluish discoloration when visible. They may show enlargement with the Valsalva maneuver or dependent positioning. Symptoms are related to size and location. Lesions of the tongue cause ulceration, bleeding, pain, speech and swallowing difficulty, and airway obstruction.
The goal of therapy for symptomatic venous malformations of the tongue is to eliminate the malformation and conserve as much lingual tissue as possible. Complete surgical excision of these lesions is rarely possible without causing significant functional impairment and disfigurement.
Ethanol sclerotherapy causes denudation of endothelium, intense inflammatory reaction, and thrombosis of the venous malformation almost immediately (2). During the next several weeks, fibrosis develops (2). Complications from ethanol are usually due to alcohol extravasation within the adjacent soft tissues, resulting in necrosis. Blistering and ulceration can develop and usually resolve with conservative therapy. Nerve damage and tissue sloughing can occur, and cardiopulmonary collapse necessitating resuscitation has also been reported (7).
Conclusion
Ethanol sclerotherapy of venous malformations has been reported by several authors to be efficacious for head and neck region venous malformations (2–6). We conclude that this therapy is efficacious for venous malformations of the tongue and is associated with a low complication rate.
References
- 1.Mulliken JB, Young AE. Vascular Birthmarks: Hemangiomas and Malformations. Philadelphia: Saunders;1988
- 2.Yakes WF, Luethke JM, Parker SH, et al. Ethanol embolization of vascular malformations. Radiographics 1990;10:787–796 [DOI] [PubMed] [Google Scholar]
- 3.Yakes WF, Haas DK, Parker SH, et al. Symptomatic vascular malformations: ethanol embolotherapy. Radiology 1989;170:1059–1066 [DOI] [PubMed] [Google Scholar]
- 4.Berenguer B, Burrows PE, Zurakowski, Mulliken JB. Sclerotherapy of craniofacial venous malformations: complications and results. Plast Reconstr Surg 1999;104:1–11 [PubMed] [Google Scholar]
- 5.Gelbert F, Enjolras O, Deffrenne, Aymard A, Mounayer C, Merland JJ. Percutaneous sclerotherapy for venous malformations of the lips: a retrospective study of 23 patients. Neuradiology 2000;42:692–696 [DOI] [PubMed] [Google Scholar]
- 6.Pappas DC, Persky MS. Evaluation and treatment of head and neck venous vascular malformations. ENT J 1988;77:914–922 [PubMed] [Google Scholar]
- 7.Yakes WF, Baker R. Cardiopulmonary collapse: sequelae of ethanol embolotherapy. Radiology 1993;189:145 [Google Scholar]