Abstract
Summary: Identification of recurrent cholesteatoma and differentiation from postoperative granulation tissue is important in a patient who has undergone mastoidectomy for cholesteatoma. We describe the diffusion-weighted imaging findings and apparent diffusion coefficient values in a case of recurrent cholesteatoma. This case suggests possible differentiation of cholesteatoma from granulation tissue on the basis of diffusion-weighted imaging findings.
An important role of imaging of patients who have undergone mastoidectomy for cholesteatoma is attempting to differentiate recurrent cholesteatoma from postoperative granulation tissue. Patients with recurrent cholesteatoma require revision mastoidectomy with resection of the recurrent disease (1). However, patients with granulation tissue are usually treated with supportive measures and may not require a follow-up procedure.
The imaging findings of recurrent cholesteatoma have been described (2). The CT findings of recurrent cholesteatoma include a progressively enlarging focal mass associated with bone erosion or ossicular displacement. The MR imaging findings of recurrent cholesteatoma include a hyperintense mass on T2-weighted images that has intermediate-to-low T1-weighted signal intensity and that enhances minimally after the administration of contrast material (3). The MR imaging findings of postoperative granulation tissue include diffuse enhancement within the surgical bed (4). Despite these accepted appearances, the ability of cross-sectional imaging to distinguish between recurrent cholesteatoma and granulation tissue is not reliable (5). Patients with well-aerated postoperative mastoid bowls and middle ear cavities can be easily evaluated with CT (6). However, patients with diffuse mucosal thickening of the middle ear cavity associated with bone or ossicular irregularities that may or may not be associated with previous surgery are difficult to evaluate with CT or MR imaging. As a result, many surgeons have to perform a follow-up procedure to determine the cause of the mucosal thickening.
Diffusion-weighted imaging is a technique that measures the molecular diffusion of water (Brownian motion) within the tissues being measured (7). We report the case of a patient who had undergone multiple procedures for recurrent cholesteatoma in which diffusion-weighted imaging detected recurrent cholesteatoma.
Case Report
A 52-year-old woman initially underwent trans-labyrinthine mastoidectomy for resection of left middle ear cholesteatoma in 1974. The patient had a residual left VIIth nerve palsy after the procedure. She was re-examined in 1994 because of recurrent otorrhea and infections. Recurrent cholesteatoma was revealed, and completion mastoidectomy with external ear canal obliteration was performed. Six years after this procedure, the patient returned with a 3-month history of progressive headaches and loss of balance. The headaches were primarily vertex but radiated to the left temporal region.
A physical examination revealed that the previous surgical incision and canal overclosure were well healed. The patient continued to have complete left facial palsy (House-Brackman grade IV).
CT of the left ear revealed the postoperative mastoid bowl filled with soft tissue (Fig 1). MR imaging showed a focal soft tissue mass just deep to the site of the overclosure that had homogeneously high signal intensity on T2-weighted images (Fig 2). Contrast-enchanced T1-weighted imaging showed an intermediate-signal-intensity mass with a thin rim of enhancement, which was strongly suspicious for recurrent cholesteatoma (Fig 3). Diffusion-weighted imaging was performed using a single-shot, spin-echo T2-weighted echo-planar sequence. This showed increased signal within the mass (Fig 4). Apparent diffusion coefficient showed the low signal intensity, with values of 0.58 × 10−3 mm2/s.
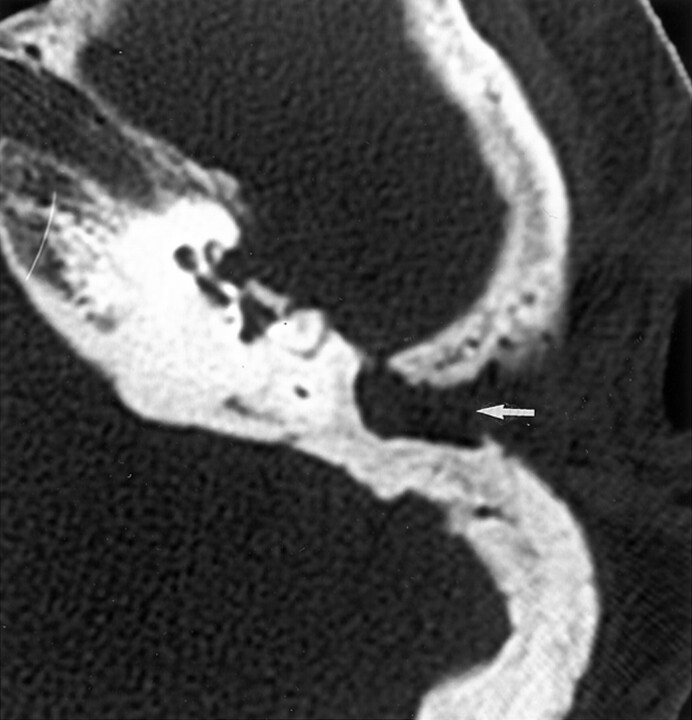
Fig 1.
Axial view CT scan shows soft tissue (arrow) filling the postoperative mastoidectomy bowl and extending medially to the middle ear cavity.
Fig 2.
Axial view T2-weighted MR image shows the soft tissue to be of high T2 signal (M).
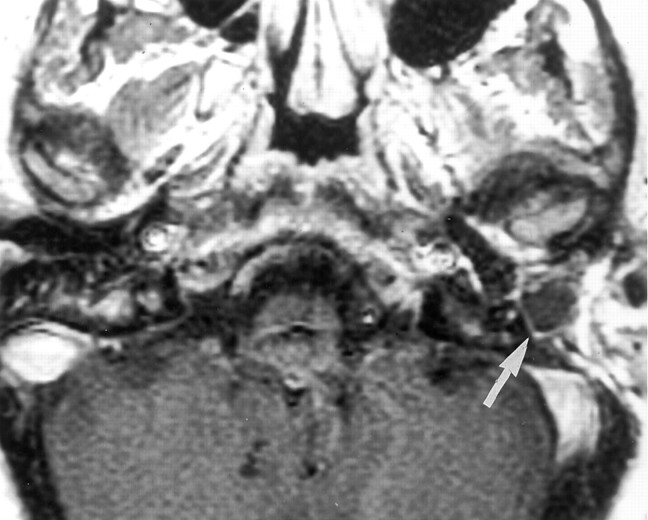
Fig 3.
Axial view contrast-enhanced T1-weighted MR image shows the mass to be of intermediate signal with a thin rim of peripheral enhancement (arrow). T1- and T2-weighted findings are strongly indicative of cholesteatoma.
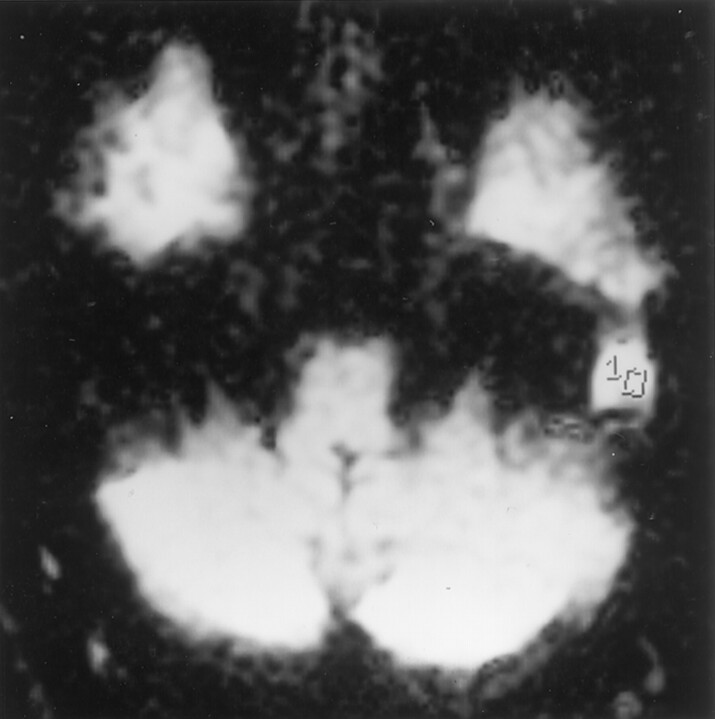
Fig 4.
Diffusion-weighted image shows increased signal intensity in the middle ear cavity mass (1). Outline indicates where the apparent diffusion coefficient values were obtained.
On the basis of the history of recurrent cholesteatoma, physical examination results, and cross-sectional imaging findings, the patient was diagnosed by her otologist as having recurrent cholesteatoma. The patient has been closely followed to monitor the growth and extension of the cholesteatoma.
Discussion
Acquired cholesteatoma consists of epithelial debris that results from desquamation of the lining of the external auditory canal and outer lining of the tympanic membrane. The treatment is surgical resection. However, complete surgical extirpation may be difficult in advanced lesions. After surgery, it is difficult to distinguish between recurrent cholesteatoma and granulation tissue from both clinical and radiologic standpoints. The middle ear cavity is difficult to visualize because of postoperative scarring and thickening of the tympanic membrane. The imaging appearance on both MR images and CT scans is often nonspecific. As a result, many patients with chronic otorrhea must undergo revision mastoidectomies and middle ear exploration to determine whether the nonspecific imaging abnormalities are due to recurrent cholesteatoma or granulation tissue. Correct identification of recurrent cholesteatoma would identify those patients who require surgical resection, whereas patients with granulation tissues would be treated more conservatively with supportive measures.
Diffusion-weighted MR imaging provides information regarding the molecular diffusion of water (Brownian motion) in the examined tissue (7). Diffusion-weighted imaging has been accepted as an accurate method for detecting acute stoke (8) and is also being evaluated in a variety of other intracranial disease processes (9). The role of diffusion-weighted imaging for evaluating head and neck disorders is currently being evaluated. Wang et al (10) recently calculated the diffusion and apparent diffusion coefficient values of a variety of head and neck lesions. They found apparent diffusion coefficient values to be increased in cystic lesions. In solid lesions, the values were higher for benign lesions as compared with malignant lesions. The role of diffusion imaging in the evaluation of recurrent cholesteatoma has not been evaluated. Our case suggested that increased diffusion-weighted imaging signal intensity within a middle ear mass that has undergone surgery for cholesteatoma is suggestive of recurrent cholesteatoma.
Histopathologically, acquired cholesteatoma is an enlarging collection of exfoliated keratin within a sac of stratified squamous epithelium (4). In the past, cholesteatoma has been confused with epidermoids. Epidermoids are congenital neoplasms that tend to occur in basal cisterns, especially cerebellopontine angles (11). On diffusion-weighted images, epidermoids are hyperintense whereas arachnoid cysts are hypointense. Schaefer et al (9) measured the apparent diffusion coefficient values of these lesions and found the values to be similar to those of gray matter but lower than those of CSF. They postulated that a combination of T2 shine-through and restricted diffusion was responsible for the hyperintensity of these lesions on diffusion images. Chen et al (12) reported a series of eight patients with epidermoids and measured apparent diffusion coefficient values. They concluded that the hyperintensity of epidermoids on diffusion-weighted images is not caused by restricted diffusion but only by T2 shine-through effects. The exact cause of the increased diffusion-weighted imaging signal intensity in association with cholesteatoma is unknown but is likely analogous to the cause of the increased diffusion-weighted imaging signal intensity in association with epidermoid tumors.
In our case, cholesteatoma was bright on diffusion-weighted images. The apparent diffusion coefficient values in the cholesteatoma were 0.58 × 10−3 mm2/s. The apparent diffusion coefficient values of CSF in the basal cisterns were approximately 2 × 10−3 and approximately 0.78 × 10−3 in the adjoining gray matter. On the basis of apparent diffusion coefficient mapping, we concur with previous reports and think that the hyperintensity of cholesteatoma on diffusion images is likely a combination of T2 shine-through and restriction.
This report suggests that diffusion-weighted imaging may be helpful in identifying recurrent cholesteatoma. However, the ability of diffusion-weighted imaging to be consistently used to evaluate the temporal bone is hindered by image distortion caused by susceptibility artifacts, chemical shift artifacts, and ghosts in the phase encoding direction. This is due to the high bone density of the inner ear and the numerous air-bone interfaces present within the mastoid air cells and the middle ear cavity. Further studies are necessary to determine the full usefulness of diffusion imaging and to determine whether diffusion imaging should become a routine part of postoperative imaging in an attempt to distinguish between postoperative granulation tissue and recurrent cholesteatoma.
References
- 1.Sheehy JL, Robinson JV. Revision tympanoplasty: residual and recurrent cholesteatoma: a report on 272 intact canal wall revisions. In: Sade J, ed. Cholesteatoma and Mastoid Surgery: IInd International Conference. Amsterdam: Kugler;1982. :443–448
- 2.Veillon F. Imaging of recurrent postoperative cholesteatoma: syllabus of the International Congress of Head and Neck Radiology. Strasbourg,1997
- 3.Martin N, Sterkers O, Nahum H. Chronic inflammatory disease of the middle ear cavities: Gd-DTPA-enhanced MR imaging. Radiology 1990;176:399–405 [DOI] [PubMed] [Google Scholar]
- 4.Joel D, Swartz H, Haensberger R. Imaging of temporal bone. Stuttgart: Thieme Medical Publishers;1997. :78 [Google Scholar]
- 5.Vanden Abeele D, Coen E, Parizel PM, Van de Heyning P. Can MRI replace a second look operation in cholesteatoma surgery? Acta Otolaryngol 1999;119:555–561 [DOI] [PubMed] [Google Scholar]
- 6.Czerny C, Turetschek K, Duman M, Imhof H. Imaging of the middle ear: CT and MRI [in German]. Radiologe 1997;37:945–953 [DOI] [PubMed] [Google Scholar]
- 7.Le Bihan D, Breton E, Lallemand D, Grenier P, Cabanis E, Laval-Jeantet M. MR imaging of intravoxel incoherent motions: application to diffusion and perfusion in neurologic disorders. Radiology 1986;161:401–407 [DOI] [PubMed] [Google Scholar]
- 8.Chien D, Kwong KK, Gress DR, Buon-anno FS, Buxton RB, Rosen BR. MR diffusion imaging of cerebral infarction in humans. AJNR Am J Neuroradiol 1992;13:1097–1105 [PMC free article] [PubMed] [Google Scholar]
- 9.Schaefer PW, Grant PE, Gonzalez RG. Diffusion-weighted MR imaging of the brain. Radiology 2000;217:331–345 [DOI] [PubMed] [Google Scholar]
- 10.Wang J, Takashima S, Takayama F, et al. Head and neck lesions: characterization with diffusion-weighted echo-planar MR imaging. Radiology 2001;220:621–630 [DOI] [PubMed] [Google Scholar]
- 11.Ikushima I, Korogi Y, Hirai T, et al. MR of epidermoids with a variety of pulse sequences. AJNR Am J Neuroradiol 1997;18:1359–1363 [PMC free article] [PubMed] [Google Scholar]
- 12.Chen S, Ikawa F, Kurisu K, Arita K, Takaba J, Kanou Y. Quantitative MR evaluation of intracranial epidermoid tumors by fast fluid-attenuated inversion recovery imaging and echo-planar diffusion-weighted imaging. AJNR Am J Neuroradiol 2001;22:1089–1096 [PMC free article] [PubMed] [Google Scholar]