Abstract
Summary: Three patients with internal carotid artery thrombus and thrombolysis in myocardial infarction (TIMI) 0–1 flow were treated by using intraarterial (IA) suction thrombectomy a mean of 4.2 hours after stroke onset. After catheterization with a 7F guide-catheter, thrombus was aspirated by using a 60-mL syringe. TIMI flow improved to 3 in all patients. The median National Institutes of Health Stroke Scale score decreased from 22 (range, 12–23) to 4 (range, 2–22) at 3 months. IA suction thrombectomy may be safe and feasible in patients with acute stroke.
Because the use of chemical thrombolytics may be contraindicated in certain patients with acute stroke, other treatment options are needed. This report discusses a readily available intraarterial (IA) technique that involves the use of suction applied with a syringe to remove thrombus in the internal carotid artery (ICA).
Case Reports
Three patients had substantial neurologic deficits due to acute anterior circulation ischemia, and CT scans showed involvement of no more than one third of the MCA territory. Symptoms were present for at least 3 hours. In each patient, ICA thrombus was angiographically visualized, with 0 or 1 thrombolysis in myocardial infarction (TIMI) flow. In all three patients, the use of intravenous or IA thrombolytics was believed to be contraindicated.
The symptomatic vessel was catheterized with a 7F catheter (Brite-tip; Cordis, Miami, FL) that was navigated over a guidewire into the proximal third of the thrombus. A 60-mL syringe was used to aspirate the thrombus. Aspiration was performed by moving the catheter in and out of the thrombus several times; aspiration was continued for approximately 10 seconds each time. The guide-catheter was slowly withdrawn to allow more complete removal of the thrombus. Aspiration was stopped when the catheter was pulled out of the occluded artery. The patient in case 2 received a 2000-U heparin bolus when the thrombus was identified, and then 500 U/h for 4 hours. Patients in cases 1 and 3 were already receiving heparin and warfarin, respectively. All patients received daily aspirin after the procedure. Those in whom stents were placed (patients in cases 1 and 2) additionally received daily ticlopidine for 1 month.
Angiographic findings were recorded before and after the procedure. The National Institutes of Health Stroke Scale (NIHSS) was evaluated at baseline, and both the NIHSS and the Modified Rankin score were assessed at 3 months. The Table provides a summary of the clinical results.
Clinical results with suction thrombectomy
| Case No./ Patient Age (y) | Hours to Treatment | Vessel | NIHSS Score |
Modified Rankin Score at 3 Months | |
|---|---|---|---|---|---|
| Preoperative | At 3 Months | ||||
| 1/57 | 3* | Right ICA | 12 | 2 | 1 |
| 2/72 | 5 | Left ICA | 23 | 22 | 3 |
| 3/49 | 4.5 | Right ICA | 22 | 4 | 3† |
Since worsening.
Patient had a concurrent foot infection that limited his walking.
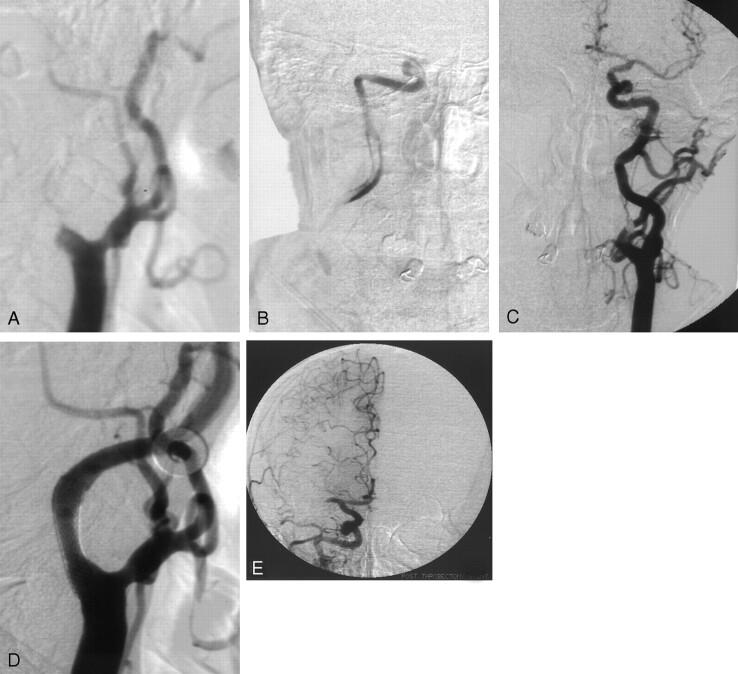
Case 1
A 67-year-old man presented with resolving left hemiparesis, which then recurred with cortical neglect 14 hours later. The recent stroke and the hypoattenuation in the right basal ganglia on CT scans discouraged the use of IA thrombolytics. Angiography showed near-occlusion (TIMI 1) of the right ICA (Fig 1A). A tight stenosis at the ICA origin was predilated with an angioplastic balloon to allow passage of the guide-catheter and to permit a more useful injection of contrast agent. Thrombus was identified in the artery after angioplasty (Fig 1B). Although some cross-filling of the right anterior cerebral artery (ACA) was seen with the left CCA injection, no filling of the right middle cerebral artery (MCA) was present (Fig 1C). With the catheter in the distal occluded right ICA, suction thrombectomy yielded 5 mL of thrombus 3 hours from symptom deterioration (17 hours from symptom onset). A 6 × 2-mm Wallstent was placed at the site of the ICA stenosis. Follow-up angiograms (Fig 1D) showed filling of the right ICA (TIMI 3) and ACA, and a mid-M1 occlusion of the right MCA. However, the distal MCA branches now filled well via pial collaterals from the ACA (Fig 1E). The patient had only a residual left facial droop and mild drift at 3 months.
Fig 1.
Case 1. A 67-year-old man presented with resolving left hemiparesis.
A, Baseline right lateral common carotid artery (CCA) angiogram shows near-occlusion of the right ICA with a string sign of slow flow into the proximal ICA.
B, After predilation of the proximal ICA stenosis, this baseline right ICA angiogram reveals the presence of extensive thrombus.
C, Baseline left CCA angiogram reveals some right ACA cross-filling but no right MCA filling.
D, Postprocedural right lateral CCA angiogram shows less than 20% residual ICA stenosis. A Wallstent in the ICA is visible at the carotid bifurcation.
E, Although the right MCA has a persistent mid-M1 occlusion, the postprocedural right CCA angiogram shows good distal filling of the MCA branches via pial collaterals from the ACA.
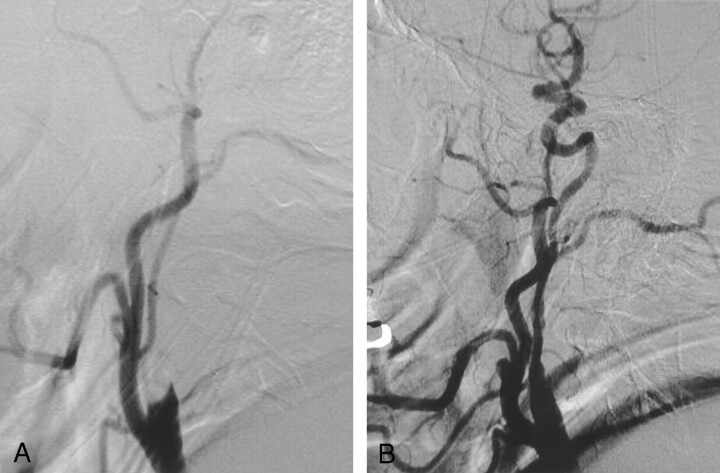
Case 2
A 72-year-old man had global aphasia and right hemiparesis. Angiography demonstrated complete occlusion (TIMI 0) of the cervical left ICA (Fig 2A). Injection of the right CCA showed no notable filling across the anterior communicating artery. Because of the severity of the clinical stroke and the extent of thrombus, compassionate use of IA thrombolytics was not recommended. Several 2–4-mm fragments of organized thrombus were aspirated from the left ICA by using suction thrombectomy approximately 5 hours after symptom onset. A residual stenosis at the carotid bifurcation was treated with angioplasty and with the placement of a 5 × 20-mm Wallstent (Fig 2B). The left ACA and MCA were patent except for small occlusions in the distal-posterior left MCA branch. Despite the reestablished ICA flow (TIMI 3), a CT scan obtained 2 days after the event showed a nonhemorrhagic infarct in the mid and posterior distributions of the left MCA. The patient’s recovery was limited over the next 3 months.
Fig 2.
Case 2. A 72-year-old man had global aphasia and right hemiparesis.
A, Baseline left lateral CCA angiogram shows complete occlusion of the cervical ICA. Flow through a 50% stenosis of the external carotid artery remains visible.
B, Postprocedural left lateral CCA angiogram demonstrates essentially complete resolution of the ICA occlusion. The Wallstent placed in the left ICA is visible at the carotid bifurcation.
Case 3
A 49-year-old man with atrial fibrillation and a poor cardiac ejection fraction presented with left hemiparesis and right gaze preference. Since the patient had had a small left temporoparietal infarct 2 weeks earlier, the use of thrombolytics was contraindicated. The first right CCA injection demonstrated complete occlusion (TIMI 0) of the cervical right ICA near its origin (Fig 3A). Suction was used to remove a small piece of thrombus approximately 4.5 hours after symptom onset; this promptly led to recanalization (TIMI 3) of the cervical ICA (Fig 3B), with good filling of the MCA, ACA and their branches. The cervical portion of the ICA had persistent stenosis of about 60% over a long segment. Two days later, MR images showed asymptomatic hemorrhagic transformation of the presenting right frontal infarction and older left temporoparietal infarct. The patient had only mild residual left hemiparesis and neglect at 3 months.
Fig 3.
Case 3. A 49-year-old man with atrial fibrillation and a poor cardiac ejection fraction presented with left hemiparesis and right gaze preference
A, Baseline right lateral CCA angiogram shows complete occlusion of the right ICA.
B, Postprocedural right lateral CCA angiogram shows restored flow within the right ICA. A long segment of vessel narrowing is seen within the cervical ICA.
Discussion
Compared with chemical thrombolytics, mechanical methods of thrombus disruption appear to shorten the time to thrombus dissolution, and they could have fewer hemorrhagic effects. Therefore, compared with drugs such as tissue plasminogen activator (tPA), mechanical methods have potential benefits in the treatment of acute stroke (1, 2). The current report illustrates the feasibility of suction thrombectomy in three patients with ICA occlusion for whom thrombolytics were believed to pose a high risk of intracranial hemorrhage. All three had excellent angiographic results, and two patients had a good clinical recovery.
ICA thrombosis has generally portended a poor prognosis, and the lesion has been resistant to treatment (3). The present series presents a more optimistic picture. Many factors may have influenced clinical outcome, despite the angiographic success in all three cases. These factors include the presence of collateral flow to the occluded vessel, the time to treatment, and the baseline neurologic status.
Two of the three cases had proximal ICA stenoses. When the stenosis was severe enough to prohibit passage of the guide-catheter, as it was in case 1, the lesion was predilated prior to thrombus aspiration. After thrombus removal, a larger-diameter balloon was used for angioplasty prior to stent placement, as was done in case 2.
Activity in the field of mechanical thrombolysis in the treatment of stroke is growing. The Endovascular Photo Acoustic Recanalization (EPAR) laser system (EndoVasix, Belmont, CA) has shown adequate safety in a preliminary study of 26 patients (4). Other technologies in early clinical trials include a device called the AngioJet that removes thrombi with suction created through the release of saline jets (Possis Medical, Minneapolis, MN), a system using ultrasound and a thrombolytic agent for thrombus disruption (EKOS, Bothell, WA), and another laser system (LaTIS, Coon Rapids, MN). Microsnares and other methods are being investigated for their ability to remove thrombi from cerebral arteries (5, 6).
One of the potential advantages of mechanical thrombolysis is the rapidity with which the vessel is opened. In the current study, the thrombus was removed within seconds of suction application, and flow was reestablished. The time required for a thrombolytic drug to lyse a clot in the clinical setting is not definitively known. In the Proact II trial (7), 63% of cases had partial or complete flow (TIMI 2 or 3) after 1 hour of prourokinase infusion into the thrombus.
Another potential benefit of mechanical thrombolysis compared with chemical thrombolysis (ICH) is a theoretically lower risk of symptomatic ICH due to the absence of a lytic state. In this small study, no patient had a symptomatic intracerebral hemorrhage. In the thrombolytic stroke treatment trials completed to date (1, 7, 8), the rates of symptomatic ICH have been 5.2–10.2%.
A potential disadvantage of mechanical thrombolysis is the production of embolic debris (2). Although two cases in the current study had evidence of MCA emboli, one was demonstrated prior to suction thrombectomy, and the status of the other prior to the procedure was unknown because of lack of cross-filling in the symptomatic side. Aside from the risks of thrombolytic use, these two cases were unlikely to have benefited from additional thrombolytic treatment. One had robust collateral flow to the occluded vessel and an excellent clinical recovery. The other patient’s persistent clinical deficits likely reflected the lack of collateral blood supply prior to thrombectomy and not flow in the small branch occlusions alone. Future cases may possibly require the use of IA thrombolytic agents to chase distal emboli that are not within reach of the mechanical devices. By decreasing the thrombus burden with suction thrombectomy, the total doses required should be lower than if thrombolytics were used alone.
In this study, suction thrombectomy was used to treat ICA thrombi. This technique is unlikely to work in thrombi in more distal vessels, because the larger-diameter catheters that have been more successful in clot extraction cannot be passed above the petrous segment of the carotid. In some cases, the thrombus composition could affect removal by means of suction. Although the thrombus was submitted for pathologic diagnosis in each of the cases in this series, no discerning features were described.
Suction thrombectomy is a simple, currently available means of mechanical thrombolysis. It should be considered on a compassionate-use basis within the first 6 hours of most recent neurologic deterioration due to carotid artery occlusion in patients in whom thrombolytic drugs are contraindicated and if marked ischemic changes affecting more than one third of the MCA territory are not present. Suction thrombectomy offers another treatment option for an often devastating disease.
Footnotes
Presented in part at the 24th International Joint Conference on Stroke and Cerebral Circulation, Nashville, TN, 1999.
References
- 1.The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. Tissue plasminogen activator for acute ischemic stroke. N Engl J Med 1995;333:1581–1587 [DOI] [PubMed] [Google Scholar]
- 2.Greenberg RK, Ouriel K, Srivastava S, et al. Mechanical versus chemical thrombolysis: an in vitro differentiation of thrombolytic mechanism. J Vasc Interv Radiol 2000;11:199–205 [DOI] [PubMed] [Google Scholar]
- 3.Mori E, Yoneda Y, Tabuchi M, et al. Intravenous recombinant tissue plasminogen activator in acute carotid artery territory stroke. Neurology 1992;42:976–982 [DOI] [PubMed] [Google Scholar]
- 4.Lutsep HL, Campbell M, Clark WM, et al. EPAR therapy system for treatment of acute stroke: safety study results. Stroke 2001;32:319b [Google Scholar]
- 5.Wikholm G. Mechanical intracranial embolectomy: a report of two cases. Intervent Neuroradiol 1998;4:159–164 [DOI] [PubMed] [Google Scholar]
- 6.Kuether TA, Nesbit GM, Barnwell SL. Other endovascular treatment strategies for acute ischemic stroke. Neuroimaging Clin N Am 1999;9:509–525 [PubMed] [Google Scholar]
- 7.Furlan A, Higashida R, Wechsler L, et al. Intra-arterial prourokinase for acute ischemic stroke: the PROACT II study—a randomized controlled trial. JAMA 1999;282:2003–2011 [DOI] [PubMed] [Google Scholar]
- 8.Sherman DG, Atkinson RP, Chippendale T, et al. Intravenous ancrod for treatment of acute ischemic stroke: The STAT study: a randomized controlled trial. JAMA 2000;283:2395–2403 [DOI] [PubMed] [Google Scholar]