Abstract
Summary: A case of recurrent brain stem edema after surgical vascular decompression in a patient with neurogenic hypertension is presented. The surgical treatment resulted in occlusion of the left vertebral artery, stable blood pressure values, and no recurrence of the brain stem edema. MR imaging and MR angiography are excellent methods with which to assess patients suspected of having neurovascular hypertension, both before and after surgical treatment.
Despite an increasing number of antihypertensive drugs, there are still certain patients who do not respond to any type of pharmaceutical therapy. Some of these patients might have so-called neurogenic hypertension caused by pulsatile vascular compression of the lower brain stem, specifically of the left lateral medulla oblongata (1). Because this disease can be treated by neurovascular decompression, establishing criteria for successful surgical intervention is critical (2).
Case Report
A 33-year-old woman had a 14-year history of hypertension, with severe aggravation within the past 3 years. Multiple antihypertensive strategies failed to control her blood pressure. Even with continuous infusion of urapidil and nitrates, her blood pressure rose to 250/150 mm Hg. Routine CT revealed an extremely elongated left vertebral and basilar artery with marked compression of the left ventrolateral medulla oblongata. These findings were confirmed by initial MR imaging in March 1999. Three-dimensional time-of-flight MR angiography confirmed extreme vessel elongation; T2-weighted and fluid-attenuated inversion recovery MR images additionally revealed a hyperintense signal of the medulla oblongata, indicating an intraaxial edema (Fig 1). On the basis of these findings and the still untreatable hypertension, neurovascular decompression was performed.
fig 1.
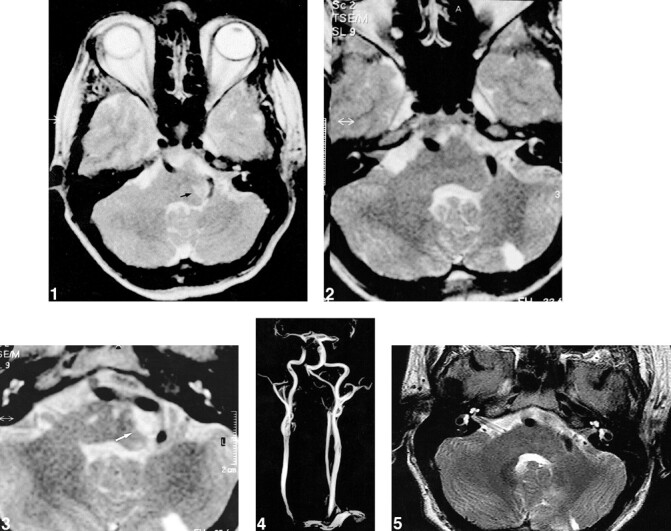
T2-weighted transversal MR image reveals extreme elongation of the vertebrobasilar junction and a hyperintense signal of the left lateral medulla oblongata (arrow), both of which indicate an intraaxial edema.fig 2. T2-weighted MR image after first microvascular decompression reveals no hyperintense signal of the left medulla oblongata, indicating disappearance of the edema. Owing to the neurovascular decompression, a small ischemic infarction of the left cerebellum developed.fig 3. T2-weighted MR image during recurrence of elevated blood pressure again reveals an edema of the brain stem at a similar location (arrowheads).fig 4. Fourteen days after second surgical intervention, MR angiography reveals complete occlusion of the left vertebral artery.fig 5. T2-weighted MR image after second microvascular decompression reveals no hyperintense signal of the left medulla oblongata, indicating a disappearance of the edema. There are residual defects of a small ischemic infarction of the left cerebellum from the first neurovascular decompression
Immediately after surgery and for the next 3 weeks, the patient had unstable blood pressure with barely treatable increases and decreases. After this period, blood pressure was excellent with values up to 150/100 mm Hg for approximately 1 month. Two MR images during this period revealed complete resolution of the previous visible edema (Fig 2). As a complication of the neurovascular decompression, MR imaging now revealed a small ischemic area in the left cerebellum and within the Wallenberg territory. Clinically the patient showed only mild ataxia and slight weakness of the right extremities.
Two months later her blood pressure again increased to 220/140 mm Hg. MR imaging again revealed an edema of the brain stem, in a similar location as before vascular decompression (Fig 3).
Owing to these MR findings, a second surgery was performed with the same approach and the elongated vertebrobasilar complex was fixed at the occipital bone. The procedure again led to an immediate marked decrease of blood pressure (mean, 150/100 mm Hg), and the edema of the ventrolateral medulla oblongata completely disappeared. At the time of this writing, the patient's blood pressure remains at a stable level of about 150/95 mm Hg with metoprolol, candesartan cilexefil, and clonidine therapy. The patient no longer has excessive peaks of blood pressure. There were no additional neurologic symptoms after the second surgery.
Routine Doppler sonography performed after the second surgery revealed occlusion of the left vertebral artery, which was confirmed by MR angiography (Fig 4). Follow-up MR imaging 6 months later did not reveal any additional ischemic lesions in the hind-brain circulation and confirmed the total disappearance of the brain stem edema (Fig 5).
Discussion
According to the hypothesis of Janetta et al (1), arterial compression of the left ventrolateral medulla oblongata close to the root entry zone of cranial nerves IX and X by looping arteries can play an important role in the pathogenesis of essential hypertension. Furthermore, experimental results revealed that there is a mechanism of neurogenic hypertension controlled by central neurons in the lower part of the brain stem. Janetta et al were able to induce hypertensive values with a balloon model in baboons, indicating the importance of pulsatile compression of the brain stem (3). The posterior inferior cerebellar artery and the vertebral artery were found to cause hypertension in humans (4–7). So far, there have been no new findings in our patient. However, this case report highlights an important point: MR imaging can show insufficient vascular decompression of the brain stem and recurrent brain stem edema, findings which should lead to repeat surgery when vascular decompression is unsuccessful.
The literature shows that hypertension recurs in as many as 50% of patients after decompressive therapy (1, 8). Debate continues about whether such recurrence indicates a lack of response to surgery or a technical failure of the first intervention. As the follow-up of our patient indicates, the recurrence of an edema in the lower brain stem after a symptom-free interval might indicate a recurrence of vascular compression. In this type of patient with hypertension, the vertebrobasilar complex often is extremely elongated and, thus, such cases are not truly comparable with the vascular decompression seen with trigeminal neuralgia or hemispasm facialis. In these patients, repeat surgery with technically modified decompression strategy might be justified.
The excellent results in our patient (stable blood pressure, no recurrent brain stem edema) after the second operation might have been caused by the unintended occlusion of the left vertebral artery. The unintended secondary occlusion of the left vertebral artery in our patient suggests the possibility of endovascular occlusion as the primary treatment technique. Further investigation might be warranted.
In summary, we have presented a case of recurrent brain stem edema after surgical vascular decompression in a patient with neurogenic hypertension. After an initial period of normotension, the patient's blood pressure again increased to uncontrolled high levels and, on the basis of MR findings, a second operation was performed. This procedure resulted in occlusion of the left vertebral artery, stable blood pressure values, and no recurrence of the brain stem edema. We suggest that MR imaging should be used to assess the need for repeat surgery in patients with recurrent neurovascular hypertension.
Footnotes
Address reprint requests to Elke R. Gizewski, M.D.
References
- 1.Jannetta PJ, Segal R, Wolfson SK. Neurogenic hypertension: etiology and surgical treatment, I: observations in 53 patients. Ann Surg 1985;201:391-396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Morimoto S, Sasaki S, Miki S, et al. Pulsatile compression of the rostral ventrolateral medulla in hypertension. Hypertension 1997;29:514-518 [DOI] [PubMed] [Google Scholar]
- 3.Jannetta PJ, Segal R, Wolfson SK, Dujovny M, Semba A, Cook EE. Neurogenic hypertension: etiology and surgical treatment, II: observations in an experimental nonhuman primate model. Ann Surg 1985;201:391-396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kleineberg B, Becker H, Gaab MR, Naraghi R. Essential hypertension associated with neurovascular compression: angiographic findings. Neurosurgery 1992;30:834-841 [DOI] [PubMed] [Google Scholar]
- 5.Fein JM, Frishman W. Neurogenic hypertension related to vascular compression of the lateral medulla. Neurosurgery 1980;6:615-622 [DOI] [PubMed] [Google Scholar]
- 6.Colon GP, Quint DJ, Dickinson LD, et al. Magnetic resonance evaluation of ventrolateral medullary compression in essential hypertension. J Neurosurg 1998;88:226-231 [DOI] [PubMed] [Google Scholar]
- 7.Akimura T, Furutani Y, Jimi Y, et al. Essential hypertension and neurovascular compression at the ventrolateral medulla oblongata: MR evaluation. AJNR Am J Neuroradiol 1995;16:401-405 [PMC free article] [PubMed] [Google Scholar]
- 8.Wilkins RH. Neurovascular compression syndromes. Neurol Clin 1985;3:359-372 [PubMed] [Google Scholar]


