Key Points
Question
Does electroacupuncture or auricular acupuncture reduce chronic musculoskeletal pain among cancer survivors?
Findings
In this randomized clinical trial of 360 diverse cancer survivors, patients receiving electroacupuncture and auricular acupuncture had significantly greater reductions in pain scores from baseline to week 12 compared with patients receiving usual care. However, auricular acupuncture was not noninferior to electroacupuncture, and patients receiving it had more adverse events.
Meaning
Electroacupuncture and auricular acupuncture are more effective than usual care at reducing chronic musculoskeletal pain in cancer survivors.
Abstract
Importance
The opioid crisis creates challenges for cancer pain management. Acupuncture confers clinical benefits for chronic nonmalignant pain, but its effectiveness in cancer survivors remains uncertain.
Objective
To determine the effectiveness of electroacupuncture or auricular acupuncture for chronic musculoskeletal pain in cancer survivors.
Design, Setting, and Participants
The Personalized Electroacupuncture vs Auricular Acupuncture Comparative Effectiveness (PEACE) trial is a randomized clinical trial that was conducted from March 2017 to October 2019 (follow-up completed April 2020) across an urban academic cancer center and 5 suburban sites in New York and New Jersey. Study statisticians were blinded to treatment assignments. The 360 adults included in the study had a prior cancer diagnosis but no current evidence of disease, reported musculoskeletal pain for at least 3 months, and self-reported pain intensity on the Brief Pain Inventory (BPI) ranging from 0 (no pain) to 10 (worst pain imaginable).
Interventions
Patients were randomized 2:2:1 to electroacupuncture (n = 145), auricular acupuncture (n = 143), or usual care (n = 72). Intervention groups received 10 weekly sessions of electroacupuncture or auricular acupuncture. Ten acupuncture sessions were offered to the usual care group from weeks 12 through 24.
Main Outcomes and Measures
The primary outcome was change in average pain severity score on the BPI from baseline to week 12. Using a gatekeeping multiple-comparison procedure, electroacupuncture and auricular acupuncture were compared with usual care using a linear mixed model. Noninferiority of auricular acupuncture to electroacupuncture was tested if both interventions were superior to usual care.
Results
Among 360 cancer survivors (mean [SD] age, 62.1 [12.7] years; mean [SD] baseline BPI score, 5.2 [1.7] points; 251 [69.7%] women; and 88 [24.4%] non-White), 340 (94.4%) completed the primary end point. Compared with usual care, electroacupuncture reduced pain severity by 1.9 points (97.5% CI, 1.4-2.4 points; P < .001) and auricular acupuncture reduced by 1.6 points (97.5% CI, 1.0-2.1 points; P < .001) from baseline to week 12. Noninferiority of auricular acupuncture to electroacupuncture was not demonstrated. Adverse events were mild; 15 of 143 (10.5%) patients receiving auricular acupuncture and 1 of 145 (0.7%) patients receiving electroacupuncture discontinued treatments due to adverse events (P < .001).
Conclusions and Relevance
In this randomized clinical trial among cancer survivors with chronic musculoskeletal pain, electroacupuncture and auricular acupuncture produced greater pain reduction than usual care. However, auricular acupuncture did not demonstrate noninferiority to electroacupuncture, and patients receiving it had more adverse events.
Trial Registration
ClinicalTrials.gov Identifier: NCT02979574
This randomized clinical trial explores the effectiveness of electroacupuncture and auricular acupuncture compared with usual care for chronic musculoskeletal pain in cancer survivors.
Introduction
Chronic pain is a prevalent, disabling condition that costs the United States up to $635 billion in health care expenditures and lost productivity every year.1 Cancer survivors, defined as those living with a past diagnosis of cancer, are a rapidly expanding population with greater pain burden than the general public.2 Nearly 1 in 2 survivors are undertreated for pain,3,4 which contributes to poor quality of life, impaired physical function, and worse cancer-related outcomes.5 The opioid crisis has exacerbated the challenges of pain management, highlighting a need for nonpharmacological treatment options.6,7
Acupuncture is an integrative medicine technique involving the insertion of single-use, sterile needles into points on the body surface.8 In an individual-level meta-analyses of more than 18 000 patients, acupuncture demonstrated superiority over usual care and placebo controls for chronic noncancer pain.9,10 Because of the growing evidence base, the Centers for Medicare & Medicaid Services announced a decision in early 2020 to cover acupuncture for chronic lower back pain.11 A recent meta-analysis12 found that acupuncture was also associated with reduced pain in cancer populations; however, the strength of the evidence was deemed moderate owing to the small sample sizes and substantial heterogeneity of acupuncture techniques in included studies.
When acupuncture is used for pain management, inserted needles are often stimulated with electricity to enhance endogenous opioid release, a technique known as electroacupuncture.13,14 This technique is only administered by licensed practitioners with formal acupuncture training and, thus, is not widely available.15 Auricular acupuncture, a technique in which needle insertion is limited to the ears, is easier to learn and administer compared with electroacupuncture. Since 2016, the United States military has developed and taught a standardized auricular acupuncture protocol to more than 2700 health care clinicians without formal acupuncture backgrounds.16 This protocol is being implemented nationwide across the Veterans Health Administration for chronic pain management17; however, its effectiveness remains uncertain. We conducted a randomized clinical trial to compare the effectiveness of electroacupuncture and auricular acupuncture vs usual care for chronic musculoskeletal pain in cancer survivors.
Methods
Trial Design
The Personalized Electroacupuncture vs Auricular Acupuncture Comparative Effectiveness (PEACE) study is an investigator-initiated, 3-arm, parallel, randomized clinical trial that was conducted at the main urban campus of Memorial Sloan Kettering Cancer Center and 5 regional suburban sites in New York and New Jersey. Details of the trial design, recruitment and retention strategies, intervention, and procedures have been reported previously.18 The institutional review board at Memorial Sloan Kettering Cancer Center approved the trial protocol (Supplement 1), and the study followed the Consolidated Standards of Reporting Trials (CONSORT) reporting guidelines.
Patients
The trial enrolled English-speaking adults with a prior cancer diagnosis and no current evidence of disease. Patients were eligible if they experienced musculoskeletal pain for at least 3 months and at least 15 days in the preceding 30 days, and if they rated their worst pain intensity in the past week as moderate or greater (≥4 on a 0-10 numerical rating scale). Nonmusculoskeletal pain syndromes (eg, headache, visceral abdominal pain, neuropathic pain) could be present as comorbid conditions if the patient reported musculoskeletal pain as the primary source of pain. We excluded patients with inflammatory arthritis requiring disease-modifying drugs; phantom limb pain; a pending pain-related Veteran Health Administration, social security, or worker’s compensation disability claim by self-report; or an implanted electronically charged medical device.
Recruitment and Randomization
Research staff mailed recruitment letters detailing the study to potentially eligible participants identified through a search of the Memorial Sloan Kettering Cancer Center Dataline patient registry. Study clinicians met with interested patients to confirm eligibility criteria were satisfied. Patients completed written informed consent and were randomized with a 2:2:1 ratio to electroacupuncture, auricular acupuncture, or usual care, respectively. Randomization was performed through a secure system with full allocation concealment, using permuted block randomization, and stratified by accrual site and baseline opioid use. The study statisticians were blinded to treatment assignments.
Electroacupuncture
The electroacupuncture intervention was delivered by licensed acupuncturists with more than 5 years of experience in oncology settings. Acupuncturists selected 4 acupuncture points near the pain location and at least 4 additional points in other body areas to address comorbid symptoms. Acupuncturists sterilized the skin overlying the points and inserted acupuncture needles (SEIRIN) at appropriate angles to indicated depths based on patient body type and point location. All needles were manually manipulated to achieve de qi, a local sensation of soreness, numbness, or distension.19 The 4 local points were electrically stimulated at 2 Hz with an A3922 E-STIM II device (Tens Plus Industrial Company). All needles remained in place for 30 minutes. Patients received 10 treatments over 10 weeks. This standardized, semifixed electroacupuncture protocol has been previously described (eAppendix in Supplement 2).18 Acupuncture sessions were audited biweekly to ensure fidelity to the protocol.
Auricular Acupuncture
The same licensed acupuncturists who delivered electroacupuncture delivered the auricular acupuncture intervention. Acupuncturists followed a standardized protocol developed by the United States military, known as battlefield acupuncture.20 Unlike electroacupuncture, the auricular acupuncture protocol was fixed and not customized based on pain location or comorbid symptoms (eAppendix in Supplement 2). Patients’ ears were sterilized prior to needle insertion. Acupuncturists placed an ASP needle (Sedatelec) in the cingulate gyrus point on 1 ear, then instructed patients to walk for 1 minute. After the walk, the acupuncturists asked patients to rate the severity of their chronic pain. If severity remained greater than 1 out of 10, the acupuncturist placed a needle in the cingulate gyrus point of the other ear. This process was repeated for each of the remaining ear points: thalamus, omega 2, point zero, and shen men. Acupuncturists stopped placing needles if any of the following conditions were met: (1) pain severity decreased to 1 or 0 out of 10, (2) patient declined further needling, or (3) vasovagal response was observed. Up to 10 needles were administered. The total duration of each treatment session was approximately 10 to 20 minutes, depending on how many needles were administered. The needles remained in place for 3 to 4 days. Patients were instructed on how to remove the needles safely. Patients received 10 treatments over 10 weeks.
Usual Care
Patients receiving usual care received standard pain management prescribed by their health care clinicians, including analgesic medications, physical therapy, and glucocorticoid injections. Given the ethical implications of withholding a potentially beneficial treatment, patients were offered the option of receiving 10 acupuncture treatments after week 12 (duration of the primary end point).
Assessments and Outcomes
The primary end point was the change in average pain severity score on the Brief Pain Inventory (BPI) from baseline to week 12. The BPI includes 4 questions related to pain severity with response choices ranging from 0 (no pain) to 10 (pain as bad as you can imagine). The mean of these 4 items was used as the primary outcome.21 In addition to the pain severity items, the BPI contains 7 pain-related functional interference questions with response choices ranging from 0 (does not interfere) to 10 (completely interferes). Pain-related interference scores (mean of these 7 items) were assessed as a secondary outcome. Other secondary outcomes included score on the Patient-Reported Outcomes Measurement Information System–Global Health, a 10-item validated instrument for physical and mental quality of life.22,23 Participants completed assessments at weeks 0 (baseline), 4, 10, 12, 16, and 24 using REDCap (Research Electronic Data Capture) tools.24 Additionally, patients completed a week of daily pain medication diaries at those time points. A quantitative analgesic medication score was generated to calculate weekly average pain medication use throughout the study time period.25
Adverse Events
Research staff completed a standard adverse event case report form at each acupuncture treatment visit during the intervention phase. Adverse events were also assessed at subsequent follow-up visits.
Statistical Analysis
The primary hypothesis was to evaluate whether electroacupuncture or auricular acupuncture was more effective than usual care for pain severity; if both treatments were effective, then we sought to establish that auricular acupuncture was noninferior to electroacupuncture for pain reduction. Therefore, we prespecified a sequential 2-step gatekeeping multiple-testing procedure26 to maintain the overall type I error rate of α = .05 for the primary end point comparisons between arms. In step 1, we split the overall α of .05 evenly between the 2 superiority tests of electroacupuncture vs usual care and auricular acupuncture vs usual care. We planned to proceed to step 2, testing whether auricular acupuncture was noninferior to electroacupuncture, only if both of the step 1 superiority comparisons were significant at the P < .025 threshold.
The power analysis reflected this gatekeeping approach. All primary end point comparisons and power analyses were based on the week 12 treatment effect from the model described herein. For the step 1 comparisons, given a sample size of 144 in each of the acupuncture arms and 72 in the usual care arm, a 20% attrition rate across all arms by week 12, a 2-sided significance threshold of P < .025, and correlation between baseline and posttreatment assessments of 0.5, we calculated 80% power to detect a standardized mean difference of 0.48 between electroacupuncture vs usual care and auricular acupuncture vs usual care.27 Assuming an SD between 2 and 3, this effect size translates to a difference of 1 to 1.5 points on the 0-10 BPI pain severity scale. For the step 2 comparison, assuming both step 1 comparisons were significant at P < .025, we calculated 80% power to find auricular acupuncture noninferior to electroacupuncture with respect to change in BPI pain severity score within a margin of one-third change-score SDs, assuming a 1-sided significance threshold of P < .05. We expected this SD to be between 2 and 3 and for this margin to translate to between a 0.67- and 1-point difference in BPI pain severity score reduction. The minimal clinically important difference (MCID) for the BPI pain severity scale has been empirically established as an SD of 0.50 in standardized units and as 1 point in raw score units on the 0 to 10 score range.28 We chose the standardized noninferiority margin to be one-third SD because it is sufficiently smaller than the standardized BPI pain severity MCID of 0.50 SD and, given the expected SD between 2 and 3, would also result in a noninferiority margin smaller than the 1-point MCID on the BPI raw score metric. The observed SD was 1.97, and the noninferiority margin was 0.657 points.
For the analysis of the primary outcome, we prespecified a constrained linear mixed model in which we constrained the treatment arms to have a common baseline mean,29 reflecting the prerandomization timing of the baseline assessment. The dependent variable vector included the prerandomization baseline (week 0) BPI pain severity assessment and all postrandomization assessments at weeks 4, 10, 12, 16, and 24. The independent variables were the randomization stratification variables (accrual site and baseline opioid use), treatment arm, week (categorical), and the arm-by-week interaction. A patient-level random intercept was included in the model to account for the repeated outcome measurements within patients. All randomized patients with at least 1 outcome assessment were included in the model. Linear mixed models provide valid inference under the reasonable assumption that missing follow-up data were missing at random. We therefore did not impute missing values. Results are reported as least-squares means, mean differences, and confidence intervals, with inferences regarding differences between arms based on model coefficients from the arm-by-week interaction and contrasts of model-adjusted means. The 2 primary end point comparisons at week 12 between electroacupuncture vs usual care and between auricular acupuncture vs usual care are reported with 97.5% CIs; all other comparisons are reported with 95% CIs. We prespecified comparisons between arms at weeks 12 and 24. Week 12 was the first posttreatment outcome assessment and is the focus of the primary end point. Week 24 comparisons allowed for evaluating the longer-term durability of acupuncture treatment effects.
We used identical models to analyze the continuous secondary outcomes (BPI pain interference score, Patient-Reported Outcomes Measurement Information System–Global Health mental and physical component scores, and quantitative analgesic medication score). Because of the potential for inflated type I error owing to multiple comparisons, results from analyses of secondary outcomes should be interpreted as exploratory. All analyses were performed using R, version 4.0.2 (R Foundation for Statistical Computing).
Results
Patients
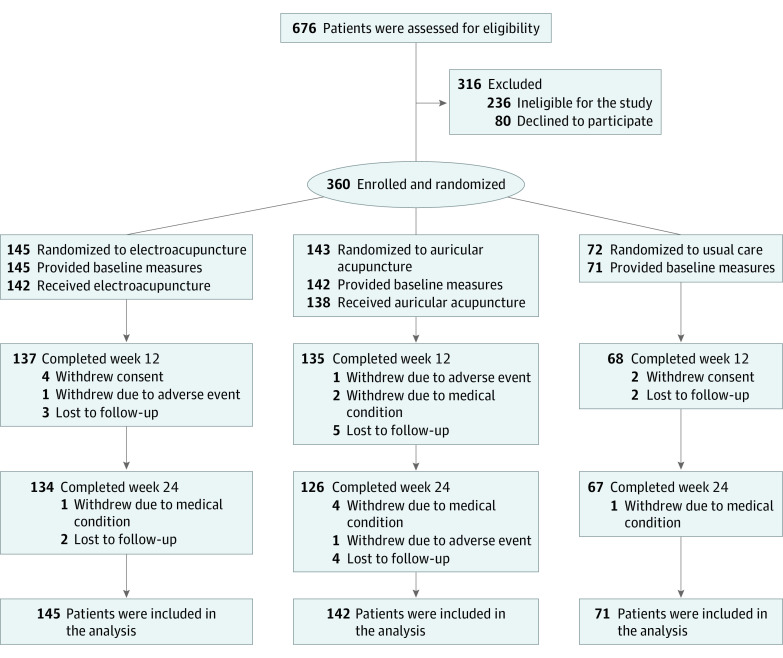
From March 2017 through October 2019, we screened 676 cancer survivors, and 316 declined to participate or were ineligible. Of the 360 enrolled patients, 145 were randomly assigned to electroacupuncture, 143 to auricular acupuncture, and 72 to usual care. Among 145 in the electroacupuncture group, 136 (93.8%) completed 8 or more treatments. Among 143 in the auricular acupuncture group, 117 (81.8%) completed 8 or more treatments. Among all participants, 20 (5.6%) withdrew from data collection at the week 12 primary end point duration (Figure 1).
Figure 1. CONSORT Diagram.
The demographic and clinical characteristics of the patients in the 3 groups were similar at baseline. The mean (SD) age of the patients was 62.1 (12.7) years, 251 (69.7%) were women, and 88 (24.4%) were non-White. The mean (SD) baseline BPI pain severity score was 5.2 (1.7) points, mean (SD) pain duration was 5.3 (6.5) years, and 210 (60.5%) patients used pain medications (Table 1 and eTable 1 in Supplement 2).
Table 1. Baseline Characteristics of Patients.
| Characteristic | No. (%) | ||
|---|---|---|---|
| Electroacupuncture (n = 145) | Auricular acupuncture (n = 143) | Usual care (n = 72) | |
| Age, mean (SD), y | 61.9 (13.2) | 62.6 (11.3) | 61.4 (14.3) |
| Sex | |||
| Male | 43 (29.7) | 49 (34.3) | 17 (23.6) |
| Female | 102 (70.3) | 94 (65.7) | 55 (76.4) |
| Race | |||
| Non-White | 42 (29.0) | 34 (23.8) | 12 (16.7) |
| White | 103 (71.0) | 109 (76.2) | 60 (83.3) |
| Ethnicity | |||
| Hispanic | 19 (13.2) | 12 (8.5) | 5 (7.0) |
| Non-Hispanic | 125 (86.8) | 130 (91.5) | 66 (93.0) |
| Cancer | |||
| Type | |||
| Breast | 66 (45.5) | 67 (46.9) | 32 (44.4) |
| Prostate | 16 (11.0) | 18 (12.6) | 7 (9.7) |
| Lymphoma | 22 (15.2) | 19 (13.3) | 10 (13.9) |
| Other | 41 (28.3) | 39 (27.2) | 23 (32.0) |
| Previous treatments | |||
| Surgery | 103 (71.0) | 103 (72.0) | 54 (75.0) |
| Chemotherapy | 57 (39.3) | 56 (39.2) | 31 (43.1) |
| Radiation | 75 (51.7) | 78 (54.5) | 35 (48.6) |
| Biological/immunotherapy | 5 (3.4) | 12 (8.4) | 1 (1.4) |
| Hormonal | 50 (34.5) | 31 (21.7) | 20 (27.8) |
| Years since cancer diagnosis, mean (SD) | 6.1 (6.5) | 6.1 (6.8) | 6.5 (7.0) |
| Duration of pain, mean (SD), ya | 5.7 (6.7) | 4.8 (6.3) | 5.5 (6.4) |
| Location of paina | |||
| Neck | 14 (9.7) | 15 (10.5) | 6 (8.3) |
| Lower back | 53 (36.6) | 44 (30.8) | 20 (27.8) |
| Shoulder/arm/elbow | 15 (10.3) | 24 (16.8) | 6 (8.3) |
| Hip/thigh | 16 (11.0) | 17 (11.9) | 9 (12.5) |
| Knee/leg | 21 (14.5) | 26 (18.2) | 17 (23.6) |
| Other | 26 (17.9) | 17 (11.8) | 14 (19.5) |
| Baseline measures | |||
| BPI pain severity score, mean (SD)b | 5.2 (1.8) | 5.0 (1.7) | 5.6 (1.5) |
| BPI interference score, mean (SD)b | 5.1 (2.4) | 4.7 (2.2) | 5.3 (2.2) |
| Taking any pain medicationsc | 83 (58.5) | 81 (59.6) | 46 (66.7) |
Abbreviation: BPI, Brief Pain Inventory.
Duration of pain symptoms and location of pain were reported by the patient and verified by clinicians before enrollment.
The BPI pain severity score (range, 0-10) was the mean of the 4 pain items. The BPI interference score (range, 0-10) was the mean of the 7 interference items.
Patients who were taking any pain medications at baseline.
Primary Outcome
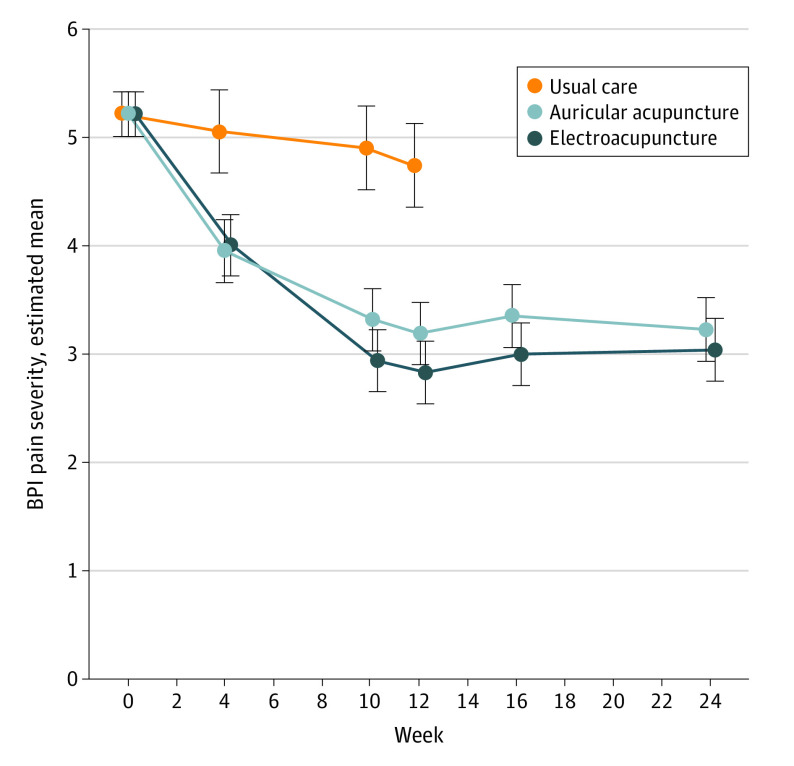
Compared with usual care, electroacupuncture reduced average BPI pain severity score by 1.9 points (97.5% CI, 1.4-2.4 points; P < .001; Cohen d, 0.97), and auricular acupuncture reduced average BPI pain severity score by 1.6 points (97.5% CI, 1.0-2.1 points; P < .001; Cohen d, 0.83) from baseline to week 12 (Figure 2 and Table 2). The reduction in BPI pain severity score was 0.36 points greater with electroacupuncture than with auricular acupuncture, and the 1-sided 95% CI bound of 0.664 exceeded the noninferiority margin of 0.657 points (P = .055); therefore, noninferiority of auricular acupuncture to electroacupuncture for pain reduction was not demonstrated. In both acupuncture groups, the reduction in average pain severity persisted until week 24 (Figure 2 and Table 2).
Figure 2. Brief Pain Inventory (BPI) Pain Severity Scores Over 24 Weeks.
The BPI pain severity scores range from 0 to 10, with higher scores indicating worse pain. Data points represent the model-estimated BPI score means, and 95% CIs (indicated by error bars) are from a linear mixed model with baseline means constrained to be equal across study arms. The dependent variable vector included the prerandomization baseline (week 0) assessment, as well as all postrandomization assessments at weeks 4, 10, 12, 16, and 24. The independent variables were the randomization stratification variables (accrual site and baseline opioid use), treatment arm, week (categorical), and the arm-by-week interaction. A patient-level random intercept was included in the model to account for the repeated outcome measurements within patients.
Table 2. Primary and Secondary Outcomes Across All Treatment Groupsa.
| Outcome | Mean (95% CI) | |||||
|---|---|---|---|---|---|---|
| Usual care | Electroacupuncture | Auricular acupuncture | Difference in change from baseline, auricular acupuncture to electroacupuncture |
|||
| Change from baseline | Change from baseline | Difference from usual care in change from baseline | Change from baseline | Difference from usual care in change from baseline | ||
| Primary outcome | ||||||
| BPI pain severity score | ||||||
| Week 12 | −0.48 (−0.85 to −0.10) | −2.39 (−2.66 to −2.12) | −1.92 (−2.43 to −1.40)b | −2.03 (−2.30 to −1.76) | −1.56 (−2.07 to −1.04)b | 0.36 (∞ to 0.665)c |
| Week 24 | NA | −2.19 (−2.46 to −1.92) | NA | −1.99 (−2.27 to −1.72) | NA | 0.20 (∞ to 0.51)d |
| Secondary outcomese | ||||||
| BPI pain interference score | ||||||
| Week 12 | −0.86 (−1.28 to −0.45) | −2.76 (−3.06 to −2.46) | −1.90 (−2.40 to −1.40) | −2.52 (−2.82 to −2.22) | −1.66 (−2.16 to −1.16) | 0.24 (−0.17 to 0.64) |
| Week 24 | NA | −2.47 (−2.77 to −2.17) | NA | −2.47 (−2.78 to −2.16) | NA | 0.00 (0.41 to −0.41) |
| PROMIS-GH physical health score | ||||||
| Week 12 | 0.41 (−0.76 to 1.58) | 4.32 (3.48 to 5.15) | 3.91 (2.49 to 5.32) | 4.50 (3.64 to 5.35) | 4.09 (2.66 to 5.51) | 0.18 (−0.98 to 1.34) |
| Week 24 | NA | 3.60 (2.77 to 4.43) | NA | 4.60 (3.73 to 5.48) | NA | 1.00 (−0.18 to 2.18) |
| PROMIS-GH mental health score | ||||||
| Week 12 | −0.73 (−2.04 to 0.58) | 1.85 (0.92 to 2.78) | 2.58 (0.99 to 4.16) | 2.71 (1.76 to 3.67) | 3.44 (1.84 to 5.04) | 0.87 (−0.44 to 2.17) |
| Week 24 | NA | 1.45 (0.52 to 2.38) | NA | 2.92 (1.94 to 3.89) | NA | 1.47 (0.15 to 2.79) |
| QAQ pain medication score | ||||||
| Week 12 | 0.13 (−0.17 to 0.43) | −0.44 (−0.66 to −0.23) | −0.57 (−0.94 to −0.21) | −0.39 (−0.61 to −0.17) | −0.52 (−0.88 to −0.15) | 0.05 (−0.25 to 0.35) |
| Week 24 | NA | −0.43 (−0.65 to −0.21) | NA | −0.28 (−0.50 to −0.06) | NA | 0.15 (−0.15 to 0.46) |
Abbreviations: BPI, Brief Pain Inventory; PROMIS-GH, Patient-Reported Outcomes Measurement Information System–Global Health; NA, not applicable; QAQ, Quantitative Analgesic Questionnaire.
For each outcome, estimates are derived from a linear mixed model with baseline means constrained to be equal across study arms. The dependent variable vector included the prerandomization baseline (week 0) assessment, as well as all postrandomization assessments at weeks 4, 10, 12, 16, and 24. The independent variables were the randomization stratification variables (accrual site and baseline opioid use), treatment arm, week (categorical), and the arm-by-week interaction. A patient-level random intercept was included in the model to account for the repeated outcome measurements within patients.
Primary end point. Point estimates with 97.5% CIs (adjusted for 2 comparisons) are presented. P < .001 for both comparisons of treatment arms with usual care for differences in BPI pain severity change from baseline to week 12.
Primary end point comparison of noninferiority of auricular acupuncture to electroacupuncture at week 12. Point estimate with 1-sided 95% CI is presented. The noninferiority margin was 0.657. The 1-sided 95% CI contains the noninferiority margin; therefore, we cannot conclude that auricular acupuncture is noninferior to electroacupuncture at the prespecified P < .05 threshold. The significance for the noninferiority test was P = .055.
Secondary end point comparison of noninferiority auricular acupuncture to electroacupuncture at week 24. Point estimate with 1-sided 95% CI is presented. The noninferiority margin was 0.657. The 1-sided 95% CI did not contain the noninferiority margin, supporting the noninferiority of auricular acupuncture to electroacupuncture at week 24 at the P < .05 threshold. The significance for the noninferiority test was P = .007. This test was not prespecified as part of the primary end point comparisons and was conducted post hoc as an exploratory analysis.
Secondary outcomes were not adjusted for multiple comparisons. Results are presented as point estimates with 95% CIs.
Secondary Outcomes
Both acupuncture groups had improved pain-related functional interference and improved physical and mental quality of life compared with the usual care group. Analgesic use decreased in both acupuncture groups at week 12 compared with the usual care group and remained decreased at week 24 relative to baseline (Table 2). Additional data related to primary and secondary outcomes are available in eTables 1 and 2 in Supplement 2.
Adverse Events
Adverse events were mild to moderate in both acupuncture groups. Among patients receiving electroacupuncture, bruising was the most common adverse event and was reported by 15 of 145 (10.3%) patients. Among patients receiving auricular acupuncture, ear pain was the most common adverse event and was reported by 27 of 143 (18.9%) patients. In the electroacupuncture group, 1 of 145 (0.7%) patients discontinued treatment due to an adverse event. In the auricular acupuncture group, 15 of 143 (10.5%) patients discontinued treatment due to adverse events (P < .001).
Discussion
Chronic pain is a common and challenging condition. In this randomized clinical trial of diverse cancer survivors with chronic musculoskeletal pain, electroacupuncture and auricular acupuncture improved pain severity, pain-related functional interference, and quality of life, and reduced analgesic use compared with usual care. While both acupuncture techniques were effective, auricular acupuncture had higher treatment discontinuation rates than electroacupuncture and did not meet criteria for noninferiority to electroacupuncture.
The magnitude of effect of electroacupuncture was clinically important and durable.28 This finding is consistent with evidence from other large acupuncture trials for chronic pain in the general population.10 Electroacupuncture has been shown to influence endogenous opioid release, which provides a mechanistic basis for chronic pain management.13,14 The present trial includes a large and diverse group of cancer survivors and provides evidence that electroacupuncture produces additional benefits beyond usual care, including not only reductions in pain severity, but also improvements in physical function and quality of life and reductions in analgesic use.
Battlefield acupuncture is a novel auricular acupuncture technique that has been standardized and successfully implemented across Veterans Health Administration settings with preliminary reports of effectiveness17; however, evidence from large randomized clinical trials was previously lacking. The present trial provides evidence that auricular acupuncture confers short-term and long-term benefits for pain management in cancer survivors. The effect size of auricular acupuncture compared with usual care is similar to or larger than that reported in meta-analyses conducted by the Acupuncture Trialist Group (N = 20 827).10 In addition, the absolute difference in pain reduction between auricular acupuncture and electroacupuncture observed in the present trial is small; therefore, it may not be clinically relevant. Unfortunately, 1 in 10 patients were unable to tolerate the ear discomfort from needling; thus, future research is needed to predict who may not tolerate it and understand how to administer this technique safely to mitigate adverse effects. The medical workforce could potentially be equipped with this technique to expand nonpharmacological treatment options in settings where electroacupuncture is not widely available.
Previous acupuncture trials in cancer populations often had small sample sizes, short follow-up, or an exclusive focus on a specific cancer type.12,30 This trial demonstrated the beneficial effects of electroacupuncture and auricular acupuncture for pain in a diverse sample of cancer survivors in terms of gender, tumor types, treatment histories, and minority representation. Although Medicare now covers acupuncture for chronic low back pain,11 cancer survivors often experience other types of chronic pain from cancer treatments, such as surgery, radiation, and hormonal therapies. Insurance coverage for acupuncture beyond low back pain will be essential to ensure survivors have access to nonpharmacological interventions to manage pain.
Limitations
This trial has limitations. First, it compared 2 types of acupuncture against usual care without a sham control; lack of blinding to patients or health care clinicians can introduce bias. However, acupuncture has been found to be superior to sham controls in prior studies.9,10 Second, experienced acupuncturists delivered the interventions, so the effects may differ if nonacupuncturist clinicians deliver auricular acupuncture. Third, we did not test whether combining these 2 acupuncture interventions would yield better results or whether nonresponders to 1 technique would respond to the other technique. Finally, this study was conducted in an academic cancer center with urban and suburban locations. Future research in the community, especially in underserved and rural settings, is needed to determine its generalizability.
Conclusions
In this randomized clinical trial, electroacupuncture and auricular acupuncture effectively reduced the severity of chronic musculoskeletal pain in a diverse population of cancer survivors compared with usual care. However, auricular acupuncture had higher treatment discontinuation rates than electroacupuncture and did not demonstrate noninferiority to electroacupuncture.
Trial Protocol
eAppendix. Acupuncture Intervention
eTable 1. Descriptive Statistics of Pain Outcome Measures, by Week and Arm
eTable 2. Primary and Secondary Outcomes (extended version of manuscript Table 2)
Data Sharing Statement
References
- 1.Steglitz J, Buscemi J, Ferguson MJ. The future of pain research, education, and treatment: a summary of the IOM report “Relieving pain in America: a blueprint for transforming prevention, care, education, and research”. Transl Behav Med. 2012;2(1):6-8. doi: 10.1007/s13142-012-0110-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mao JJ, Armstrong K, Bowman MA, Xie SX, Kadakia R, Farrar JT. Symptom burden among cancer survivors: impact of age and comorbidity. J Am Board Fam Med. 2007;20(5):434-443. doi: 10.3122/jabfm.2007.05.060225 [DOI] [PubMed] [Google Scholar]
- 3.Deandrea S, Montanari M, Moja L, Apolone G. Prevalence of undertreatment in cancer pain. A review of published literature. Ann Oncol. 2008;19(12):1985-1991. doi: 10.1093/annonc/mdn419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.van den Beuken-van Everdingen MH, Hochstenbach LM, Joosten EA, Tjan-Heijnen VC, Janssen DJ. Update on prevalence of pain in patients with cancer: systematic review and meta-analysis. J Pain Symptom Manage. 2016;51(6):1070-1090.e9. doi: 10.1016/j.jpainsymman.2015.12.340 [DOI] [PubMed] [Google Scholar]
- 5.Zylla D, Steele G, Gupta P. A systematic review of the impact of pain on overall survival in patients with cancer. Support Care Cancer. 2017;25(5):1687-1698. doi: 10.1007/s00520-017-3614-y [DOI] [PubMed] [Google Scholar]
- 6.Paice JA. Managing pain in patients and survivors: challenges within the united states opioid crisis. J Natl Compr Canc Netw. 2019;17(5.5):595-598. doi: 10.6004/jnccn.2019.5010 [DOI] [PubMed] [Google Scholar]
- 7.Vitzthum LK, Riviere P, Murphy JD. Managing cancer pain during the opioid epidemic-balancing caution and compassion. JAMA Oncol. 2020;6(7):1103-1104. doi: 10.1001/jamaoncol.2020.0779 [DOI] [PubMed] [Google Scholar]
- 8.Kaptchuk TJ. Acupuncture: theory, efficacy, and practice. Ann Intern Med. 2002;136(5):374-383. doi: 10.7326/0003-4819-136-5-200203050-00010 [DOI] [PubMed] [Google Scholar]
- 9.Vickers AJ, Cronin AM, Maschino AC, et al. ; Acupuncture Trialists’ Collaboration . Acupuncture for chronic pain: individual patient data meta-analysis. Arch Intern Med. 2012;172(19):1444-1453. doi: 10.1001/archinternmed.2012.3654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vickers AJ, Vertosick EA, Lewith G, et al. ; Acupuncture Trialists’ Collaboration . Acupuncture for chronic pain: update of an individual patient data meta-analysis. J Pain. 2018;19(5):455-474. doi: 10.1016/j.jpain.2017.11.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.CMS finalizes decision to cover acupuncture for chronic low back pain for Medicare beneficiaries. News release. Centers for Medicare & Medicaid Services. January 21, 2020. Accessed February 10, 2021. https://www.cms.gov/newsroom/press-releases/cms-finalizes-decision-cover-acupuncture-chronic-low-back-pain-medicare-beneficiaries
- 12.He Y, Guo X, May BH, et al. Clinical evidence for association of acupuncture and acupressure with improved cancer pain: a systematic review and meta-analysis. JAMA Oncol. 2020;6(2):271-278. doi: 10.1001/jamaoncol.2019.5233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ulett GA, Han S, Han JS. Electroacupuncture: mechanisms and clinical application. Biol Psychiatry. 1998;44(2):129-138. doi: 10.1016/S0006-3223(97)00394-6 [DOI] [PubMed] [Google Scholar]
- 14.Zhang R, Lao L, Ren K, Berman BM. Mechanisms of acupuncture-electroacupuncture on persistent pain. Anesthesiology. 2014;120(2):482-503. doi: 10.1097/ALN.0000000000000101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fan AY, Stumpf SH, Faggert Alemi S, Matecki A. Distribution of licensed acupuncturists and educational institutions in the United States at the start of 2018. Complement Ther Med. 2018;41:295-301. doi: 10.1016/j.ctim.2018.10.015 [DOI] [PubMed] [Google Scholar]
- 16.Niemtzow R, Baxter J, Gallagher RM, et al. Building capacity for complementary and integrative medicine through a large, cross-agency, acupuncture training program: lessons learned from a military health system and veterans health administration joint initiative project. Mil Med. 2018;183(11-12):e486-e493. doi: 10.1093/milmed/usy028 [DOI] [PubMed] [Google Scholar]
- 17.Zeliadt SB, Thomas ER, Olson J, et al. Patient feedback on the effectiveness of auricular acupuncture on pain in routine clinical care: the experience of 11,406 veterans. Med Care. 2020;58(suppl 2 9S):S101-S107. doi: 10.1097/MLR.0000000000001368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liou KT, Baser R, Romero SAD, et al. Personalized electro-acupuncture versus auricular-acupuncture comparative effectiveness (PEACE): a protocol of a randomized controlled trial for chronic musculoskeletal pain in cancer survivors. Medicine (Baltimore). 2020;99(21):e20085. doi: 10.1097/MD.0000000000020085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mao JJ, Farrar JT, Armstrong K, Donahue A, Ngo J, Bowman MA. De qi: Chinese acupuncture patients’ experiences and beliefs regarding acupuncture needling sensation—an exploratory survey. Acupunct Med. 2007;25(4):158-165. doi: 10.1136/aim.25.4.158 [DOI] [PubMed] [Google Scholar]
- 20.Niemtzow RC. Battlefield acupuncture: my story. Med Acupunct. 2018;30(2):57-58. doi: 10.1089/acu.2018.29077.rcn [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cleeland CS, Ryan KM. Pain assessment: global use of the Brief Pain Inventory. Ann Acad Med Singap. 1994;23(2):129-138. [PubMed] [Google Scholar]
- 22.Hays RD, Bjorner JB, Revicki DA, Spritzer KL, Cella D. Development of physical and mental health summary scores from the patient-reported outcomes measurement information system (PROMIS) global items. Qual Life Res. 2009;18(7):873-880. doi: 10.1007/s11136-009-9496-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Revicki DA, Kawata AK, Harnam N, Chen WH, Hays RD, Cella D. Predicting EuroQol (EQ-5D) scores from the patient-reported outcomes measurement information system (PROMIS) global items and domain item banks in a United States sample. Qual Life Res. 2009;18(6):783-791. doi: 10.1007/s11136-009-9489-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377-381. doi: 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Robinson-Papp J, George MC, Wongmek A, et al. The Quantitative Analgesic Questionnaire: a tool to capture patient-reported chronic pain medication use. J Pain Symptom Manage. 2015;50(3):381-386. doi: 10.1016/j.jpainsymman.2015.03.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dmitrienko A, Millen BA, Brechenmacher T, Paux G. Development of gatekeeping strategies in confirmatory clinical trials. Biom J. 2011;53(6):875-893. doi: 10.1002/bimj.201100036 [DOI] [PubMed] [Google Scholar]
- 27.Lu K, Luo X, Chen P-Y. Sample size estimation for repeated measures analysis in randomized clinical trials with missing data. Int J Biostat. 2008;4(1):9. doi: 10.2202/1557-4679.1098 [DOI] [PubMed] [Google Scholar]
- 28.Dworkin RH, Turk DC, Wyrwich KW, et al. Interpreting the clinical importance of treatment outcomes in chronic pain clinical trials: IMMPACT recommendations. J Pain. 2008;9(2):105-121. doi: 10.1016/j.jpain.2007.09.005 [DOI] [PubMed] [Google Scholar]
- 29.Liu GF, Lu K, Mogg R, Mallick M, Mehrotra DV. Should baseline be a covariate or dependent variable in analyses of change from baseline in clinical trials? Stat Med. 2009;28(20):2509-2530. doi: 10.1002/sim.3639 [DOI] [PubMed] [Google Scholar]
- 30.Hershman DL, Unger JM, Greenlee H, et al. Effect of acupuncture vs sham acupuncture or waitlist control on joint pain related to aromatase inhibitors among women with early-stage breast cancer: a randomized clinical trial. JAMA. 2018;320(2):167-176. doi: 10.1001/jama.2018.8907 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Trial Protocol
eAppendix. Acupuncture Intervention
eTable 1. Descriptive Statistics of Pain Outcome Measures, by Week and Arm
eTable 2. Primary and Secondary Outcomes (extended version of manuscript Table 2)
Data Sharing Statement