Abstract
Summary: Traumatic posterior circulation aneurysms are rare, especially in children. They are typically associated with severe trauma and are thought to result from either direct osseous injury or stretching or compression of an artery against the tentorium. They may grow, rupture, or both. Although spontaneous thrombosis may occur, it rarely results in complete occlusion. We report the spontaneous and complete thrombosis of a large posterior cerebral artery aneurysm in a child who presented after minor head trauma. Five-year follow-up documents the complete occlusion of the aneurysm.
Traumatic aneurysms comprise <1% of all intracranial aneurysms and are usually found in the anterior circulation (1, 2). They most commonly occur in the distal middle cerebral or anterior cerebral artery or in the petrous or cavernous portion of the internal carotid artery, with posterior circulation aneurysms accounting for only 7–10% of these lesions (3). They usually occur as a consequence of severe head trauma. In closed injuries, one of the possible causes is arterial injury because of a sudden stretching or compression against a rigid dural structure such as the falx or the tentorium. These aneurysms often bleed, with intracranial hemorrhage reported in as many as 60% of patients with such aneurysms (3). Associated mortality is as high as 31% (4). Some degree of spontaneous thrombosis may occur (5).
Case Report
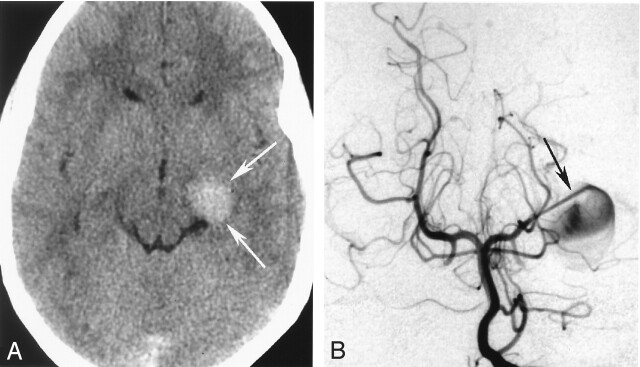
A 6-year-old boy was seen in the emergency room after a fall from a swing. He had a mild headache and a slight contusion over his forehead. He had not lost consciousness, and his physical and neurologic examinations were normal. A CT scan demonstrated a hyperattenuated, round lesion in the left ambient cistern (Fig 1A).
Fig 1.
A, Initial CT scan. Axial CT scan shows hyperattenuated round lesion (arrows) adjacent to the left ambient cistern with slight compression of the brain stem. B, Initial arteriogram. Left vertebral arteriogram, anteroposterior view, shows a contrast medium “jet” filling (arrow) of a large aneurysm arising from the left P2 segment.
Angiography 2 days later revealed a 20-mm aneurysm arising from the P2 segment of the left posterior cerebral artery (PCA; Fig 1B). Cortical branches of the PCA arose from the aneurysm. The images were interpreted as representing a posttraumatic aneurysm with cortical branches filling from the aneurysm. It was not thought to be possible to occlude the aneurysm without sacrificing the parent artery. Because of the high risk of rupture, occlusion of the parent artery by using endovascular techniques was recommended. Because of concern about the risks of treatment, the parents requested a second opinion. After these consultants agreed with the original recommendation, the parents wished to proceed with treatment. Before readmission (15 days after initial evaluation), the child developed a significant increase in his headache. He also had nausea and vomiting, but no focal neurologic deficit. A CT scan showed a marked increase in the attenuation of the aneurysm. This was interpreted as indicating significant thrombosis (Fig 2). Angiography done the next day showed total occlusion of the aneurysm with preservation of the parent artery and its branches (not shown).
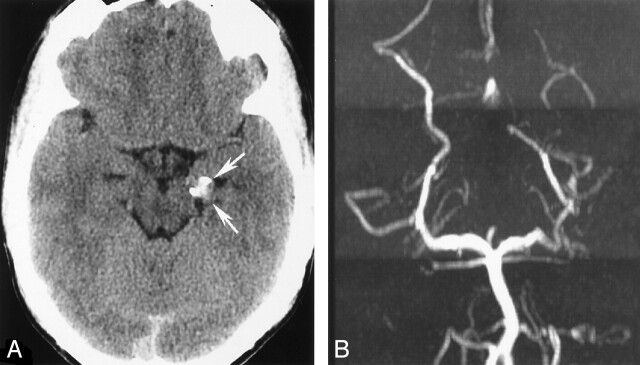
Fig 2.

Follow-up CT scan. Axial CT scan shows increased hyperattenuation of the lesion (arrows), indicating acute thrombosis.
Serial CT and MR imaging scans done over the ensuing 5 years showed a gradual shrinking and calcification of the thrombosed aneurysm (Fig 3A and B). The child remained neurologically normal.
Fig 3.
A, Follow-up axial CT scan, obtained 5 years later, demonstrating the shrinkage of the lesion associated with some calcifications. B, Follow-up MR angiogram obtained 5 years later. MR angiogram documents no recanalization of the aneurysm and partial filling of distal PCA branches.
Discussion
Intracranial aneurysms in children are uncommon, accounting for 0.5–4.6% of all aneurysms (6). Among them, traumatic aneurysms account for as many as 39%. Of 500 cases of traumatic intracranial aneurysms reported in the literature, >60 occurred in children younger than 10 years old (3). Intracranial aneurysms most frequently involve the distal anterior cerebral artery (38%), the internal carotid artery (29%) at the level of the skull base, usually the supraclinoid segment, or the distal middle cerebral artery (25%). Only a few cases (8%) involving the posterior circulation have been reported (3, 7). Intracranial traumatic aneurysms usually develop as a consequence of direct vessel injury associated with fractures, penetrating wounds, or acceleration-induced shear forces. Closed head injuries leading to traumatic aneurysms are relatively common in children, accounting for 68–72% of cases (3). Minor head trauma, without fractures or significant initial impairment of consciousness, may also cause vessel injury. The underlying mechanism in these instances is either a direct compression or a sudden stretching of the vessel wall against stationary structures. Aneurysms arising from such an injury occur most commonly in arteries that are closely related to the falx cerebri (anterior cerebral artery), the tentorium (PCA, superior cerebellar artery), or the falx cerebelli (posterior inferior cerebellar artery).
Casey and Moore (8) reported the case of a 24-year-old man with a traumatic giant PCA aneurysm mimicking a tentorial edge meningioma. Kaplan and Hahn (9) described nonruptured PCA aneurysms in two children, both 4 years old. Kaplan and Hahn’s review of the literature contains 21 published cases of PCA aneurysms under the age of 20, seven younger than 10 years of age, and 10 presenting without subarachnoid hemorrhage. Although the angiographic appearance in one of his cases (case 1) is somewhat similar to ours, closed head injury or minor head trauma was not noted as a possible cause. De Sousa et al (10), who described a ruptured nontraumatic giant PCA aneurysm, found only 10 previously published cases in children 5 years of age or younger.
Burton et al (11) reported that so far, the only case of a PCA aneurysm in a child of traumatic origin. A 14-year-old boy developed an aneurysm of the right temporooccipital branch following an automobile accident. Although he was asymptomatic until the time of his minor trauma, it cannot be excluded that the aneurysm was present before this event and that it may not have been of a traumatic origin.
As stated by Stehbens (12) most aneurysms >10 mm in diameter contain thrombus. The incidence of some degree of spontaneous thrombosis of all aneurysms varies depending on location, size, and origin, but it is higher in giant aneurysms (13). Ohta (14) analyzed 30 cases of distal superior cerebellar artery aneurysms from the literature. Seven cases (23%) showed partial intraaneurysmal thrombosis, and one was completely thrombosed.
In general, complete aneurysm thrombosis is more unusual (5, 14–19) and is particularly rare in a short period of time (1 month) (17, 18). It may, however, occur even within a few days (20).
To the best of our knowledge, only one instance of spontaneous thrombosis of a traumatic aneurysm in a child has been reported (5). Loevner et al (5) described the case of a 7-year-old boy with a traumatic basilar artery aneurysm that showed complete thrombosis confirmed by a follow-up arteriogram after 13 years. Various factors influence the spontaneous thrombosis of an aneurysm, the most important of which is likely the relationship between volume and neck size (13, 21). In a now classic study in a canine aneurysm model, Black and German (21) demonstrated that the volume-to-orifice ratio of the aneurysm appear to be the major contributing factor to the balance between thrombogenesis and thrombolysis. In this study of 21 aneurysms none of those with a volume-to-area quotient of less than 23 thrombosed (n = 8), whereas all of those with a volume-to-area quotient of 28 or greater thrombosed completely (n = 11). The larger the volume with respect to the neck, the more sluggish flow inside the aneurysm. A volume-to-area quotient >25 seemed to provoke spontaneous thrombosis. Our patient’s aneurysm was large (18 mm). It filled and emptied very slowly, which indicates very sluggish intraaneurysmal flow.
Another factor that has been related to spontaneous aneurysm thrombosis is the contrast medium used for angiography. Recently, Krapf et al (15) reported the complete disappearance of a giant posterior communicating artery aneurysm in a 9-month-year-old infant following diagnostic angiography. Warschewske et al (18) reported the complete thrombosis of a giant anterior communicating artery aneurysm 4 weeks after diagnostic angiography. Although the underlying mechanisms are not completely understood, nonionic contrast media may interact with clotting (endothelium, platelets, and red blood cells) so as to cause activation of coagulation or thrombosis (22, 23). Particularly under low-flow conditions as was present in our patient; they may induce red blood cell aggregation and thus may also promote thrombosis by this mechanism (23, 24). Because we do not have definitive proof that this aneurysm was not present before the trauma, we cannot exclude the possibility that, in some manner, the injury initiated events that led to its thrombosis. Because one cannot predict whether a particular aneurysm will thrombose, and because the incidence of rupture of traumatic aneurysms is high, it is not appropriate to manage these patients in a conservative manner in the hope that spontaneous thrombosis will occur.
Conclusion
We report the rapid, spontaneous, and complete thrombosis of a nonruptured, large posttraumatic aneurysm of the PCA in a child. MR imaging and CT examinations over a 5-year period confirmed the permanent obliteration of the aneurysm.
Acknowledgments
We wish to thank Ramin Naeini for his help in performing the literature search.
References
- 1.Benoit BG, Wortzman G. Traumatic cerebral aneurysms: clinical features and natural history. J Neurol Neurosurg Psychiatry 1973;36:127–138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nakstad P, Nornes H, Hauge HN. Traumatic aneurysms of the pericallosal arteries. Neuroradiology 1986;28:335–338 [DOI] [PubMed] [Google Scholar]
- 3.Ventureyra EC, Higgins MJ. Traumatic intracranial aneurysms in childhood and adolescence: case reports and review of the literature. Childs Nerv Syst 1994;10:361–379 [DOI] [PubMed] [Google Scholar]
- 4.Buckingham MJ, Crone KR, Ball WS, et al. Traumatic intracranial aneurysms in childhood: two cases and a review of the literature. Neurosurgery 1988;22:398–408 [DOI] [PubMed] [Google Scholar]
- 5.Loevner LA, Ting TY, Hurst RW, et al. Spontaneous thrombosis of a basilar artery traumatic aneurysm in a child. AJNR Am J Neuroradiol 1998;19:386–388 [PMC free article] [PubMed] [Google Scholar]
- 6.Kanaan I, Lasjaunias P, Coates R. The spectrum of intracranial aneurysms in pediatrics. Minim Invasive Neurosurg 1995;38:1–9 [DOI] [PubMed] [Google Scholar]
- 7.Raju BS, Purohit AK, Murthy SR, et al. Traumatic distal anterior cerebral artery aneurysm in a child: a case report. Neurol India 2001;49:295–298 [PubMed] [Google Scholar]
- 8.Casey AT, Moore AJ. A traumatic giant posterior cerebral artery aneurysm mimicking a tentorial edge meningioma. Br J Neurosurg 1994;8:97–99 [DOI] [PubMed] [Google Scholar]
- 9.Kaplan PA, Hahn FJ. Aneurysms of the posterior cerebral artery in children. AJNR Am J Neuroradiol 1984;5:771–774 [PMC free article] [PubMed] [Google Scholar]
- 10.de Sousa AA, Dantas FL, Neto AP, Carvalho GT. Giant posterior cerebral artery aneurysm in a 4-year-old child: Case report. Surg Neurol 1996;45:31–35 [DOI] [PubMed] [Google Scholar]
- 11.Burton C, Velasco F, Dorman J. Traumatic aneurysm of a peripheral cerebral artery: review and case report. J Neurosurg 1968;28:468–474 [DOI] [PubMed] [Google Scholar]
- 12.Stehbens WE. Aneurysms and anatomical variation of cerebral arteries. Arch Pathol 1963;75:45–64 [PubMed] [Google Scholar]
- 13.Whittle IR, Dorsch NW, Besser M. Spontaneous thrombosis in giant intracranial aneurysms. J Neurol Neurosurg Psychiatry 1982;45:1040–1047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ohta H, Sakai N, Nagata I, et al. Spontaneous total thrombosis of distal superior cerebellar artery aneurysm. Acta Neurochir 2001;143:837–842 [DOI] [PubMed] [Google Scholar]
- 15.Krapf H, Schoning M, Petersen D, Kuker W. Complete asymptomatic thrombosis and resorption of a congenital giant intracranial aneurysm. J Neurosurg 2002;97:184–189 [DOI] [PubMed] [Google Scholar]
- 16.Nagasawa S, Kobata H, Aoki J, et al. A large thrombosed superior cerebellar artery aneurysm: a case report. Surg Neurol 1996;45:36–38 [DOI] [PubMed] [Google Scholar]
- 17.Gerber S, Dormont D, Sahel M, et al. Complete spontaneous thrombosis of a giant intracranial aneurysm. Neuroradiology 1994;36:316–317 [DOI] [PubMed] [Google Scholar]
- 18.Warschewske G, Benndorf G, Lehmann T, Lanksch W. Spontaneous occlusion of a giant aneurysm within 4 weeks: documented by angiography. Interv Neuroradiol 1999;5:327. [DOI] [PubMed] [Google Scholar]
- 19.Choudhury AR, al Amiri NH, al Moutaery KR, et al. Giant middle cerebral aneurysm presenting as hemiathetosis in a child and its spontaneous thrombosis. Childs Nerv Syst 1991;7:59–61 [DOI] [PubMed] [Google Scholar]
- 20.Carlson DH, Thomson D. Spontaneous thrombosis of a giant cerebral aneurysm in five days: report of a case. Neurology 1976;26:334–336 [DOI] [PubMed] [Google Scholar]
- 21.Black S, German W. Observations of the relationship between the volume and the size of the orifice of the experimental aneurysms. J Neurosurg 1960;17:984–990 [DOI] [PubMed] [Google Scholar]
- 22.Hay KL, Bull BS. Factors influencing the activation of platelets by nonionic contrast medium. J Vasc Interv Radiol 1996;7:401–407 [DOI] [PubMed] [Google Scholar]
- 23.Eloy R. Thromboembolic risks in angiography: role of idionated contrast media. Heidelberg: Springer-Verlag;1990
- 24.Konus OL, Ilgit ET, Ozdemir A, Onal B. Spontaneous thrombosis of a vein of Galen aneurysmal malformation: possible effects of contrast media. Eur Radiol 2000;10:1456–1458 [DOI] [PubMed] [Google Scholar]