Abstract
Summary: Rosai-Dorfman disease (sinus histiocytosis with massive lymphadenopathy) is a rare benign idiopathic proliferative disease of phagocytic histiocytes. Approximately 80% of patients present with painless massive cervical lymphadenopathy. Isolated extranodal involvement is relatively uncommon. Two cases of Rosai-Dorfman disease are reported: one with isolated bilateral orbital involvement and one with marked cervical lymphadenopathy and multiple dural-based and intraventricular masses.
Rosai and Dorfman (1) first described the rare disease entity sinus histiocytosis with massive lymphadenopathy, also referred to as Rosai-Dorfman disease (RDD), in 1969. Rosai-Dorfman disease predominantly affects children and young adults, with slight male predominance (1, 2). Most (83%–95%) patients have painless bilateral cervical lymphadenopathy, but a few present with isolated extranodal disease; as such, some have proposed preferential use of the term “Rosai-Dorfman disease” over “sinus histiocytosis with massive lymphadenopathy”. In their latest review of the disease, Rosai and Dorfman list 43% of patients as having at least one site of extranodal involvement (2). These sites include the respiratory tract, skin, nasal cavity, orbit and eyelid, and skeletal system. While rare, intracranial involvement has been reported in several cases (3–5). Although the entity is well described in the clinical literature, few imaging findings have been reported (4, 6). We report two cases of RDD: one with isolated bilateral orbital involvement, and one with intracranial involvement.
Case Reports
Case 1
At age 5, this 19-year-old Indian woman presented with proptosis initially diagnosed as orbital pseudotumor. Despite treatment with steroids and radiation during childhood, the patient's proptosis worsened during the next 12 years with eventual decrease in visual acuity. Physical examination revealed marked proptosis with limited extraocular muscle movement. She could not fully close her eyes, and bilateral conjunctival exposure and chemosis were seen inferiorly. No cervical lymphadenopathy was present, and no weight loss or fever was noted. Laboratory results at time of presentation included a white blood cell count of 29,000/mm3 and indications of microcytic anemia. Contrast-enhanced CT of the orbit demonstrated large heterogeneously enhancing orbital soft-tissue masses with striking exophthalmos. The right optic nerve was stretched and bowed by the abnormal orbital soft tissue, with additional flattening of the globes noted (Fig 1). Hyperostosis of the orbital wall was demonstrated, as was expansion of the infraorbital foramina and right sphenopalatine foramen. Enhancing soft tissue also involved the medial canthal regions, as well as the nasal cavity, ethmoid and maxillary sinuses, and infratemporal fossae (Fig 1). The patient underwent a debulking procedure of the right orbit, with biopsy, which yielded firm, tan, slightly fibrous tissue demonstrating a mixed histiocytic and lymphocytic infiltrate with additional findings of lymphocytophagocytosis (Fig 2). Initiation of a vinblastine and prednisone regimen resulted in only a very slight decrease in size of the patient's orbital masses but did allow for a slight improvement in her vision; 6-mercaptopurine was later added to her treatment regimen with little subsequent improvement.
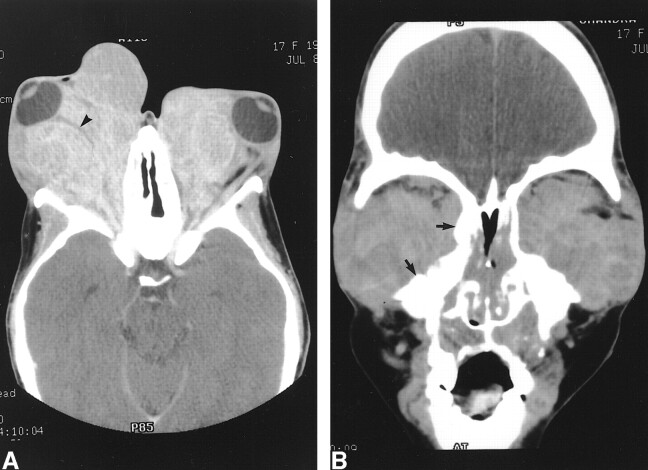
fig 1.
Case 1, extranodal orbital involvement in Rosai-Dorfman disease. Axial (A) image from contrast-enhanced CT scan demonstrates abnormal, heterogeneously enhancing orbital soft tissue, producing marked bilateral exophthalmos and bowing of the right optic nerve (arrows). Coronal (B) image from the same examination reveals involvement of the ethmoid and maxillary sinuses, and the nasal cavity, with prominent orbital floor hyperostosis, and demineralization of the turbinates
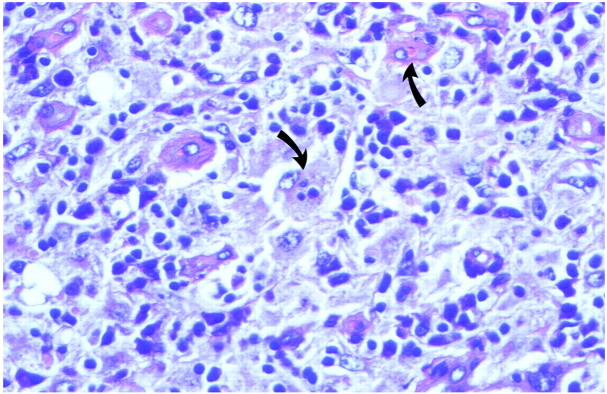
fig 2.
Case 1, histologic sample from left orbital mass. High-power image (hematoxylin and eosin stain) from excisional biopsy demonstrates abundant histiocytes with lymphocytic infiltrate. A few histiocytes exhibit lymphophagocytosis (arrows), characteristic of Rosai-Dorfman disease
Case 2
A 38-year-old man presented with pain and swelling involving the proximal right thigh that was persistent despite antibiotic treatment. Cervical, axillary, and inguinal lymphadenopathy, as well as lower extremity and scrotal edema, subsequently developed. A subcutaneous nodule over the right flank was noted. Laboratory findings included mild leukocytosis, mild microcytic anemia, and a slightly elevated erythrocyte sedimentation rate. A CT examination of the neck at this time revealed extensive bilateral cervical adenopathy involving nearly all lymph node groups (Fig 3). In addition, there were multiple dural-based enhancing lesions at the right frontal and right temporal regions, and at the atrium of the left lateral ventricle and the fourth ventricle. Abdominal and pelvic CT demonstrated extensive retroperitoneal lymphadenopathy resulting in hydronephrosis of the right kidney secondary to obstruction of the proximal and mid-right ureter. A cervical node biopsy demonstrated foamy cell histiocytosis and lymphocytophagocytosis. A biopsy of the intracranial lesions was not performed. Despite initiation of treatment with prednisone, cyclophosphamide, and vincristine, the patient's symptoms did not remit, and right ureteral stent placement for ureteral obstruction was performed. A change in regimen to melphalan and prednisone resulted in a slight decrease in overall nodal enlargement, but lymphadenopathy and lower extremity and scrotal edema persisted.
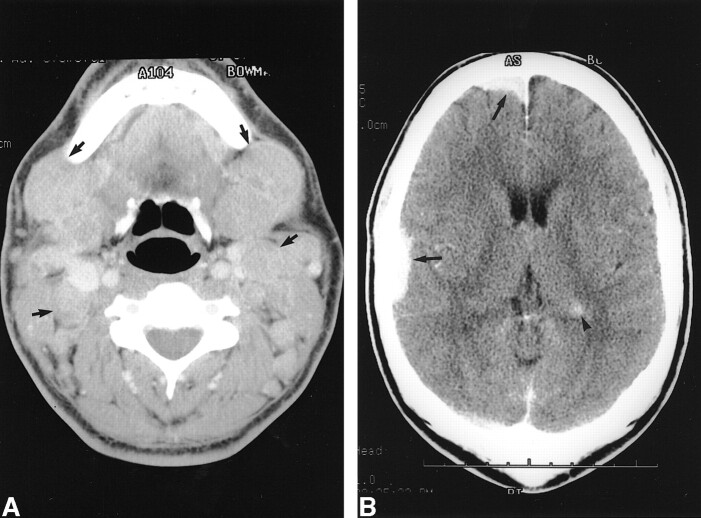
fig 3.
Case 2, extranodal cervical nodal involvement in Rosai-Dorfman disease. Axial images (A and B) from contrast-enhanced demonstrate prominent cervical lymphadenopathy bilaterally, involving multiple nodal groups, including submandibular and posterior cervical nodes.
Discussion
Since 1969, when Rosai and Dorfman first described a rare benign lymphoproliferative disease, then referred to as sinus histiocytosis with massive lymphadenopathy and now known primarily as Rosai-Dorfman disease (1), there have been 423 cases registered. Among them, 40 cases had some evidence of orbital and/ or eyelid involvement. Only seven of these 40 revealed no evidence of lymphadenopathy, including our Case 1. Most patients presented with proptosis, limited eye movement, eyelid edema, epiphora, and decreased visual acuity. Orbital involvement is usually unilateral (7), and bilateral diffuse involvement, as noted in our first case, is rare (8). Appearance of orbital involvement during imaging has been reported in a few cases (5, 7, 8). The lesion usually appears as an infiltrative soft-tissue mass with variable contrast enhancement. Fatty infiltration within the orbital mass is occasionally seen. Some cases have both eyelid and orbital involvement with extensive preseptal and postseptal masses, but lesions can be purely retrobulbar. Lacrimal gland involvement also has been reported, as has direct intracranial extension through the orbital apex to the middle cranial fossa. Sclerotic bone changes of the orbital wall are seen in this case, which might indicate a slow-growing benign process causing bone remodeling. In one case report describing the MR appearance of this lesion, the lesion was noted as being isointense to gray matter (6) with homogeneous contrast enhancement. A differential diagnosis based on a diffuse infiltrating orbital mass includes orbital pseudotumor, lymphoma, sarcoidosis, lymphangioma, or hemangioma.
Although intracranial involvement in RDD is rare, there have been several cases reported (6–8). The most common imaging appearance of intracranial RDD is a dural-based enhancing mass, mimicking a meningioma. A recent case report, however, describes a case of RDD involving the suprasellar cistern, similar to sarcoidosis or Langhan's cells histiocytosis (4). Case 2 in our study had multiple intracranial masses; two of which were dural-based masses and the other two of which were intraventricular lesions. To our knowledge, manifestation of intracranial RDD as an intraventricular mass has not been reported. As the patient was asymptomatic, no biopsy or surgery of the intracranial lesions was performed.
Most (95%) patients present with cervical lymphadenopathy; inguinal and axillary lymphadenopathy also are common features, present in 44% and 38% of patients, respectively. The extent of lymphadenopathy is often striking, with nodes as large as 6 cm noted, in some cases leading to respiratory compromise (9). Patients might present with nonspecific systemic symptoms, including fever, weight loss, and malaise. Laboratory abnormalities are nonspecific and include anemia, hypergammaglobulinemia, and increased erythrocyte sedimentation rate and white blood cell count. The pathogenesis of this disease is poorly understood, although some have suggested that either infection or immunodeficiency might play a role (9, 10).
Sinus histiocytosis is characterized histologically by nodal sinus dilatation with nonneoplastic proliferation of histiocytes. Avid staining for S-100 protein commonly is seen. The degree of histiocytic proliferation might lead to effacement of normal nodal architecture with nodal capsular fibrosis. These histiocytes typically demonstrate a foamy or vacuolated eosinophilic cytoplasm and characteristically contain small, mature lymphocytes, a condition called lymphocytophagocytosis or emperipolesis. Interestingly, sites of extranodal involvement can demonstrate a histologic pattern resembling nodal involvement (1, 10), with some mimicking of nodal architecture. Typically, however, more fibrosis is evident, and lymphocytophagocytosis may be less often demonstrated.
Although many patients experience spontaneously regressing courses, some, such as our patients, will have disease present in a more extensive form requiring treatment, in some cases to prevent functional loss. Some patients may experience life-threatening complications, such as airway obstruction (11); others may succumb to immunologic disorder and infection. The reported mortality rate is 7%, with many patients who have a fatal outcome having concomitant immune dysfunction. There have been some reports of success in treating Rosai-Dorfman disease with a combination of cytotoxic agents such as alkylating agents, Vinca alkaloids, and prednisone (12). Primary treatment with surgical excision and radiation has been attempted but has not proved to be of consistent value.
Footnotes
Address reprint requests to Yoshimi Anzai, Department of Radiology, University of Michigan Medical Center, 1500 East Medical Center Drive, Ann Arbor, MI 48109-0030.
References
- 1.Rosai J, Dorfman RF. Sinus histiocytosis with massive lymphadenopathy: a newly recognized benign clinicopathological entity. Arch Pathol 1969;87:63-70 [PubMed] [Google Scholar]
- 2.Foucar E, Rosai J, Dorfman R. Sinus histiocytosis with massive lymphadenopathy (Rosai-Dorfman disease): review of the entity. Semin Diagn Pathol 1990;7:19-73 [PubMed] [Google Scholar]
- 3.Mir R, Aftalion B, Kahn LB, et al. Sinus histiocytosis with massive lymphadenopathy and unusual extranodal manifestations. Arch Pathol Lab Med 1985;109:867-870 [PubMed] [Google Scholar]
- 4.Woodcock RJ, Mandell JW, Lipper MH. Sinus histiocytosis (Rosai-Dorfman disease) of the suprasellar region: MR imaging findings: a case report. Radiology 1999;213:808-810 [DOI] [PubMed] [Google Scholar]
- 5.Burton EM, Hickman M, Boulden TF, et al. Orbital sinus histiocytosis: MR appearance. J Comput Assist Tomogr 1989;13:696-699 [DOI] [PubMed] [Google Scholar]
- 6.Udono H, Fukuyama K, Okamoto H, et al. Rosai-Dorfman disease presenting multiple intracranial lesions with unique findings on magnetic resonance imaging: case report. J Neurosurg 1999;91:335-339 [DOI] [PubMed] [Google Scholar]
- 7.Asai A, Matsutani M, Kohno T, et al. Leptomeningeal and orbital benign lymphophagocytic histiocytosis: case report. J Neurosurg 1988;69:610-612 [DOI] [PubMed] [Google Scholar]
- 8.Resnick DK, Johnson BL, Lovely TJ. Rosai-Dorfman disease presenting with multiple orbital and intracranial masses. Acta Neuropathol 1996;91:554-557 [DOI] [PubMed] [Google Scholar]
- 9.Lampert F, Lennert K. Sinus histiocytosis with massive lymphadenopathy: fifteen new cases. Cancer 1976;37:783-789 [DOI] [PubMed] [Google Scholar]
- 10.Rosai J, Dorfman RF. Sinus histiocytosis with massive lymphadenopathy: a pseudolymphomatous benign disorder: analysis of 34 cases. Cancer 1972;30:1174-1188 [DOI] [PubMed] [Google Scholar]
- 11.Stankiewicz JA, Lotan AN, Ratajczak HV. Sinus histiocytosis with massive lymphadenopathy and subglottic stenosis. Ear Nose Throat J 1987;66:440-443 [PubMed] [Google Scholar]
- 12.Komp DM. The treatment of sinus histiocytosis with massive lymphadenopathy (Rosai-Dorfman disease). Semin Diagn Pathol 1990;7:83-86 [PubMed] [Google Scholar]