Spontaneous spinal epidural hematomas are rare clinical conditions that are sometimes difficult to diagnose. The severity of preoperative neurologic deficits and the interval between the onset of symptoms and surgical decompression mainly determine therapeutic outcome. Thanks to recent advances in MR imaging, acute spinal epidural hematomas with minimal neurologic deficits have been reported to be treatable by means of a non-operative approach (1, 2). Although conservative management, based on frequent monitoring of patient neurologic function and repeated MR imaging, is often successful, it can also put such patients at risk of developing spinal cord damage that may not be reversed by an evacuation of the hematoma. The MR imaging characteristics that can accurately predict which patients can successfully undergo conservative treatment are thus important, as mentioned by Fukui et al (1). We recently encountered a case of hyperacute spontaneous spinal epidural hematoma in a 60-year-old woman who suddently developed low back pain without any predisposing illness, followed by weakness in both legs. Within several hours, the weakness in her legs progressed to complete paraplegia. Neurologic examinations revealed flaccid paraparesis and a decreased tactile and pain sensation below the L1 dermatomes, with a preservation of deep sensations. She also presented with urinary retention. Spinal MR imaging performed 5 hours after the onset of symptoms revealed a posterior epidural isointense mass on the T1-weighted images and heterogeneous hyperintensity on the T2-weighted images (Fig 1A) at the T9–L1 levels. The center of the cord showed hyperintensity on T2-weighted images (Fig 1A), indicating secondary ischemic changes. After IV contrast material administration, sizeable dotted enhancement was noted in the lower part of the mass (Fig 1B), thus suggesting the extravasation of contrast-enhanced blood. Surgical intervention revealed a pure epidural hematoma without any causative disease. To investigate the underlying disease entity, such as tumor or vascular anomalies associated with spinal epidural hematomas, contrast-enhanced MR images may be useful. Furthermore, a sizeable enhancement in the hyperacute stage of the hematoma itself might indicate continuing bleeding. Taking the above MR findings into consideration, together with clinical neurologic conditions, it is therefore possible to predict the need for surgical intervention of hyperacute spinal epidural hematomas.
fig 1.
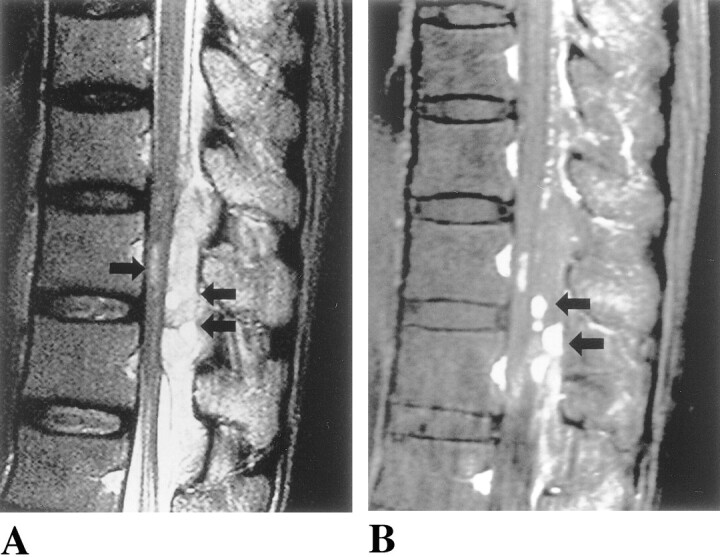
A, Sagittal T2-weighted image, obtained 5 hours after the onset of symptoms, showing an inhomogeneous epidural mass (double arrow) compressing the spinal cord. In the center of the spinal cord, slit-like hyperintensity (arrow) is noted.
B, A sagittal contrast-enhanced T1-weighted image showing a sizeable dotted enhancement (double arrows) in the epidural mass.
Corrections/Clarifications
In the June 2000 issue the name Manzia was misspelled. The correct citation is: Matsubara S, Mandzia JL, ter Brugge K, Willinsky RA, Faughnan ME. Angiographic and clinical characteristics of patients with cerebral arteriovenous malformations associated with hereditary hemorrhagic telangiectasia.AJNR Am Neuroradiol 21:1016–1020.
In the April 2001 issue the name incorrectly appeared as Valérie Ickowitz on the article Prenatal Diagnosis and Postnatal Follow-up of Pericallosal Lipoma: Report of Seven New Cases. The correct name is Valentine Ickowitz.
References
- 1.Fukui MB, Swarnkar AS, Williams RL. Acute spontaneous spinal epidural hematomas. AJNR Am J Neuroradiol 1999;20:1365-1372 [PMC free article] [PubMed] [Google Scholar]
- 2.Holtås S, Heiling M, Lönntoft M. Spontaneous spinal epidural hematoma. Findings at MR imaging and clinical correlation. Radiology 1996;199:409-413 [DOI] [PubMed] [Google Scholar]


