Abstract
Summary: A case of bilateral anomalous origins of the vertebral arteries (VAs) is reported. Both VAs arose directly from the aortic arch between the left common carotid artery and the left subclavian artery. The possible embryologic mechanism and clinical importance of this previously unreported variant are reviewed.
Although the vertebral artery (VA) is classically described as the first branch of the ipsilateral subclavian artery, multiple variations in the origin of that vessel have been reported in the literature. The VA can arise from the aortic arch; from the common, internal, or external carotid arteries; or from subclavian branches, such as the thyrocervical trunk. Also, they may have duplicate origins, generally from the aortic arch and subclavian artery (1). The left VA (LVA) not infrequently arises from the aortic arch, with reported prevalences of 2.4–5.8% (1). When it originates from the arch, the LVA usually enters the transverse foramen of the fourth or fifth cervical vertebra rather than the sixth (2). On the other hand, an aortic origin of the right VA (RVA) is a rare anatomic variant. In such instances, the RVA generally arises distal to the supra-aortic trunks. In a literature review in 1999, Lemke et al (1) found only nine cases in which the RVA originated from the arch. In those cases, the RVA arose between the left common carotid and left subclavian arteries (one case), between the right subclavian and right common carotid arteries in the absence of a formed innominate artery (one case), or distal to the left subclavian artery (seven cases). A bilateral aortic arch origin of the VA represents an exceptional anatomic variant (2).
We present a case of bilateral VA origins from the aortic arch in which both VAs arose proximal to the left subclavian artery. To our knowledge, this anatomic configuration has not been previously reported in the literature. The angiographic findings, possible embryologic mechanism, and clinical implications of this anatomic variant are presented.
Case Report
A 53-year-old man presented with a history of severe headache of acute onset. Brain CT revealed diffuse subarachnoid hemorrhage. Digital subtraction angiography (DSA) was performed by using biplanar angiographic equipment. The right and left common carotid arteries were selectively injected. Because the VAs were not found at their usual location and because they did not become opacified with selective injections in the subclavian arteries, an aortic arch study was performed. The results of this study showed that both VAs arose directly from the aortic arch, between the origins of the left common carotid and left subclavian arteries (Fig 1A and B). The innominate, left common carotid, and left subclavian arteries were otherwise unremarkable. The intracranial study revealed the presence of a distal right anterior cerebral artery aneurysm at the A2-A3 junction (Fig 1C). Because of the presence of large, bilateral, posterior communicating arteries, the anterior circulation studies also resulted in the opacification of the posterior cerebral, distal basilar, and superior cerebellar arteries (Fig 1C).
Fig 1.
DSA images in a 53-year-old man who was examined for a subarachnoid hemorrhage.
A, Aortic arch, left anterior oblique view. On this early arterial-phase image, both carotid axes and both subclavian arteries are well opacified with the contrast agent. The LVA (L) and RVA (R) arise bilaterally from the aortic arch and are opacified, with some delay, when compared with the other supra-aortic trunks. Note that the origin of both VAs is located between the left common carotid and left subclavian arteries (arrows).
B, Aortic arch, left anterior oblique view. This later arterial-phase image shows complete opacification of the VAs and allows better appreciation of their proximal segments.
C, Right internal carotid artery, lateral view. This angiogram shows a small saccular aneurysm located at the A2-A3 junction of the right anterior cerebral artery (arrow). Note the presence of a large right posterior communicating artery and retrograde filling of the distal basilar artery, with opacification of the right superior cerebellar artery (arrowhead). A similar filling pattern was observed on the left side.
Discussion
We describe findings in a patient in whom angiographic investigation for subarachnoid hemorrhage incidentally revealed bilateral VA origins from the aortic arch. Both VAs arose between the left common carotid and left subclavian arteries. The incidence of an aortic arch with five or more primary branches is low. In his comprehensive review in 1916, Poynter (3) recorded only 31 cases of aortic arches with five branches and four with six branches. In seven of these 35 specimens, both VAs arose from the aortic arch. The aortic branching pattern, in a proximal-to-distal progression, was as follows: 1) innominate artery, RVA, left common carotid artery, LVA, and left subclavian artery (four cases) or 2) right subclavian artery, RVA, right common carotid artery, left common carotid artery, LVA, and left subclavian artery (three cases). In 1989, Schwarzacher and Krammer (2) reported an additional case in which the LVA originated between the left common carotid and left subclavian arteries and in which the RVA was the last branch to arise from aortic arch. To our knowledge, no case is reported in the literature in which both VAs originate between the left common carotid and left subclavian arteries.
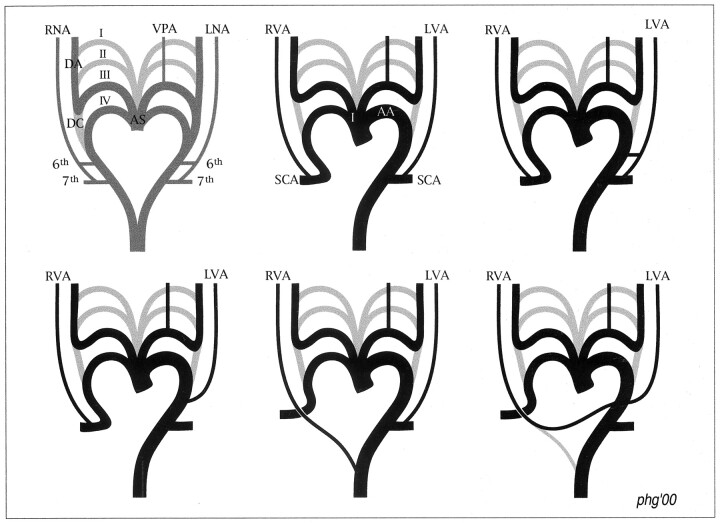
Embryologically, the VA is formed by the development of longitudinal anastomoses that link the cervical intersegmental arteries. The intersegmental arteries eventually regress except for the seventh, which becomes the proximal subclavian artery and which includes the point of origin of the VA in adults (4, 5). Most VA origin variants are easily explained by this embryologic mechanism (Fig 2).
Fig 2.
Schematic representation of the embryologic mechanisms underlying anatomic variants of the VA origin.
Top left, Normal embryologic development. The aortic sac (AS) is connected with the left and right dorsal aortas (DA) via the aortic arches. The first (I), second (II), third (III), and fourth (IV) aortic arches are illustrated. The segment of the DA located between the third and fourth aortic arches is called the ductus caroticus (DC). The left neural axis (LNA) and right neural axis (RNA), which later become the VAs, result from the formation of longitudinal connections linking the intersegmental arteries (only the sixth and seventh intersegmental arteries are depicted here). The ventral pharyngeal artery (VPA) arises from the third aortic arch. It later constitutes the external carotid artery trunk.
Top middle, Normal anatomy in adults. Bilateral regression of the DC separates the common carotid arteries from the subclavian artery on the right side and from the aortic arch on the left side. The LVA and RVA arise from the ipsilateral subclavian arteries (SCA), which are derived from the seventh intersegmental arteries. The AS has evolved into the innominate artery (I) and aortic arch (AA). On each side, the third aortic arch and the distal dorsal aorta constitute the carotid axis, which is divided into the common and internal carotid arteries by the origin of the external carotid artery from the third arch.
Top right, Double origin of the LVA. If both the sixth and seventh intersegmental arteries persist, the LVA has a double origin from the left subclavian artery and aortic arch. A similar mechanism on the right side usually results in a double origin of the RVA from the right subclavian artery.
Bottom left, Aortic origin of the LVA. If the sixth intersegmental artery persists instead of the seventh, the LVA has a single origin from the aortic arch, between the left common and subclavian arteries.
Bottom middle, Aortic origin of the RVA (aberrant RVA). This variant involves the persistence of the proximal right dorsal aorta, which links the RVA to the thoracic aorta distal to the left subclavian artery. If the right fourth aortic arch involutes as well, the right subclavian artery stays connected to the descending thoracic aorta (aberrant right subclavian artery or arteria lusoria).
Bottom right, Bilateral arch origin of the VAs (reported case). The LVA arises from the arch because of the persistence of the sixth intersegmental artery instead of the seventh. The RVA arises from the arch proximal to the left subclavian artery by means of an hypothetic mechanism that involves the initial origin from the descending thoracic aorta distal to the left subclavian artery (as in bottom middle), which is followed by proximal migration of the RVA origin between the left common carotid and subclavian arteries.
For example, the LVA may have a duplicated origin from the arch and the left subclavian artery (combined persistence of the sixth and seventh intersegmental arteries) (Fig 2), or it may arise from only the arch, either proximal or distal to the left subclavian artery (persistence of the sixth or eighth intersegmental arteries, respectively) (Fig 2). An RVA origin distal to the left subclavian artery is compatible with the persistence of the proximal dorsal aorta on the right side and with regression of the segment of right dorsal aorta between the sixth and seventh intersegmental arteries. In such instances, the right subclavian artery may remain connected to the proximal right dorsal aorta, becoming an aberrant subclavian artery (or arteria lusoria). On the other hand, if the right subclavian artery (normally) originates from the seventh intersegmental artery, the RVA is the only branch to stay connected to the persistent proximal dorsal aorta and arise distal to the left subclavian artery (Fig 2). By embryologic analogy and for the sake of simplification, this type of RVA might be referred to as an aberrant RVA. Reported cases of a bilateral aortic origin of the VA are secondary to a combination of these embryologic mechanisms. Understanding the embryologic process that underlies an RVA origin between the left common carotid and subclavian arteries, as in our patient, appears to be more challenging. Wasserman et al (6), reporting about a similar case of an RVA origin in 1992, proposed that the proximal migration of a RVA that initially arises distal to the left subclavian artery produces this variation. If we follow this hypothesis, the aortic branching pattern observed in our patient would result from the combination of a persistent left sixth intersegmental artery and from an aberrant RVA with secondary proximal migration (Fig 2).
Conclusion
To our knowledge, clinical signs or symptoms associated with anomalous VA origins have not been reported yet. Although some have hypothesized that an anomalous origin and the distribution of the large cervical arteries might result in cerebral hemodynamic perturbation with secondary cerebral changes, no conclusive evidence presently suggests that VA origin variants predispose an individual to cerebrovascular disorders (1, 6). Interestingly, our patient had persistent, large, bilateral posterior communicating arteries, which allowed opacification of a substantial portion of the posterior circulation during the carotid angiographic studies. If a large posterior communicating artery not infrequently provides blood flow to the ipsilateral posterior cerebral artery, the observation of distal basilar and superior cerebellar opacification during anterior circulation studies in the absence of severe VA disease is very unusual. Thus, the bilateral aortic origin of the VA appear to represent an unfavorable hemodynamic situation that is responsible for the pattern of flow observed in our case. This anatomic disposition might constitute a risk factor for cerebrovascular pathologic conditions, such as the development of a saccular aneurysm at the origin of a posterior communicating artery, with increased hemodynamic stress or vertebrobasilar insufficiency. In our case, a saccular aneurysm was indeed found during angiography, but its location in the distal anterior cerebral artery makes a causative relation with the VA anatomic variant unlikely. Anomalous VA origins also represent a potential pitfall at diagnostic cerebrovascular imaging. One or both VAs may be wrongly assumed to be occluded or diseased, either by eluding catheterization during angiography or by lying outside the region of interest during noninvasive studies such as CT angiography, MR angiography, or Doppler sonography. Finally, knowledge of potential VA origin variants appears to be mandatory for planning aortic arch surgery or endovascular interventions.
References
- 1.Lemke AJ, Benndorf G, Liebig T, Felix R. Anomalous origin of the right vertebral artery: review of the literature and case report of the right vertebral artery origin distal to the left subclavian artery. AJNR Am J Neuroradiol 1999;20:1318–1321 [PMC free article] [PubMed] [Google Scholar]
- 2.Schwarzacher SW, Krammer EB. Complex anomalies of the human aortic arch system: unique case with both vertebral arteries as additional branches of the aortic arch. Anat Rec 1989;225:246–250 [DOI] [PubMed] [Google Scholar]
- 3.Poynter CWM. Arterial anomalies pertaining to the aortic arches and the branches arising from them. Nebr Univ Stud 1916;16:229–345 [Google Scholar]
- 4.Newton TH, Mani RL. The vertebral artery. In: Newton TH, Potts DG, eds. Radiology of skull and Brain. St. Louis, Mo: Mosby;1974;1659–1672
- 5.Moore KL. The Developing Human. 3rd ed. Philadelphia, Pa: Saunders; 1982
- 6.Wasserman BA, Mikulis DJ, Manzione JV. Origin of the right vertebral artery from the left side of the aortic arch proximal to the origin of the left subclavian artery. AJNR Am J Neuroradiol 1992;13:355–358 [PMC free article] [PubMed] [Google Scholar]