Abstract
Summary: In this report, we describe the appearance of the spinal vertebral body and epidural abscesses in a patient who underwent diffusion-weighted imaging of the spine and CT-guided aspiration of one of the abscesses. The abscesses were hyperintense relative to the surrounding tissues on diffusion-weighted images, and they appeared dark on apparent diffusion coefficient maps; these findings were consistent with those of published reports of the brain and liver.
Diffusion-weighted MR imaging is well established as an important clinical tool for the study of a number of brain disorders. Diffusion-weighted images can be used to rapidly and accurately assess the extent of cerebral ischemia in patients with acute stroke (1) and also to accurately distinguish brain abscesses from cystic neoplasms, a distinction not always possible by using conventional images alone (2–5). Until recently, only a few published reports (6–8) have described the use of diffusion-weighted imaging to evaluate disease processes of the spine. Recent technical advances have made diffusion-weighted imaging of the spine substantially more practical for routine clinical use (9, 10). As experience with diffusion-weighted imaging in the spine increases, new information about the appearance of common spinal abnormalities is expected to be helpful to physicians who interpret MR images of the spine. We report the findings in a patient with osseous and epidural abscesses who underwent both diffusion-weighted imaging and percutaneous aspiration of one of the abscesses, with subsequent histologic analysis. This report provides information about the appearance of spinal abscesses on diffusion-weighted images compared with that of conventional MR images in the same patient.
Case Report
An 83-year-old-man who had been undergoing IV vancomycin therapy for recurrent methicillin-resistant Staphylococcus aureus bacteremia and osteomyelitis involving the L1 vertebral body was examined for increasing back pain. Lumbar MR imaging examination included T1-weighted, T2-weighted, and contrast material–enhanced T1-weighted imaging (Fig 1A–C) with a 1.5-T clinical MR unit. Additionally, sagittal diffusion-weighted images were obtained by using a spin-echo echo-planar technique (b values, 0 and 500 s/mm2; TR/TE (effective)/excitations, 1215/80/2; 30-cm field of view; 256 × 256 matrix) (Fig 1D and E). The sequence provided equal diffusion weighting in three mutually orthogonal directions (superior-inferior, anterior-posterior, and left-right) and thus produced trace-weighted diffusion-weighted images. Navigator echo motion correction was used to correct for phase errors due to motion on the diffusion-weighted images. Isotropic (ie, trace-weighted) maps of the apparent diffusion coefficient (ADC) were generated by using software available on the MR unit (Fig 1F). Region-of-interest analysis of ADC values was not performed.
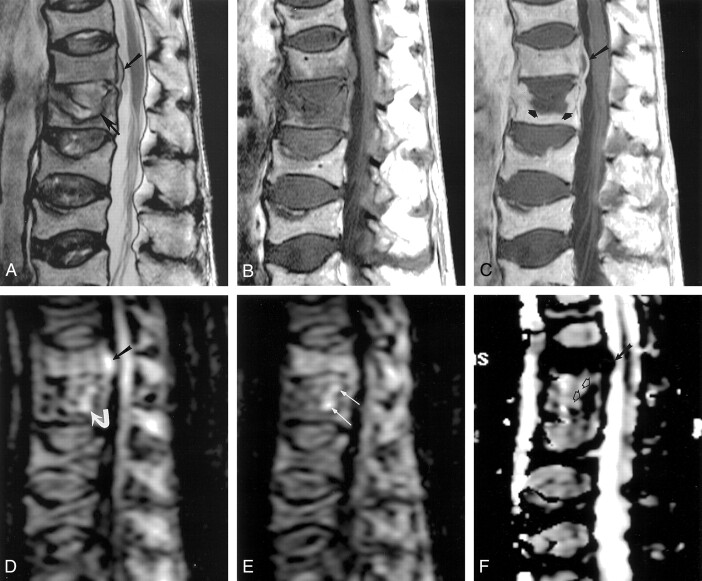
Fig 1.
Images obtained in an 83-year-old man with bacteremia and back pain.
A, T2-weighted sagittal MR image (3000/103) shows a small ventral extradural mass (upper arrow) and a fracture and abnormal signal intensity adjacent to the superior endplate of the L1 vertebral body (lower arrow).
B and C, T1-weighted sagittal MR images (815/30) obtained before (B) and after (C) IV administration of gadolinium-based contrast material show central nonenhancement in the extradural mass (long arrow in C) and in a substantial portion of the superior portion of the L1 vertebral body (short arrows in C). Both areas of nonenhancement were interpreted as abscesses.
D, Sagittal diffusion-weighted MR image (1215/80/2, b = 500) obtained at the same location as in A–C shows very high signal intensity within the extradural abscess (straight arrow) and high signal intensity within the region of the vertebral abscess (curved arrow).
E, Sagittal diffusion-weighted MR image (1215/80/2) obtained immediately to the left of D shows high signal intensity in the vertebral abscess (arrows).
F, ADC map obtained at same location as in D shows the dark appearance of both epidural (solid arrow) and vertebral abscess (open arrows) regions.
Because of the patient’s worsening symptoms and because of new MR findings consistent with epidural and vertebral body abscesses, CT-guided biopsy of the vertebral body thought to contain an abscess (L1) was performed to obtain material for microbial culturing and sensitivity analysis. Antibiotic therapy was discontinued during the 2 days before biopsy to increase the likelihood of positive findings with the microbial culture. The location that was sampled corresponded to the region thought to contain the vertebral body abscess within the superior portion of the L1 vertebral body (Fig 2). At this location, turbid liquid material was aspirated from the bone.
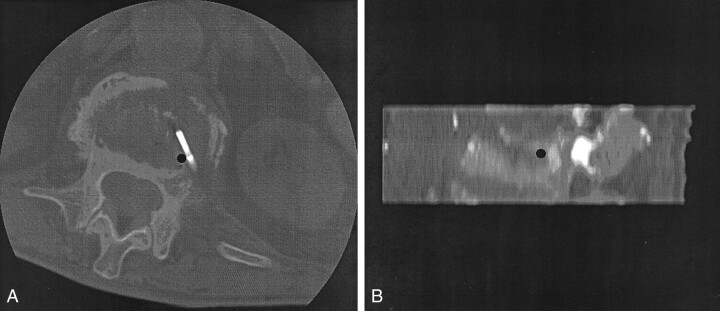
Fig 2.
Images obtained during biopsy of the vertebral body thought to contain an abscess.
A, Transverse CT image obtained at the level of L1 during needle placement for biopsy shows the position of the biopsy needle with the inner stylet at the final position prior to the aspiration of fluid from the bone. The black dot marks the location of the tip of the needle after removal of the inner stylet.
B, Sagittal reformatted image that was constructed from the prebiopsy CT scan. The black dot shows the position of the needle tip shown in A.
Cytologic examination of the aspirated material revealed increased numbers of polymorphonuclear leukocytes; this finding was consistent with acute infection (Fig 3). Antibiotic therapy was restarted and continued without further worsening of symptoms. Cultures of the material obtained at both locations showed no organismal growth after 7 days.
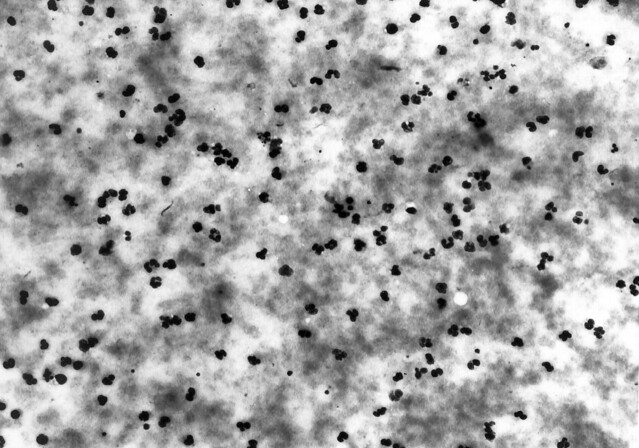
Fig 3.
Photomicrograph shows debris and multiple polymorphonuclear leukocytes. The findings were interpreted as being consistent with acute infection (hematoxylin-eosin, original magnification ×800).
Discussion
MR imaging is frequently ordered to determine the presence and extent of spinal infection. Diffusion-weighted imaging is a well-established method for studying cerebral disease processes, but the previous use of diffusion-weighted imaging in the spine has been limited for technical reasons. Recent advances in techniques designed to decrease motion-related artifacts have made spinal diffusion-weighted imaging more practical for routine use (7, 9, 10). Therefore, knowledge of the diffusion-weighted imaging appearance of common disease entities that affect the spine is valuable.
Spinal infections such as discitis and osteomyelitis are commonly seen in clinical practice. Spinal abscesses in the epidural space, paraspinal space, and bone are important complications of spinal infection. Abscesses in the epidural space frequently are surgical emergencies, because the mass effect from the abscesses and adjacent phlegmonous tissues can result in spinal cord compression and permanent neurologic deficit if it is not treated rapidly. Abscesses in the bony structures of the spine can result in bone weakening and spinal instability. Thus, techniques that could help in the accurate and early detection of spinal abscesses are valuable. The present report shows how diffusion-weighted images could help to increase the conspicuity of spinal abscesses.
Our finding that both the osseous abscess and the epidural abscess were markedly hyperintense relative to the surrounding tissues on diffusion-weighted images agrees with those of previously published reports that describe a similar appearance in abscess cavities in the brain and liver (2, 3, 11). Additionally, the present finding that the abscesses were dark on the ADC maps also agrees with those of published articles that have described low ADC values within abscesses (2, 11).
We could not obtain accurate absolute ADC values in the present case for two reasons. First, we assumed that the small abscess cavities in the present case would result in errors due to volume-averaging artifacts. Second, a routine algorithm designed to increase homogeneity of signal intensity across the images was active during image acquisition. This algorithm typically improves the quality of spinal images, but such automated processing is expected to decrease the accuracy of quantitative analysis. Therefore, we believe that we cannot properly compare our ADC values with those of previous studies of brain and liver abscesses. In the future, we hope to be able to study absolute ADC values in cases of spinal infection that are evaluated with diffusion-weighted imaging.
Our finding that the vertebral body abscess appeared to be more conspicuous on the diffusion-weighted images than on conventional images (eg, contrast-enhanced T1-weighted images) is notable. One likely reason is that the location of the vertebral body abscess along the T12-L1 intervertebral disk margin may have decreased its conspicuity on the conventional images. Another reason may be that the vertebral body abscess was located within a deformed vertebra that was shortened because of a prior compression fracture. These factors may have decreased accuracy in the visual assessment of the expected contour along the superior margin of the vertebral body. By comparison, the markedly hyperintense signal of the vertebral body abscess on the diffusion-weighted images increased its conspicuity.
References
- 1.Warach S, Chien D, Li W, Ronthal M, Edelman RR. Fast magnetic resonance diffusion-weighted imaging of acute human stroke. Neurology 1992;42:1717–1723 [DOI] [PubMed] [Google Scholar]
- 2.Ebisu T, Tanaka C, Umeda M, et al. Discrimination of brain abscess from necrotic or cystic tumors by diffusion-weighted echo planar imaging. Magn Reson Imaging 1996;9:1113–1116 [DOI] [PubMed] [Google Scholar]
- 3.Kim YJ, Chang KH, Song IC, et al. Brain abscess and necrotic or cystic brain tumor: discrimination with signal intensity on diffusion-weighted MR imaging. AJR Am J Roentgenol 1998;171:1487–1490 [DOI] [PubMed] [Google Scholar]
- 4.Desprechins B, Stadnik T, Koerts G, Shabana W, Breucq C, Osteaux M. Use of diffusion-weighted MR imaging in differential diagnosis between intracerebral necrotic tumors and cerebral abscesses. AJNR Am J Neuroradiol 1999;20:1252–1257 [PMC free article] [PubMed] [Google Scholar]
- 5.Noguchi K, Watanabe N, Nagayoshi T, et al. Role of diffusion-weighted echo-planar MRI in distinguishing between brain abscess and tumor: a preliminary report. Neuroradiology 1999;41:171–174 [DOI] [PubMed] [Google Scholar]
- 6.Spuentrup E, Buecker A, Adam G, van Vaals JJ, Guenther RW. Diffusion-weighted MR imaging for differentiation of benign fracture edema and tumor infiltration of the vertebral body. AJR Am J Roentgenol 2001;176:351–358 [DOI] [PubMed] [Google Scholar]
- 7.Baur A, Huber A, Ertl-Wagner B, et al. Diagnostic value of increased diffusion weighting of steady-state free precession sequence for differentiating acute benign osteoporotic fractures from pathologic vertebral compression fractures. AJNR Am J Neuroradiol 2001;22:366–372 [PMC free article] [PubMed] [Google Scholar]
- 8.Baur A, Stabler A, Bruning R, et al. Diffusion-weighted MR imaging of bone marrow: differentiation of benign versus pathologic vertebral compression fractures. Radiology 1998;207:349–356 [DOI] [PubMed] [Google Scholar]
- 9.Holder CA, Muthupillai R, Mukundun S, Eastwood JD, Hudgins PA. Diffusion-weighted MR imaging of the normal human spinal cord in-vivo. AJNR Am J Neuroradiol 2000;21:1799–1806 [PMC free article] [PubMed] [Google Scholar]
- 10.Clark CA, Barker GJ, Tofts PS. Magnetic resonance diffusion imaging of the human cervical spinal cord in vivo. Magn Reson Med 1999;41:1269–1273 [DOI] [PubMed] [Google Scholar]
- 11.Chan JH, Tsui EY, Luk SH, et al. Diffusion-weighted MR imaging of the liver: distinguishing hepatic abscess from cystic or necrotic tumor. Abdom Imaging 2001;26:161–165 [DOI] [PubMed] [Google Scholar]