Abstract
Summary: We describe the clinical, MR imaging, and pathologic findings in two cases of primary sellar lymphoma in immunocompetent individuals. Both patients had hypopituitarism, and one patient had a sixth cranial nerve palsy. MR images depicted sellar and suprasellar masses in both patients, and extension into the cavernous and sphenoid sinuses was also present in one patient. The pathologic diagnosis in both cases was large B cell lymphoma.
The incidence of primary CNS lymphoma has been dramatically increasing in both immunocompromised and immunocompetent patients (1). However, primary pituitary lymphoma remains exceedingly rare. We describe two cases of primary sellar lymphoma in immunocompetent individuals.
Case Reports
Case 1
A 74-year-old man had a history of mild dementia, chronic obstructive pulmonary disease, and chronic constipation; a 3-wk history of seizurelike activity, mental status changes, progressive weakness, dizziness and falling; and a 28-lb weight loss over several months. Questioning revealed that he had increased thirst, cold intolerance, worsening constipation, and impotence for 1 y. Physical examination revealed axillary and groin hair loss, hypogonadism, orthostatic hypotension, and a possible mild bitemporal visual field deficit.
The patient was admitted for presumed hypopituitarism, which was confirmed with the following abnormally low laboratory findings: plasma cortisol level (0.6 μg/dL; normal, 5–18 μg/dL), total testosterone level (5.0 ng/dL; normal, 270–1070 ng/dL), free testosterone level (<0.7 pg/dL; normal, 9–26 pg/dL), follicle stimulating hormone level (1.3 IU/L; normal, 4–20 IU/L), luteinizing hormone level (0.1 IU/L; normal, 3–12 IU/L), thyroid stimulating hormone level (<0.16 μU/mL; normal, 0.4–6.2 μU/mL), and triiodothyronine resin uptake (24%; normal, 25–35%). The patient did not have hypernatremia or other signs of diabetes insipidus.
MR images of the brain revealed a 1–2-cm-diameter well-circumscribed dumbbell-shaped sellar and suprasellar mass extending through the diaphragma sellae. The mass involved the pituitary gland and infundibular stalk and abutted the optic chiasm. Erosion of the left sellar floor was present. The mass was isointense relative to gray matter on T1- and T2-weighted images and showed inhomogeneous contrast enhancement (Fig 1). No other brain lesions were seen. A presumptive diagnosis of pituitary adenoma was made.
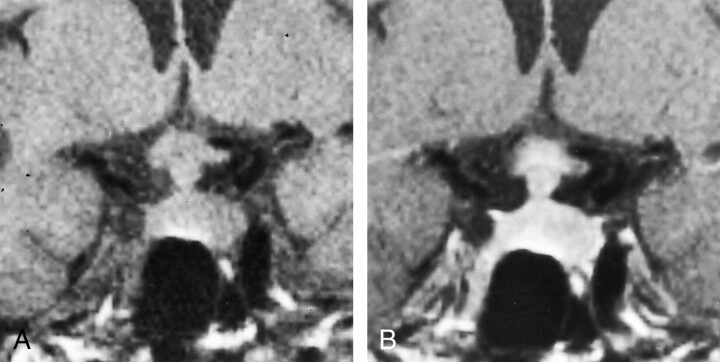
Fig 1.
Case 1. Coronal T1-weighted (TR/TE, 500/20) MR images of the sellar region depict a large, heterogeneously enhancing sellar mass.
A, Nonenhanced image.
B, Gadolinium-enhanced image.
The patient underwent transsphenoidal piecemeal resection of the pituitary mass. The mass was a firm gray lesion that filled the sella turcica, eroded the central sellar floor, and extended to the suprasellar region. The mass extensively infiltrated the anterior pituitary and contained areas of necrosis and dense desmoplastic reaction. It did not extend into the dura mater. At light microscopy, the mass contained loosely cohesive cells with numerous mitotic figures (Fig 2A). The tumoral cells were immunoreactive for leukocyte common antigen (LCA) CD45 (Fig 2B) and for the B-cell markers L26 (CD20) and 4KB5. Results with T-cell markers CD3p and CD43 were negative in the tumor cells. These pathologic findings were consistent with those of a large B-cell lymphoma.
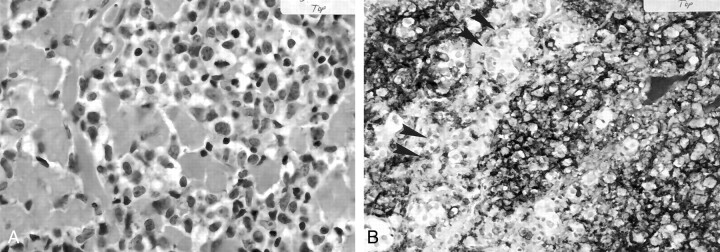
Fig 2.
Case 1. Photomicrographs.
A, Large cells with nuclei display prominent nucleoli that diffusely infiltrate the pituitary gland (hematoxylin-eosin, original magnification ×200).
B, The lymphoma cells are reactive for LCA and stain darkly, in contrast with the normal entrapped pituitary cells (arrowheads) (CD45 immunohistochemical stain, original magnification ×100).
After surgery, diabetes insipidus developed. Findings at staging CT of the chest, abdomen, and pelvis and at bone marrow biopsy were negative. Results of enzyme-linked immunosorbent assay and p24 testing for human immunodeficiency virus (HIV) were negative. The patient was discharged with a diagnosis of primary CNS lymphoma and was treated with pituitary hormone replacement therapy and desmopressin, or DDAVP. He was also given a 6-wk 4600-cGy course of conventional radiation therapy to the pituitary, but he died soon thereafter.
Case 2
A 65-year-old man with a history of smoking presented with diplopia, severe right retrobulbar pain, and a 1-y history of decreased energy and libido. Physical examination revealed a right-sided sixth cranial nerve palsy. Laboratory findings revealed partial hypopituitarism, with low levels of follicle stimulating hormone (2.5 IU/L; normal, 4–20 IU/L) and luteinizing hormone (2.5 IU/L; normal. 3–12 IU/L). Hypothyroidism, hypocortisolism, and low testosterone levels had been diagnosed at the referring institution and treated. The serum prolactin level was normal (9.8 ng/mL; normal, <18.5 ng/mL). The patient did not have hypernatremia or other signs of diabetes insipidus.
Brain MR imaging revealed a 2-cm-diameter dumbbell-shaped sellar and suprasellar mass extending through the diaphragma sellae and abutting and slightly compressing the optic chiasm. The mass also extended into the right cavernous sinus surrounding the right internal carotid artery and eroded into the sphenoid sinus on the right (Fig 3). The mass was isointense relative to gray matter on T1-weighted images and hypointense on T2-weighted images; it showed marked inhomogeneous contrast enhancement. A presumptive diagnosis of pituitary adenoma was made.
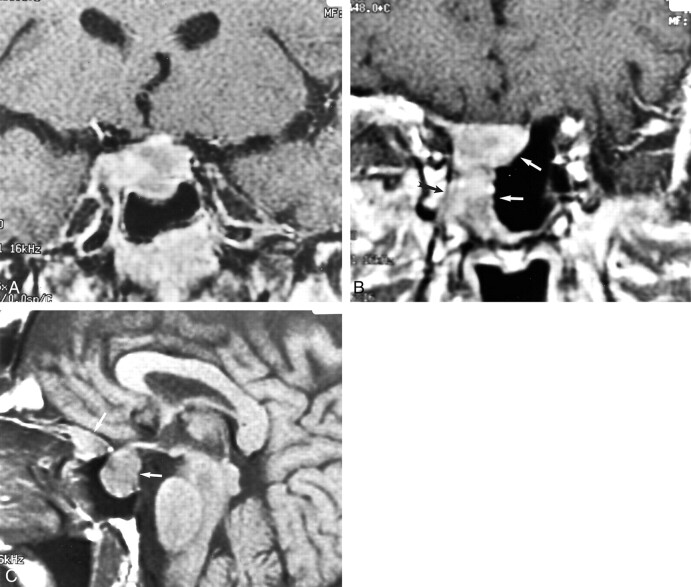
Fig 3.
Case 2. T1-weighted MR images of the sellar region.
A, Coronal image (600/15) depicts a heterogeneously enhancing sellar mass.
B, More anterior coronal section (600/15) depicts invasion of the right sphenoid sinus (white arrows) and cavernous sinus (black arrow).
C, Sagittal gadolinium-enhanced image (500/16) depicts two large portions of the sellar and parasellar mass (arrows).
The patient underwent a difficult transsphenoidal piecemeal resection of the pituitary mass. The mass filled the sella turcica and was large, pink, and fleshy. It eroded through the floor of the sella turcica into the sphenoid sinus and extended into suprasellar and parasellar regions. Invasion of the dura mater was present. Cytologically, the mass contained a monomorphic proliferation of intermediate-to-large lymphoid cells characterized by scant eosinophilic cytoplasm, frequent nuclear membrane irregularities, one to several nucleoli, and a high level of mitotic activity (Fig 4A). Necrosis was not a prominent feature. Immunohistochemical staining revealed expression of LCA (CD45) and the B-cell markers L26 (CD20) (Fig 4B) and 4KB5 by the cells of the mass. These findings were consistent with those of a high-grade, large B cell lymphoma
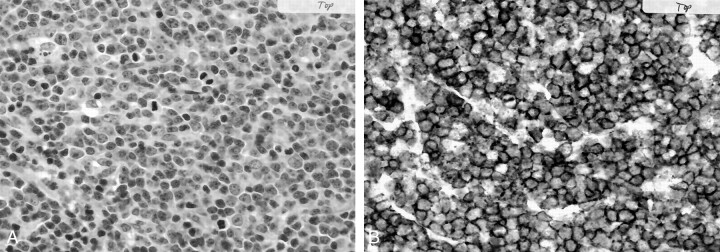
Fig 4.
Case 2. Photomicrographs.
A, Highly anaplastic malignant lymphoma with numerous mitotic figures (hematoxylin-eosin, original magnification ×200).
B, Tumor cells express the B-cell marker L26 (CD20) and show dark membrane staining (CD45 immunohistochemical stain, original magnification ×100).
No surgical complications occurred. Findings at staging CT of the chest, abdomen, and pelvis and at bone marrow biopsy were negative. The patient did not have known HIV infection or immunosuppression. The patient was discharged with a diagnosis of primary CNS lymphoma and further treated with pituitary hormone replacement, stereotactic radiosurgery, and four cycles of Codox-M chemotherapy. He was considered to be in remission until 14 mo after surgery, when he presented with urinary obstruction secondary to lymphadenopathy in the abdomen. The patient then received four cycles of reinduction chemotherapy with etoposide, vincristine, and doxorubicin with cyclophosphamide, or EPOCH, and underwent bone marrow transplantation. He died of pulmonary failure 2 y after surgery.
Discussion
We have described the clinical, MR imaging, and pathologic findings in two cases of primary sellar lymphoma, an exceedingly rare entity, in immunocompetent individuals. Neither patient had systemic lymphoma or other brain lesions. A preoperative presumptive diagnosis of pituitary adenoma had been made in both cases, on the basis of the patient’s presentation and imaging findings. However, pathologic evaluation of the surgical specimens in both cases revealed that the masses represented B-cell lymphoma of the pituitary.
Primary CNS lymphoma is an uncommon neoplasm, historically representing approximately 1% of primary brain tumors (1). However, its incidence has more than tripled in the United States and United Kingdom since the early 1980s (1). Primary CNS lymphoma represents approximately 3% of intracranial neoplasms in patients with acquired immunodeficiency syndromes, but the incidence in immunocompetent patients has been increasing, for uncertain reasons (1, 2). The vast majority of CNS lymphomas are non-Hodgkin B-cell lymphomas (3), as in the two present cases.
Reports of primary pituitary lymphoma have been exceedingly rare (4–12). Primary CNS lymphoma most commonly arises from the deep hemispheric periventricular white matter; other expected sites include the corpus callosum, cerebellum, orbits, and cranial nerves (13). The typical MR findings in primary CNS lymphoma are mass lesions that are iso- to hypointense on T1- and T2-weighted images (3, 13), as in the two present cases. The absence of T2 prolongation results from the dense cellularity and high nucleus-to-cytoplasm ratio of lymphoma (13), and it may help in the differentiation of primary CNS lymphoma from other brain tumors (3). Typically, contrast enhancement is intense and homogeneous in immunocompetent patients, but it is more likely to be inhomogeneous or ringlike in immunocompromised patients (3, 13). Nonetheless, contrast enhancement was inhomogeneous in the two present cases of primary pituitary lymphoma. Also, multiple lesions are frequently seen on MR images in both individuals with intact immune systems and those with compromised systems, but they may be more common in immunocompromised patients (3, 13).
The mean age of immunocompetent patients with primary CNS lymphoma has been reported to be 60–70 y, compared with a mean age of 30–40 y in immunocompromised individuals (3). A male predominance has also been reported (3). The demographic characteristics of the two present patients are consistent with these observations. Of the reported cases of primary sellar lymphoma, the majority involved headache, cranial nerve abnormalities, and evidence of pituitary insufficiency (12). Indeed, the two present cases had hypopituitarism at clinical presentation, and one had a cranial nerve palsy as well. Primary CNS lymphoma in other locations has a different presentation, unless extension of the tumor involves the hypothalamus, infundibular stalk, or pituitary.
Pituitary adenoma is, by far, the most common sellar mass, although craniopharyngioma, Rathke cleft cyst, dermoid, epidermoid, germinoma, metastasis, meningioma, arachnoid cyst, sarcoidosis, tuberculosis, histiocytosis, lymphocytic hypophysitis, schwannoma, infundibular glioma, and cavernous carotid artery aneurysm are included in the differential diagnosis of sellar and parasellar disease (12, 14). Although primary pituitary lymphoma may be indistinguishable from pituitary adenoma at imaging, one should consider lymphoma when evaluating an invasive sellar mass that is iso- to hypointense on T2-weighted MR images, particularly when the patient is immunocompromised or old.
Acknowledgments
We sincerely thank Robb Hoehlein, MD, University of Virginia, for valuable assistance in manuscript preparation.
References
- 1.Jellinger KA, Paulus W. Primary central nervous system lymphomas: an update. J Cancer Res Clin Oncol 1992;199:7–27 [DOI] [PubMed] [Google Scholar]
- 2.Maher EA, Fine HA. Primary CNS lymphoma. Semin Oncol 1999;26:346–356 [PubMed] [Google Scholar]
- 3.Johnson BA, Fram EK, Johnson PC, Jacobowitz R. The variable MR appearance of primary lymphoma of the central nervous system: comparison with histopathologic features. AJNR Am J Neuroradiol 1997;18:563–572 [PMC free article] [PubMed] [Google Scholar]
- 4.Singh VP, Mahapatra AK, Dinde AK. Sellar-suprasellar primary malignant lymphoma: case report. Indian J Cancer 1993;30:88–91 [PubMed] [Google Scholar]
- 5.Gottfredsson M, Oury TD, Bernstein C, Carpenter C, Bartlett JA. Lymphoma of the pituitary gland: an unusual presentation of central nervous system lymphoma in AIDS. Am J Med 1996;5:563–564 [DOI] [PubMed] [Google Scholar]
- 6.Shaw JAM, Sawers HA, Strachan FM, Bevan JS. Non-Hodgkin lymphoma with panhypopituitarism, hyperprolactinaemia and sixth nerve palsy. J R Soc Med 1997;90:274–275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Freda PU, Post KD. Differential diagnosis of sellar masses. Endocrinol Metab Clin North Am 1999;28:81–117 [DOI] [PubMed] [Google Scholar]
- 8.Kuhn D, Buchfelder M, Brabletz T, Paulus W. Intrasellar malignant lymphoma developing within pituitary adenoma. Acta Neuropathol 1999;97:311–316 [DOI] [PubMed] [Google Scholar]
- 9.Au WY, Kwong YL, Shek TW, Leung G, Ooi C. Diffuse large-cell B-cell lymphoma in a pituitary adenoma: an unusual cause of pituitary apoplexy. Am J Hematol 2000;63:231–232 [DOI] [PubMed] [Google Scholar]
- 10.Mathiasen RA, Jarrahy R, Cha ST, et al. Pituitary lymphoma: a case report and literature review. Pituitary 2000;2:283–287 [DOI] [PubMed] [Google Scholar]
- 11.Singh S, Cherian RS, George B, Nair S, Srivastava A. Unusual extra-axial central nervous system involvement of non-Hodgkin’s lymphoma: magnetic resonance imaging. Australas Radiol 2000;44:112–114 [DOI] [PubMed] [Google Scholar]
- 12.Landman RE, Wardlaw SL, McConnell RJ, Khandji AG, Bruce JN, and Freda PU. Pituitary lymphoma presenting as fever of unknown origin. J Clin Endocrinol Metab 2001;86:1470–1476 [DOI] [PubMed] [Google Scholar]
- 13.Erdag N, Bhorade RM, Alberico RA, Yousuf N, Patel M. Primary lymphoma of the central nervous system: typical and atypical CT and MR imaging appearances. AJR Am J Roentgenol 2001;176:1319–1326 [DOI] [PubMed] [Google Scholar]
- 14.FitzPatrick M, Tartaglino LM, Hollander MD, Zimmerman RA, Flanders AE. Imaging of sellar and parasellar pathology. Radiol Clin North Am 1999;37:101–121 [DOI] [PubMed] [Google Scholar]