Abstract
Summary: MR digital subtraction angiography (DSA) is a new diagnostic tool capable of producing dynamic images of the cerebral circulation with the injection of gadopentetate dimeglumine into a peripheral vein. Previous reports have concentrated on its potential as a noninvasive technique for the study of pial arteriovenous malformations. In this report, we present our early findings with MR DSA in the evaluation of intracranial dural arteriovenous fistulae.
MR digital subtraction angiography (DSA) is a noninvasive technique that allows dynamic assessment of the cranial circulation. To our knowledge, we present the first report of its use in the detection and classification of dural arteriovenous fistulae (DAVF).
Case Reports
Case 1
A 73-year-old man with ischemic heart disease was admitted with visual deterioration. He described daily headaches for the previous 9 months and pulsatile tinnitus. On examination, he was found to have papilledema and an opening pressure in excess of 40 cm of water at lumbar puncture. Contrast material–enhanced CT and T1-weighted MR images were normal. The T2-weighted image was normal except for loss of the normal flow void at the right jugular bulb. Time-of-flight (TOF) venography demonstrated reduced, heterogeneous, irregular signal intensity within the right lateral sinus (Fig 1A), but after the injection of gadolinium-based contrast material, the lateral sinuses showed symmetric signal intensity. The vascularity of the external carotid circulation was clearly increased.
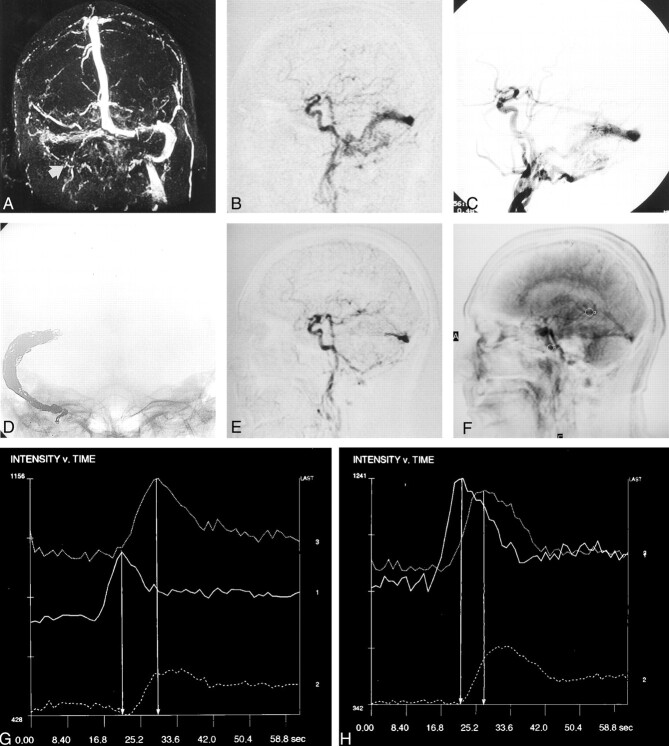
Fig 1.
Case 1. A 73-year-old man with ischemic heart disease, visual deterioration, and pulsatile tinnitus.
A, Nonenhanced TOF MR venogram demonstrates reduced signal intensity within the right lateral sinus and occlusion of the right jugular bulb (arrow).
B, Single-frame MR-DSA image from the early arterial phase of the lateral acquisition demonstrates synchronous opacification of the intracranial ICA and right lateral sinus by an extensive DAVF.
C, Catheter angiogram confirms the diagnosis of a type IIa DAVF.
D, Most of the right lateral sinus has been packed with platinum coils.
E, Postembolization MR-DSA image (acquired as in B) reveals a modest residual shunt via branches of the occipital and posterior meningeal arteries.
F, Lateral MR-DSA frame demonstrates the regions of interest for measures of signal intensity: 1 indicates the ICA; 2, SSS; and 3, voG.
G and H, Preembolization (G) and postembolization (H) signal intensity–time plots. Plots in H demonstrate earlier (by 3 seconds) peak filling of the voG. 1 indicates the ICA; 2, SSS; and 3, voG. Vertical lines mark the peak intensities of the ICA and voG.
Dynamic MR DSA revealed synchronous filling of the intracranial carotid artery and the right lateral sinus due to the presence of a DAVF (Fig 1B). Occlusion of the right jugular bulb resulted in retrograde filling of the left lateral sinus without reflux into the cortical veins. Catheter angiographic findings confirmed the diagnosis of a Djindjian type IIa DAVF (Fig 1C). The right lateral sinus was subsequently packed with mechanical detachable coils in an attempt to alleviate the intracranial hypertension (Fig 1D).
Three months after treatment, the patient was asymptomatic and reported improved exercise tolerance. Repeat MR DSA revealed near total occlusion of the fistula with only a small arteriovenous shunt at the torcula (Fig 1E). Signal intensity was plotted against time by using the petrous segment of the internal carotid artery (ICA), superior sagittal sinus (SSS), and vein of Galen (voG) as regions of interest (Fig 1F). Measurements of the temporal separation of time-to-peak values for the ICA and voG/SSS were then obtained. These values had an estimated precision of ±0.5 seconds. After embolization, venous opacification occurred 3 seconds earlier than on the pretreatment image (Fig 1G and H). The difference between the peak opacification of the ICA and voG was 5 seconds, which was similar to that of an age-matched subject with pulsatile tinnitus but no DAVF.
Case 2
A 51-year-old woman had bilateral tinnitus for 6 weeks and an audible bruit over the left mastoid bone. T2-weighted MR images demonstrated uniform high signal intensity within the left sigmoid sinus and jugular bulb. This area of signal change was isointense compared with muscle on T1-weighted images and enhanced avidly with gadolinium-based contrast material. The jugular bulb was distended, and a diagnosis of acute sinus thrombosis was made (Fig 2A). Catheter angiography demonstrated occlusion of the sigmoid sinus and a type IIa DAVF in the transverse sinus. Venous drainage was retrograde, without reflux into the cortical veins. Treatment was not offered at this time because the patient’s symptoms were not severe, and the sinus was required for drainage of a large vein of Labbé.
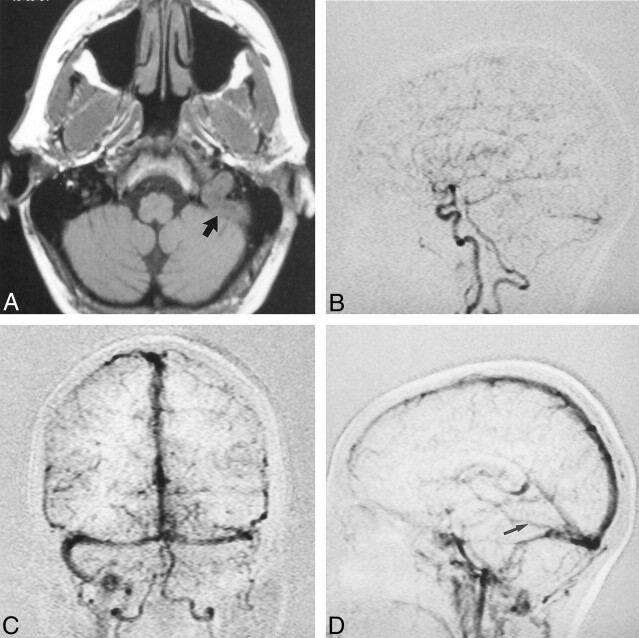
Fig 2.
Case 2. A 51-year-old woman had bilateral tinnitus and an audible bruit over the left mastoid bone.
A, Axial nonenhanced T1-weighted MR image demonstrates marked distension of the left jugular bulb and sigmoid sinus caused by a thrombus (arrow).
B, Single MR-DSA frame from the early arterial phase of the lateral acquisition demonstrates synchronous opacification of the intracranial ICA and left transverse sinus caused by a DAVF fed primarily by branches of the left occipital and posterior auricular arteries.
C, Single MR-DSA frame from the midvenous phase of the frontal acquisition demonstrates enlarged arterial pedicles, occlusion of the left sigmoid sinus, and retrograde venous drainage into the right lateral sinus. Filling of the SSS is not delayed.
D, Single MR-DSA frame from the venous phase of the lateral acquisition demonstrates a large vein of Labbé (arrow) entering the left transverse sinus distal to the DAVF.
Repeat MR imaging was performed after 2 years, following a change in the character of the tinnitus. The study revealed persistent signal change within the sigmoid sinus, and arterial flow voids were identified within the wall of the sinus. MR DSA demonstrated the DAVF, which received its supply predominantly from the occipital artery (Fig 2B), and confirmed patency of the venous outflow through the contralateral jugular bulb (Fig 2C). The ipsilateral sinus remained occluded. The dominant ipsilateral vein of Labbé was easily visualized, and its presence contraindicated venous sacrifice (Fig 2D). Opacification of the SSS and voG was not delayed.
Case 3
A 69-year-old woman had progressive pulsatile tinnitus for 6 months and headache. On examination, an audible bruit was present over the right mastoid bone, but no papilledema or loss of visual acuity was noted. T2-weighted MR images demonstrated normal flow voids within the dural sinuses, and no definite signal change or flow voids related to walls of the sinus were seen. A TOF MR venogram obtained after the injection of contrast material revealed enlarged branches of the external carotid circulation abutting the right lateral sinus. On MR-DSA images, contrast enhancement appeared simultaneously in the ICA and right lateral sinus via a DAVF, and prompt filling of the contralateral sinus occurred. Subsequent frames showed initial clearing of the right lateral sinus before it became opacified once again by venous drainage from the normal brain. Catheter angiographic findings confirmed the presence of a DAVF in the lateral sinus, with both antegrade and retrograde filling of the venous sinuses but no outflow obstruction. Because the patient had no signs or symptoms of intracranial hypertension and because the lateral sinus was functional, venous occlusion was not offered. Despite fairly severe tinnitus, the patient declined embolization of the occipital artery as a palliative procedure.
Discussion
Symptoms and complications of DAVF result from arterialization of the venous system, and they can be predicted from the pattern of venous drainage. Lesions that involve the dural sinuses often present with a bruit, tinnitus, or intracranial hypertension, while those involving the cortical veins directly or indirectly by means of reflux from the diseased sinus are at risk of hemorrhage, seizures, focal neurologic deficits, myelopathy and dementia (1–3).
Conventional CT and MR techniques are of limited value in the diagnosis and classification of DAVF. Spin-echo MR images may be entirely normal unless occlusion of the venous sinus, enlarged arterial pedicles, engorged cortical veins, or established intracranial complications (eg, venous ischemia and hemorrhage) are present. Contrast-enhanced TOF MR angiography may allow visualization of abnormal arterial pedicles and static venous anatomy, but only MR DSA enables dynamic assessment of the cerebral circulation (4, 5).
MR-DSA techniques involve the use a contrast medium bolus and a digital mask (5, 6). Typically, the matrix size is 256, and the temporal resolution is one frame per second. Currently, MR DSA lacks the spatial resolution of high-quality TOF MR angiography; therefore, it is not appropriate for the study of lesions such as small aneurysms, but its dynamic capability makes the technique ideally suited to the study of shunting arteriovenous malformations (AVMs).
Our MR-DSA protocol has been described in detail before (6), but it is summarized here. It involves a gradient-echo T1-weighted sequence, identical to that used for standard volume acquisitions, except that single 6–10-cm sections are acquired every second. A mask acquisition is obtained, followed by 60-second contrast-enhanced acquisitions with 5–9 mL of gadopentetate dimeglumine in the frontal (Towne) and lateral projections. The data are then imported into a proprietary software package that can be used to produce intensity-versus-time plots based on the T1 shortening effect of gadolinium. Using this technique, we examined three patients with DAVFs that were confirmed at catheter angiography. It proved possible to identify the larger of the arterial pedicles and demonstrate synchronous opacification of the intracranial carotid artery and diseased sinus. Furthermore, we were able to identify patients who were at greatest risk of neurologic complications because the patency of vessels and direction of flow within the venous sinuses could be demonstrated. DAVF without retrograde filling of the venous sinus and cerebral and/or spinal veins are considered to pose much less risk of neurologic complications than fistulae with venous reflux. We have not yet encountered a patient with retrograde filling of leptomeningeal veins due to a DAVF, but we know from experience with brain AVMs (6) that the technique has the spatial resolution to permit identification of these structures. The demonstration of a large vein of Labbé entering the diseased sinus in case 3 meant that we were able to dismiss the possibility of venous sacrifice with MR examination alone. Whether MR DSA in its current form can be used to identify fistulae that involve only the cortical veins (types 3 and 4) remains to be seen.
Our current MR-DSA protocol is clearly inferior to that of catheter angiography, and therefore, invasive vascular imaging is still necessary to document the detailed anatomy of the arterial pedicles and the exact relationship of normal cortical veins to the site of the fistula. The latter is imperative if the DAVF is to be treated by obliterating the venous sinus. However, MR imaging does have a theoretical advantage compared with catheter angiography in that MR perfusion techniques may prove useful in studying the effects of a DAVF on local and regional perfusion. Furthermore, MR DSA can be used to noninvasively characterize the transit of a gadolinium-based contrast agent through the cerebral circulation. So far, we have not performed a perfusion MR examination in a patient with a DAVF, but we are encouraged by the potential of MR DSA in identifying and monitoring patients with venous hypertension with plots of venous signal intensity in relation to an arterial input.
Conclusion
Many patients present with symptoms or signs that might be attributable to a DAVF, but few actually have a vascular malformation. It is difficult to know which patients with pulsatile tinnitus, seizures, or symptoms related to unexplained intracranial hypertension should undergo conventional catheter angiography, a procedure that involves ionizing radiation and a risk (albeit small) of permanent neurologic damage. We believe MR DSA is ideally suited for the investigation of these groups of patients to identify the minority that has a potentially dangerous vascular malformation. MR DSA also shows potential for use in the classification and pretherapeutic evaluation of DAVF. The technique will also permit noninvasive follow-up of treated lesions and those that are managed conservatively. The latter is important because, as is well recognized, benign fistulae may transform into more aggressive lesions if the pattern of venous drainage changes (7).
Addendum
We have now had the opportunity to study eight DAVFs with MR DSA, two of which were confirmed to be Djindjian type III lesions with catheter angiography.
References
- 1.Djindijan R, Merland J, Theron J. Superselective Arteriography of the External Carotid Artery. New York, NY: Springer-Verlag;1977;606–628
- 2.Lasjaunias P, Chiu M, Terbrugge KT, et al. Neurological manifestations of intracranial dural sinus arteriovenous malformations. J Neurosurg 1986;64:724–730 [DOI] [PubMed] [Google Scholar]
- 3.Awad I, Little J, Akrawi W, et al. Intracranial dural arteriovenous malformations: factors predisposing to an aggressive neurological course. J Neurosurg 1990;72:839–850 [DOI] [PubMed] [Google Scholar]
- 4.Warren DJ, Hoggard N, Walton L, et al. Cerebral arteriovenous malformations: comparison of novel magnetic resonance angiographic techniques and conventional catheter angiography. Neurosurgery 2001;48:973–982 [PubMed] [Google Scholar]
- 5.Aoki S, Nanbu A, Yoshikawa T, et al. 2D thick-slice MR digital subtraction angiography with one-second temporal resolution: assessment of cerebrovascular disorders. In: Proceedings of the Annual Meeting of the American Society of Neuroradiology, 1999. Oak Brook, IL: American Society of Neuroradiology;1999;122
- 6.Griffiths PD, Hoggard N, Warren DJ, et al. Brain arteriovenous malformations: assessment with dynamic MR digital subtraction angiography. AJNR Am J Neuroradiol 2000;21:1892–1899 [PMC free article] [PubMed] [Google Scholar]
- 7.Cognard C, Houdart E, Casasco A, et al. Long term modification of intracranial dural arteriovenous fistulas leading to a worsening in the type of venous drainage. Neuroradiology 1997;39:59–56 [DOI] [PubMed] [Google Scholar]