Abstract
Summary: Riedel's thyroiditis is a rare disorder of unknown etiology and may be seen isolated or as a part of multifocal fibrosclerosis. It is important to distinguish Riedel's thyroiditis from thyroid carcinoma. Reports about imaging features of Riedel's thyroiditis are limited in the radiologic literature. We describe herein CT and MR imaging features of Riedel's thyroiditis in a case of multifocal fibrosclerosis with previously unreported radiologic observations.
Multifocal fibrosclerosis is a rare syndrome characterized by fibrosis involving multiple organ systems (1). Varying combinations of involvement have been reported: Riedel's thyroiditis, retroperitoneal fibrosis, orbital pseudotumor, mediastinal fibrosis, and sclerosing cholangitis (1–4). Although it is important to distinguish Riedel's thyroiditis from thyroid carcinoma, reports about imaging features of Riedel's thyroiditis are very limited in the radiologic literature (5–8). Herein, we describe imaging features of Riedel's thyroiditis in a case of multifocal fibrosclerosis with previously unreported radiologic observations.
Case Report
A 46-year-old man presented with dysphagia and hoarseness. Physical examination revealed an enlarged and hard thyroid gland. Laboratory findings were remarkable for high levels of alkaline phosphatase and γ-glutamyl transferase. Sedimentation rate was 45 mm/hr. Sonography demonstrated a symmetrically enlarged and hypoechoic thyroid. Scintigraphy failed to reveal any uptake in the gland. CT of the neck showed an enlarged and hypodense thyroid gland surrounding the trachea posteriorly and compressing the esophagus. After infusion of contrast medium, most of the thyroid showed decreased enhancement, whereas a small area in the gland enhanced normally (Fig 1A). MR imaging of the neck showed a mass that was hypointense on T1- and T2-weighted images, replacing most of the thyroid gland with minimal enhancement after gadolinium injection (Fig 1B–D). Anterior to the mass was seen a small amount of normal thyroid parenchyma with normal intensity and normal enhancement after gadolinium injection. No abnormal lymph node was identified in the neck. Fine needle aspiration biopsy was attempted but could not be performed because of hardness of the mass. Tru-cut biopsy of the thyroid revealed only dense fibrous tissue with some inflammatory cells lacking vessels. No acini were seen. Histopathologic findings were diagnostic for Riedel's thyroiditis.
fig 1.
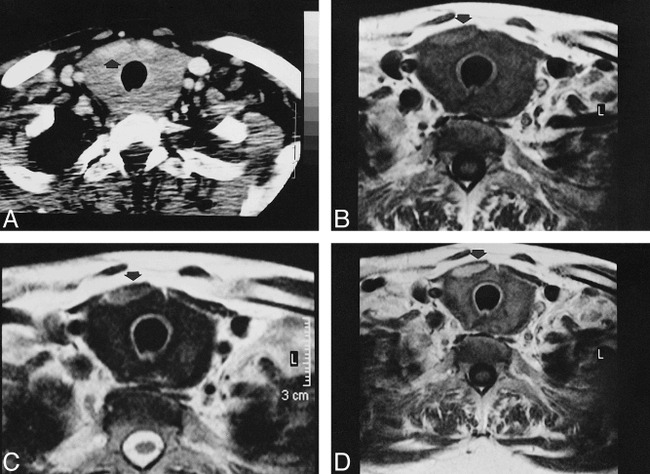
A, Enhanced CT of the neck shows an enlarged and hypodense thyroid gland surrounding the trachea and compressing the esophagus. Note the small piece of normal enhancing thyroid tissue (arrow).
B and C, T1-weighted (560/25/2 [TR/TE/excitations]) unenhanced (B) and fast spin-echo T2-weighted (3800/96/3) (C) MR images of the neck showing the enlarged and diffusely hypointense thyroid gland with a small piece of thyroid tissue with normal intensity (arrow).
D, T1-weighted (560/25/2) MR image after administration of gadolinium shows an extremely diminished enhancement of most of the thyroid gland. Note the anteriorly located normal thyroid tissue with normal homogenous enhancement (arrow).
Abdominal sonography showed segmental dilatations in the left intrahepatic biliary tract. Abdominal CT confirmed the findings on sonography. Retroperitoneal fibrosis surrounding the abdominal aorta also was noted. Endoscopic retrograde cholangiopancreatography revealed multiple segmental dilatations and strictures in the left intrahepatic biliary tract consistent with sclerosing cholangitis. CT of the thorax and MR imaging of the orbits were within normal limits. The patient was given corticosteroid therapy with the diagnoses of Riedel's thyroiditis, retroperitoneal fibrosis, and sclerosing cholangitis. After 3 months of corticosteroid therapy, dysphagia and hoarseness disappeared; the size of the thyroid gland diminished on palpation; laboratory values became normal; and sonography and CT findings of the liver returned to normal. Follow-up MR imaging of the thyroid revealed no significant change in size or MR characteristics of the mass 6 months later.
Discussion
Multifocal fibrosclerosis is a rare syndrome of unknown etiology characterized by fibrosis involving multiple organ systems (1). Retroperitoneal fibrosis, Riedel's thyroiditis, orbital pseudotumor, mediastinal fibrosis, and sclerosing cholangitis have been reported to be a part of this syndrome (1–4). Isolated reports of pulmonary fibrosis, fibrous parotitis, fibrosclerosis in the kidneys and pituitary gland, pancreatic fibrosis, testicular fibrosis, Dupuytren's contracture, subcutaneous fibrosis, vasculitis, and neurologic involvement also have been reported.
Riedel's thyroiditis may be seen isolated or as a part of multifocal fibrosclerosis. Its major clinical significance lies in its ability to mimic invasive thyroid carcinoma. Some affected patients benefit from corticosteroid therapy (6–8). On imaging, Riedel's thyroiditis is reported to be homogeneously hypoechoic on sonography and shows hypodense-to-normal thyroid tissue on CT scans (5). Slight enhancement of the mass has been noted after administration of contrast medium (7). Invasion of nearby soft tissues or compression of the trachea or esophagus or a combination of these three characteristics may be observed. Only two case reports have defined MR imaging features of Riedel's thyroiditis. The thyroid was reported to be hypointense on both T1- and T2-weighted images (5, 6), with marked homogeneous enhancement after gadolinium administration (6). Our sonography, unen-hanced CT, and unenhanced MR imaging features were similar to those presented in the literature. We observed, however, a considerably decreased enhancement after gadolinium administration on MR imaging. Decreased enhancement also was observed after administration of iodinated contrast medium on CT, which increased the contrast between the normal thyroid tissue and the fibrotic parenchyma. We think that decreased enhancement after administration of contrast medium was caused by dense fibrosis that replaced most of the thyroid gland and was consistent with extremely diminished vascularity compared with the normal, highly vascular, thyroid parenchyma.
Conclusion
We described imaging features of Riedel's thyroiditis in a patient with multifocal fibrosclerosis. A thyroid hypodense on CT and hypointense on T1- and T2-weighted MR images can be suggestive of Riedel's thyroiditis whether invasion to nearby soft tissues is observed or not. Administration of contrast medium may be helpful in differentiating the normal thyroid parenchyma from the fibro-sclerotic mass. To our knowledge, no other entity causes diffuse decreased enhancement after gadolinium administration on MR imaging or administration of iodinated contrast medium on CT. Therefore, these radiologic findings may be diagnostic for Riedel's thyroiditis.
Footnotes
Address reprint requests to Ali Özgen, MD, Sporcular Sitesi, Ilkyerlesim Mahallesi, 438. sokak, No:12, Batikent, 06370, Ankara, Turkey.
References
- 1.Comings DE, Skubi KB, Van Eyes J, Motulsky AG. Familial multifocal fibrosclerosis. Ann Int Med 1967;66:884-892 [DOI] [PubMed] [Google Scholar]
- 2.Laitt RD, Hubscher SG, Buckels JA, Darby S, Elias E. Sclerosing cholangitis associated with multifocal fibrosis: a case report. Gut 1992;33:1430-1432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Aylward GW, Sullivan TJ, Garner A, et al. Orbital involvement in multifocal fibrosclerosis. Br J Ophthalmol 1995;79:246-249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yousem DM, Scheff A. Thyroid and parathyroid. In: Som PM, Curtin HD, eds Head and Neck Imaging 3rd ed. St. Louis, Mo: Mosby; 1996;952-975
- 5.Perez Fontan PJ, Cordido Carballido F, Pompo Felipe F, et al. Riedel thyroiditis: US, CT, and MR evaluation. J Comput Assist Tomogr 1993;17:324-325 [PubMed] [Google Scholar]
- 6.Lo JC, Loh KC, Rubin AL, et al. Riedel's thyroiditis presenting with hypothyroidism and hypoparathyroidism: dramatic response to glucocorticoid and thyroxine therapy. Clin Endocrinol 1998;48:815-818 [DOI] [PubMed] [Google Scholar]
- 7.Malotte MJ, Chonkich GD, Zuppan CW. Riedel's thyroiditis. Arch Otolaryngol Head Neck Surg 1991;117:214-217 [DOI] [PubMed] [Google Scholar]
- 8.Belsing TZ, Rasmussen UF. Riedel's thyroiditis: an autoimmune or primary fibrotic disease? J Int Med 1994;235:271-274 [DOI] [PubMed] [Google Scholar]


