Abstract
Background:
Utilization of family planning services improves women’s reproductive health outcomes. Long-acting reversible contraceptive (LARCs) methods, in particular, prevent unwanted pregnancy and significantly reduce maternal mortality and morbidity. In Ethiopia utilization of LARCs was very low. Therefore, this study was aimed at assessing the utilization of LARCs and associated factors among reproductive-age women in Wondo Genet District, Southern Ethiopia.
Method:
Institution based cross-sectional study was conducted from 15 May to 15 August 2020 among reproductive-age women. A systematic sampling method was applied to recruit 376 women and the sample size was allocated to health centers proportionally. Data collection was conducted by trained collectors using pretested and structured questionnaires. Data coded and entered into EPI Info 7 and the analysis was done using SPSS version 25. Binary and multiple logistic regression analyses were done. Statistical significance was declared with P < 0.05.
Result:
The utilization of LARCs was 37.8% (95% CI: 32.9-42.7). The multivariable analysis showed that odds of the utilization of LARCs were increased among reproductive-aged ≥25 years (Adjusted odds ratio (AOR) = 2.21, 95% CI: 1.04, 4.41), gave birth to ≥3 live births (AOR = 2.2, 95% CI: 1.2, 4.04), employed (AOR = 1.92, 95% CI: 1.17, 3.14), earned high monthly income (AOR = 2.02, 95% CI: 1.25, 3.26) and discussed contraceptive methods with their husbands (AOR = 2.87, CI: 1.68, 4.89].
Conclusions:
Utilization of LARCs was low. The odds of the utilization of LARCs were increased in women aged ≥25 years, gave birth to 3 or more children, earned high monthly income, and discussed with their husbands about contraception methods.
Keywords: contraceptives, reproductive age women, utilization, association, Wondo Genet district
Introduction
Family planning services are one of the key components of safe motherhood.1 Reduction in fertility by accessing family planning services to reproductive-age women is crucial to improve reproductive health outcomes.2 Among the 1.9 billion women of reproductive age living in the world in 2019, 1.1 billion have a need for family planning (FP). Of those who have a need for family planning, 842 (44%) and 80 (4%) million use modern and traditional methods respectively. 190 million women want to avoid pregnancy but do not use any contraceptive method (have an unmet need for family planning).3
Globally, the contraceptive prevalence rate increased slightly and the use of specific methods varied widely.4 In 2019, 45.2% of contraceptive users relied on permanent or long-acting methods (implant, intrauterine device and female and male sterilization), 46.1% on a short-acting methods (male condom, the pill and injectable) while remaining on traditional methods (rhythm/calendar and withdrawal/coitus interruptus methods).3 Short-acting methods constituted more than half of all contraceptive methods used in sub-Saharan Africa countries.5,6
In sub-Saharan Africa countries, the fertility rate is relatively high.7 The main reason for the high fertility rate across the region was the low level of contraceptive uptake and high unmet needs for contraception.4 Even if contraceptives utilization has increased across the region in the recent years, the region has the lowest rates of contraceptive prevalence.8 Countries in the region tried their best to improve the contraceptive prevalence rates using available policies.9 Despite all their efforts, long acting reversible contraceptive utilization remained very low.10
Ethiopia is the second-most populous country in Africa. The average number of children a woman would have by the end of her childbearing years per 1,000 women (total fertility rate) was 4.6 in 2016 but the modern contraceptive prevalence rate (CPR) among married Ethiopian women was 36%. The utilization of the contraceptive method was dominated by the use of injectables and pills.11 The government intended to increase implants and intrauterine contraceptive device(IUCD) utilization to 33% and 15% respectively in the method mix by strengthening public and private sectors providing services of reversible long-acting methods using static and outreach programs12 but only 8% and 2% of currently married women used implants and IUCD respectively.11
Several factors affected the utilization of long-acting reversible contraceptives in Ethiopia.13 Identification of factors affecting the utilization of FP services is crucial. Recent Ethiopia Demographic and Health Survey (EDHS) identified the place of residence, education level, and wealth quintiles of women as factors that affected the uptake of family planning but uncover the major reasons for not using reversible long-acting family planning specifically. Therefore, this study was aimed at assessing the utilization of the reversible long acting reversible contraceptives its determinants among reproductive-age women in the Wondo Genet District, Sidama National Regional state.
Methodology
Study Design
An institution-based cross-sectional study among reproductive-age women attending health centers for family planning service was held from May 15 to August 15, 2020, in 3 health centers of Wondo Genet District. Wondo Genet District is located 261 km south of Addis Ababa, the capital of Ethiopia, and 24 km east of Hawassa City, the capital of the region. It’s one of the districts found in the Sidama National Regional State. According to the 2007 Ethiopian population and housing census, the total population residing in the district was estimated at about 154, 363 of which 35,503 childbearing age women. The district has 3 health centers providing health services for the community. The study populations were all reproductive-age women in the district who attended health centers for family planning services.
Sample Size Determination and Sampling Technique
The sample size was computed using the single population proportion formula taking into account the following assumption: 95% confidence level, 5% margin of error, 33.5%14 expected magnitude of long-acting reversible contraceptives utilization, and 10% non-response rate. A sample size of 376 was computed.
The average numbers of clients visited the family planning service unit daily during data collection period was estimated based on the previous 2 months’ daily client flow of the units which was obtained by referring client registration/record prior to data collection. The sample size was proportionally allocated to the health centers. Study participants were selected using a systematic random sampling technique with an interval of 2 where the interval constant was obtained by dividing the total modern contraceptive users in the health center to the sample size.
Data Collection and Quality Control
Data were collected using structured, interviewer administered questionnaire. The questionnaire was adapted and modified from different related literatures,11,15 prepared in English language and translated into local language (Sidamu Afoo) for data collection by 2 native speakers who got Master in Sidamu Afoo language studies. Similarly, back translation to English language was done by language experts. Six midwifery nurses and 3 public health officers participated in data collection and supervision respectively. Data collectors and supervisors were trained for 2 days. Supervisors and principal investigators checked the consistency and completeness of the questionnaire.
Data Management and Analysis
Principal investigators reviewed and organized data after the collection; then coded and entered it into EPI Info 7 and the analysis was done using SPSS version 25.0. The statistical significance and strength of the association between independent variables and an outcome variable were measured by a bivariable logistic regression model with a p-value of less than 0.25. Then multivariable logistic regression was used to decrease the effect of confounding factors and statistical significance was declared with P < 0.05. Finally, the result was presented using the table.
Ethical Approval
Ethical clearance was obtained from the Institutional Review Board of Yirgalem Hospital Medical College (IRB). Wondo Genet District Health Office provided permission to conduct this survey in the study area. Verbal consent was obtained from each study participant prior to participation in the study after the nature of the study was fully explained to them.
Result
Socio Demographic and Economic Characteristics of Study Participants
A total of 376 reproductive-age women participated in the study making the response rate 100%. The mean age (±SD) of the study subjects was 27.1 ± 5.2 years. The age range of women was between 18-44 years. About two-thirds of respondents, 250 (66.5%) were aged ≥25 years. Regarding ethnicity, three fourth, 281(74.7%) of the respondents were Sidama, and 303 (80.6%) were protestant religious followers. All of the study participants were currently married and the majority of them (82.4%) have ≥5 family members. Near to three fourths (71.8%) of women were rural dwellers.
Pertaining to education, 219 (58.2%) women and half of their husbands were did not attend formal education. More than half, 217(57.7%) of study participants were housewives whereas only 86 (22.9%) of their husbands were employed. About two-third, 242(64.4%) of women’s family earned monthly income less than 2000 Ethiopian birr (Table 1).
Table 1.
Socio-Demographic Characteristics of Study Participants in Wondo Genet Woreda, Sidama Region, Southern Ethiopia.
| Variable (n = 376) | Category | Frequency | Percent (%) |
|---|---|---|---|
| Age | ≤ 25 years | 126 | 33.5 |
| >25 years | 250 | 66.5 | |
| Ethnicity | Sidama | 281 | 74.7 |
| Oromo | 60 | 16.0 | |
| Amhara | 35 | 9.30 | |
| Religion | Protestant | 303 | 80.6 |
| Orthodox | 43 | 11.4 | |
| Muslim | 30 | 8.00 | |
| Education level | Not attended formal education | 219 | 58.2 |
| Primary education | 90 | 23.9 | |
| Secondary education and above | 67 | 17.8 | |
| Husband’s education level | Not attended formal education | 193 | 51.3 |
| Primary education | 97 | 25.8 | |
| Secondary education and above | 86 | 22.9 | |
| Occupation of women | Housewife | 217 | 57.7 |
| Employed | 159 | 42.3 | |
| Income level | < 2000 Ethiopian Birr | 134 | 35.6 |
| ≥2000 Ethiopian Birr | 242 | 64.4 | |
| Family size | ≤ 4 members | 66 | 17.6 |
| ≥5 members | 310 | 82.4 | |
| Place of residence | Rural | 270 | 71.8 |
| Urban | 106 | 28.2 |
Reproductive History of Respondents
Concerning the parity of women, 350(93%) gave at least 1 birth before and 3.7% had a history of miscarriage. Of 376 respondents, 235 (62.5%) gave more than 2 live births during the study period. About half, 193(51.3%) women had the desire to give birth to additional children in their reproductive life. All of the married women responded that the desired number of children was decided with their husband jointly (Table 2).
Table 2.
Reproductive History of the Study Participants in Wondo Genet Woreda, Sidama Region, Southern Ethiopia.
| Variable (n = 376) | Category | Frequency | Percent (%) |
|---|---|---|---|
| Parity | Null | 26 | 7 |
| Prime | 115 | 30.6 | |
| Multi | 235 | 62.5 | |
| History of miscarriage | Yes | 14 | 3.7 |
| No | 362 | 96.3 | |
| Future desire to fertility | Yes | 193 | 51.3 |
| No | 183 | 48.7 |
Information About Contraceptives Methods
More than two-thirds (70%) of women owned a radio and/ or television. About two-thirds, (62%) of women heard about contraceptive methods. Mass media was the source of information for 60% of women. More than half (56.6%) of women reported that they were counseled about LARCs use during health facilities visits.
Long Acting Reversible Contraceptives Utilization
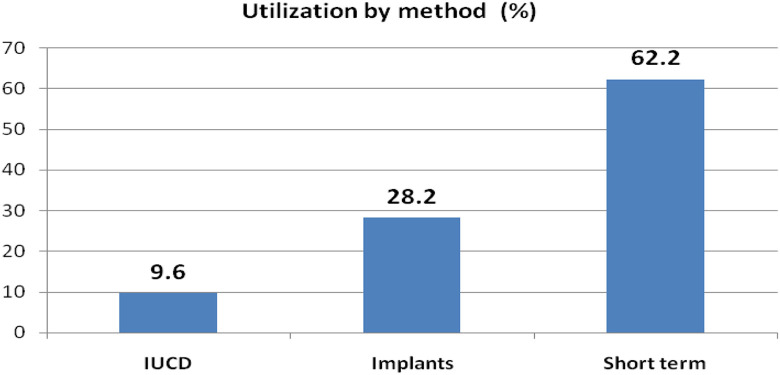
Among the study participants, the utilization of reversible long-acting contraceptives was 37.8% (95% CI: 32.9-42.7). From them, 106(28.2%) used implants whereas 36(9.6%) utilized IUCD (Figure 1). Eight in 10 women received services from government health institutions. About three-fourths, (72.3%) of women discussed contraceptive methods with their husbands. About half of women’s husbands supported the utilization of LARCs (Figure 1).
Figure 1.
Utilization contraceptives by method in Wondo Genet district.
Associated Factors of LARCs Utilization
Both bivariable and multivariable logistic regression analysis were done to identify the independent predictors of LARCs utilization among reproductive-age women. All the variables were analyzed in bivariable logistic regression analysis and those with a p-value less than 0.2 were considered in multivariable logistic regression analysis. The multivariable logistic regression analysis outputs confirmed that the age of women (p ≤ 0.025), occupation (p ≤ 0.009), income level (p ≤ 0.004), number of live births (p ≤ 0.010), and discussion with husbands about LARC use with husbands (p ≤ 0.0001) were independent predicators of LARCs utilization.
Compared to their counterparts, the odds of the utilization of long-acting reversible contraceptives were higher among reproductive-age women with age 25 years or older (AOR = 2.21, 95% CI: 1.04, 4.41), In regard to respondent occupation, those who were employed (salaried) (AOR = 1.92, 95% CI: 1.17, 3.14) had the highest odds of utilizing long acting reversible contraceptives. Further, the study revealed that as the household income increased, the chances of using LARCs also improved. Women with household monthly income ≥2000 Ethiopian Birr (AOR = 2.02, 95% CI: 1.25, 3.26) were 2 times more likely to utilize LARCs as compared to those who had an income of less than 2000 Ethiopian Birr.
Similarity, the number of live births was also shown to be positively associated with the utilization of long acting reversible contraceptives in reproductive age women (AOR = 2.2, 95% CI: 1.2, 4.04). About 2.2 times increased odds of LARCs utilization were observed among reproductive-age women who gave birth to ≥3 live births. Furthermore, this study reported that those reproductive-age women who had discussed contraceptive methods with their husbands were about 3 times more likely to utilize LARCs (AOR = 2.87, CI: 1.68, 4.89) (Table 3).
Table 3.
Associated Factors of LARCs Utilization Among Study Participants in Wondo Genet Woreda, Sidama Region, Southern Ethiopia.
| Variable (n = 376) | Category | Use of LARCs | COR (95% CI) | AOR (95% CI) | P-value | |
|---|---|---|---|---|---|---|
| Yes | No | |||||
| Place of residence | Rural | 113 | 157 | 1.91(1.71-3.12) | 1.35(0.79-2.33) | 0.27 |
| Urban | 29 | 77 | 1 | 1 | ||
| Age of women | < 25 years | 38 | 88 | 1 | 1 | |
| ≥25 years | 104 | 146 | 1.65(1.04-2.60) | 2.21(1.10-4.44)** | 0.025 | |
| Women education | Illiterate | 87 | 132 | 1.44(0.81-2.59) | 1.01(0.52 -1.96) | 0.97 |
| Primary | 34 | 56 | 1.33(0.68-2.59) | 1.09(0.53-2.27) | 0.81 | |
| ≥secondary | 21 | 46 | 1 | 1 | ||
| Women occupation | Housewife | 63 | 154 | 1 | 1 | |
| Employed | 79 | 80 | 2.14(1.57-3.70) | 1.92(1.17-3.14)** | 0.009 | |
| Family income level | <2000 Birr | 70 | 64 | 1 | 1 | |
| ≥2000 Birr | 72 | 170 | 2.58(1.67-3.99) | 2.02(1.25-3.26)** | 0.004 | |
| Family size of women | ≤ 4 | 26 | 40 | 1 | 1 | |
| ≥5 | 116 | 194 | 1.09(0.63-1.87) | 1.37(0.58-3.19) | 0.47 | |
| Number of live births | ≤ 2 | 64 | 77 | 1 | 1 | |
| ≥3 | 78 | 157 | 1.67(1.09-2.57) | 2.20(1.21-4.04)** | 0.01 | |
| Family own radio/TV | Yes | 93 | 170 | 1.43(0.89-2.19) | 1.23(0.71-2.15) | 0.46 |
| No | 49 | 64 | 1 | 1 | ||
| Women heard about LARCs | Yes | 85 | 148 | 1.54(0.75-1.77) | 1.07(0.65-1.75) | 0.79 |
| No | 57 | 86 | 1 | 1 | ||
| Counseled about LARCs | Yes | 76 | 137 | 1.23(0.81-1.87) | 0.78(0.49-1.24) | 0.29 |
| No | 66 | 97 | 1 | 1 | ||
| Discussed with husbands | Yes | 81 | 191 | 3.34(2.09-5.35) | 2.86(1.68-4.89)** | 0.0001 |
| No | 61 | 43 | 1 | |||
| Husbands’ support | Yes | 74 | 130 | 1.15(0.76-1.74) | 1.13(0.71-1.81) | 0.61 |
| No | 68 | 104 | 1 | 1 | ||
Discussion
This study came up with utilization of long-acting reversible contraceptives among reproductive-age women attending health centers of Wondo Genet district for family planning service was 37.8%. Utilization of LARCs was found to be associated with women age, parity, occupation, monthly income, and discussion with husbands about contraception methods.
Utilization of long-acting reversible contraceptives among reproductive-age women attending health centers for family planning service was 37.8%. Previous studies conducted in Arsi Negel 33.5% 16,14 Wolaita Zone 38%,17 Hossana 36.5%,18 Gondar City 33.7%,16 Harar City 38%,19 and Afar Region 33.4%20 reported the similar finding. The finding was higher than the study done in different parts of Ethiopia,21-25 Kenya,26,27 Uganda28 and Nepal.29 Increased utilization of LARCs in this might be due to improved awareness of women on LARCs and differences in study time, setting, and socio-demographic backgrounds.
The current study showed women aged ≥ 25 years and who gave birth to 3 or more children utilized LARCs more compared to those with age less than 25 years. This finding is consistent with a study conducted in the Afar region,20 Uganda,28 and Nigeria.30 This might be explained as those women who had already attained their plan of fertility could use LARCs up to reaching menopause. Similarly, increased utilization of LARCs was observed among employed women compared to their counterparts. This finding is in line with studies conducted in different parts of Ethiopia31-33 and Kenya.26,34 This could have happened because employed women have increased access to information and frequent health institution contact to access the service LARCs methods.
Improved utilization of LARCs was observed in women who have a better monthly income. This finding is consistent with EDHS 2016, which reported that contraceptive use increased from 20% for women in the lowest wealth quintile to 47% for women in the highest wealth quintile Afar15 and Nepal.29 This implies that empowering women in income and decision-making power are essential strategies to improve FP use and betterment of health status of reproductive-age women and the community as a whole.
Discussion with husbands and husbands’ approval of methods played a significant role in utilization of long acting reversible contraceptives. Women who discussed contraceptives with their husbands utilized LARCs 3 times more likely than their counterparts. This finding was comparable with studies in Arsi Negele14 and Arbaminch32 and Nigeria.30 This could have happened because jointly decision with husbands on methods choice and fertility comfort women and increase their intention to use long-acting reversible contraceptives.
Strength and Limitation
This study tried to assess the utilization of LARCs and incorporate as many predictors of LARC utilization as possible. However, the study was not free from some limitations. This study was institution based and therefore, it might not be possible to generalize the current findings to the entire reproductive-age female population in the district. In addition, Quantitative nature of the study hinders in-depth exploration of women’s perception and barriers for LARCs use.
Researchers should conduct further studies on assessing the quality of service given and additional factors affecting the utilization. Including in-depth or focus group interviews enhance their understanding of women’s perception and barriers for LARCs use.
Conclusion
The utilization of long-acting reversible contraceptives was comparable with studies done in different parts of Ethiopia. The odds of the utilization of LARCs were increased in women aged ≥25 years, who gave birth to 3 or more children, high monthly income, and discussed with their husbands about contraception methods. Community and facility-level awareness creation and empowering women in income and decision making power should be strengthened to improve the utilization of long-acting reversible contraceptives.
Abbreviations
AOR: Adjusted Odds Ratio; CI: Confidence Intervals; COR: Crude Odds Ratio; CPR: Contraceptive Prevalence Rate; EDHS: Ethiopia Demographic and Health Survey; IRB: Institutional Review Board; IUCD: Intrauterine Contraceptive Device; LARCs: Long-acting Reversible Contraceptives; SD: Standard Deviation; WHO: World Health Organization.
Author Biographies
Amelo Bolka Gujo has a Master Degree in General Public Health and Applied Human Nutrition from Hawassa University and is Lecturer of Public Health/Nutrition in Yirgalem Hospital Medical College.
Assefa Philipos Kare has a Master Degree in General Public Health from Hawassa University and is Lecturer of Public Health in Yirgalem Hospital Medical College.
Footnotes
Author Contributions: Study conceptualization, AB and AP; data curation, AB and AP; methodology AB and AP; formal analysis, AB and AP; funding acquisition, AB; investigation, AB and AP, software, AB and AP; supervision, AP; validation, AP; visualization, AB and AP; writing original manuscript, AB; review and editing, AB and AP.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The financial support for this study came from Yirgalem Hospital Medical College. Funding body did not involve in the collection, analysis, and interpretation of data and in writing of the manuscript.
ORCID iD: Amelo Bolka Gujo  https://orcid.org/0000-0002-1233-8899
https://orcid.org/0000-0002-1233-8899
References
- 1. Cleland J, Bernstein S, Ezeh A, Faundes A, Glasier A, Innis J. Family planning: the unfinished agenda. Lancet. 2006;368(9549):1810–1827. [DOI] [PubMed] [Google Scholar]
- 2. Osotimehin B. Family planning as a critical component of sustainable global development. Glob Health Action. 2015;8:29978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. United Nations, Department of Economic and Social Affairs, Population Division. Contraceptive Use by Method 2019: Data Booklet (ST/ESA/SER.A/435). United Nations, Department of Economic and Social Affairs, Population Division; 2019. [Google Scholar]
- 4. Alkema L, Kantorova V, Menozzi C, Biddlecom A. National, regional, and global rates and trends in contraceptive prevalence and unmet need for family planning between 1990 and 2015: a systematic and comprehensive analysis. Lancet. 2015;(12):1–11. [DOI] [PubMed] [Google Scholar]
- 5. Ahmed S, Choi Y, Rimon JG, et al. Trends in contraceptive prevalence rates in sub-Saharan Africa since the 2012 London Summit on Family Planning: results from repeated cross-sectional surveys. Lancet Global Health. 2019;7(7):e904–e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Slaymaker E, Scott RH, Palmer MJ, et al. Trends in sexual activity and demand for and use of modern contraceptive methods in 74 countries: a retrospective analysis of nationally representative surveys. Lancet Global Health. 2020;8(4):e567–e79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Cahill N, Sonneveldt E, Stover J, et al. Modern contraceptive use, unmet need, and demand satisfied among women of reproductive age who are married or in a union in the focus countries of the Family Planning 2020 initiative: a systematic analysis using the Family Planning Estimation Tool. Lancet. 2018;391(10123):870–882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. United Nations Department of Economic and Social Affairs. World Family Planning Highlights. United Nations Department of Economic and Social Affairs; 2017. [Google Scholar]
- 9. Gaffield ML, Festin M. World Health Organization Family Planning Guidelines Tools. World Health Organization Press; 2017. [Google Scholar]
- 10. Adedini SA, Omisakin OA, Somefun OD. Trends, patterns and determinants of long-acting reversible methods of contraception among women in sub-Saharan Africa. PLoS One. 2019;14(6):e0217574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Agency Central Statistical, ICF. Ethiopia Demographic and Health Survey. Agency Central Statistical, ICF; 2016. [Google Scholar]
- 12. Ethiopia Ministry of Health. Ethiopia-Health-Sector-Transformation-Plan of 2015-2020. Ethiopia Ministry of Health; 2015. [Google Scholar]
- 13. Hrusa G, Spigt M, Dejene T, Shiferaw S. Quality of Family Planning Counseling in Ethiopia: trends and determinants of information received by female modern contraceptive users, evidence from national survey data, (2014-2018). PLoS One. 2020;15(2):e0228714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hibstu DT, Alemayehu A. Long acting reversible contraceptives utilization and associated factors among women of reproductive age in Arsi Negele town, Southeastern Ethiopia. Contracept Reprod Med. 2020;5:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Alemayehu M, Lemma H, Abrha K, et al. Family planning use and associated factors among pastoralist community of afar region, eastern Ethiopia. BMC Womens Health. 2016;16:39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Tulu AS, Gebremariam T. Utilization of reversible long acting contraceptive methods and associated factors among women getting family planning service in governmental health institutions of Gondar City Administration, Northwest Ethiopia. Int J Med Sci Public Health. 2018;8(2):178–187. [Google Scholar]
- 17. Meskele M, Mekonnen W. Factors affecting women’s intention to use long acting and permanent contraceptive methods in Wolaita Zone, Southern Ethiopia: a cross-sectional study. BMC Womens Health. 2014;14:109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Woldu BF, Ermolo TL, Lemu LG, Gejo NG. Long-acting reversible contraception utilization and associated factors among women in extended postpartum period in Hossana town, southern Ethiopia: cross sectional study. Contracept Reprod Med. 2020;5:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Shiferaw K, Musa A. Assessment of utilization of long acting reversible contraceptive and associated factors among women of reproductive age in Harar City, Ethiopia. Pan Afr Med J. 2017;28:222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Muhammed MA, Abdo RA. Long-acting reversible contraceptive utilization and its associated factors among family planning users in pastoral communities of Afar region, Ethiopia: a facility-based crosssectional study. J Midwifery Reproductive Health. 2020;8(1):2022–2032. [Google Scholar]
- 21. Animen S, Lake S, Mekuriaw E. Utilization of intra uterine contraceptive device and associated factors among reproductive age group of family planning users in Han Health Center, Bahir Dar, North West Amhara, Ethiopia, 2018. BMC Res Notes. 2018;11(1):922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kelborea W, Yesufb N, Alto G. Long acting reversible contraceptive methods switching and associated factors among women attending family planning clinic at public health facilities of Dilla Town, Southern Ethiopia. Int J Sci Basic Appl Res. 2020;53(2):59–72. [Google Scholar]
- 23. Goshu YA, Hayley M. Prevalence of long-acting reversible contraceptive among women of reproductive age group in Debre Tabor Town Visiting Health Institution, North-West Ethiopia 2018. an institutional based study. J Women Health Safety Res. 2020;4(1):127–134. [Google Scholar]
- 24. Ayenew AA, Mulat A, Hiyaru T. Utilization of long acting reversible contraceptive methods and associated factor among women who came for family planning service in Bahir Dar City Public Health Facility, North West, Ethiopia, Institutional Based Cross Sectional Study. J Women’s Health Care. 2019;8(4):1–9. [Google Scholar]
- 25. Belayneh F, Abreha S, Meskele M. Knowledge, attitude and factors associated with the use of long acting and permanent contraceptive methods among women of reproductive age in Gesuba Town, Southern Ethiopia. J Biology Agricult Healthcare. 2015;5(21):15–22. [Google Scholar]
- 26. Ontiri S, Ndirangu G, Kabue M, Biesma R, Stekelenburg J, Ouma C. Long-acting reversible contraception uptake and associated factors among women of reproductive age in rural Kenya. Int J Environ Res Public Health. 2019;16(9):1543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kungu W, Khasakhala A, Agwanda A. Use of long-acting reversible contraception among adolescents and young women in Kenya. PLoS One. 2020;15(11):e0241506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Anguzu R, Sempeera H, Sekandi JN. High parity predicts use of long-acting reversible contraceptives in the extended postpartum period among women in rural Uganda. Contracept Reprod Med. 2018;3:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Bhandari R, Pokhrel KN, Gabrielle N, Amatya A. Long acting reversible contraception use and associated factors among married women of reproductive age in Nepal. PLoS One. 2019;14(3):e0214590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Okafor II. Uptake of long-acting reversible contraceptive methods in Enugu State University Teaching Hospital Enugu, South-East, Nigeria. Divers Equal Health Care. 2016;13(3). [Google Scholar]
- 31. Kabalo MY. Utilization of reversible long acting family planning methods among married 15-49 years women in Areka town, Southern Ethiopia. Int J Sci Rep. 2016;2(1):1–6. [Google Scholar]
- 32. Gultie T, Hailu D, Workineh Y. Predictors of long acting contraceptives utilization among reproductive age women in Arba Minch Zuria district, Ethiopia. Qual Prim Care. 2016;24(1):17–22. [Google Scholar]
- 33. Bewket Zeleke L, Gella MM, Almaw Derseh H, Alemu AA, Abebe Kassahun E, Gelaw KA. Utilization of long-acting contraceptive methods and associated factors among female health care providers in east gojjam zone, Northwest Ethiopia, in 2018. BioMed Res Int. 2019;2019:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Kungu W, Khasakhala A, Agwanda A. Trends and factors associated with long-acting reversible contraception in Kenya. PLoS One. 2020;15(11):e0241506. [DOI] [PMC free article] [PubMed] [Google Scholar]