Abstract
Summary: Venous fenestrations are a rarely seen entity in the neck. Although their clinical significance is questionable, their importance in presurgical planning may be considerable. We present a report of two cases of internal jugular vein fenestration.
Fenestrations, or complete divisions of vasculature, have been described in many of the craniocervical arteries. One postmortem study has shown that as many as 6% of people have a fenestrated basilar artery (1). Arterial fenestrations have been described in the vertebral artery, the basilar artery, the middle cerebral artery, the anterior cerebral artery, the posterioinferior cerebellar artery, the posterior cerebral artery, the posterior communicating artery, and the internal carotid artery. Although multiple craniocervical arterial fenestrations have been described, venous fenestrations have not. Two recent cases of internal jugular vein fenestrations are described herein.
Case Reports
Patient 1
After a fall, a 62-year-old woman presented for CT angiography (CTA) to rule out vertebral artery injury. A CT scan 1 day prior revealed a fracture of the left transverse process of C4. CTA revealed no vascular injury. There was an incidental finding of a fenestrated proximal left internal jugular vein without dilatation (Fig 1).
Fig 1.
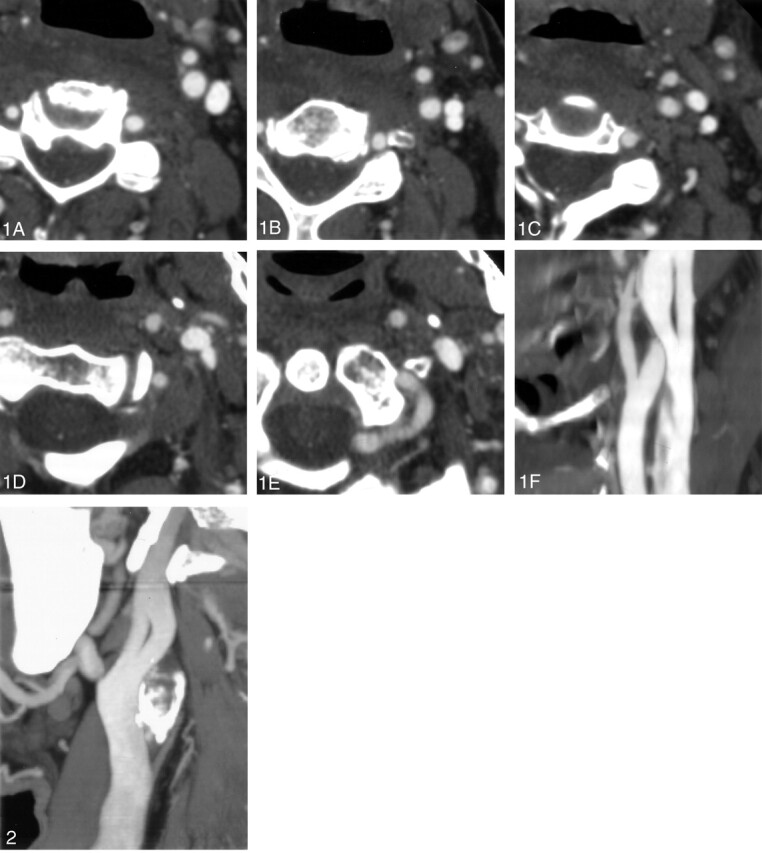
The appearance of an internal jugular vein on CTA images is characteristic. The vein begins its course with a single lumen (A, B). It then bifurcates forming two distinct lumena (C). As the vein continues caudally, it once again becomes a single vessel (D, E). Panel F shows the fenestrated internal jugular vein reformatted in a single sagittal, oblique plane.
Patient 2
After a subarachnoid hemorrhage, a 70-year-old man presented for CTA to rule out an intracranial aneurysm. CTA showed areas of moderate and severe stenosis of the proximal right internal carotid artery and complete occlusion of the proximal left internal carotid artery. A significant network of collateral arterial flow was noted. No aneurysm was observed. There was an incidental finding of a fenestrated proximal left internal jugular vein without dilatation (Fig 2).
Fig 2.
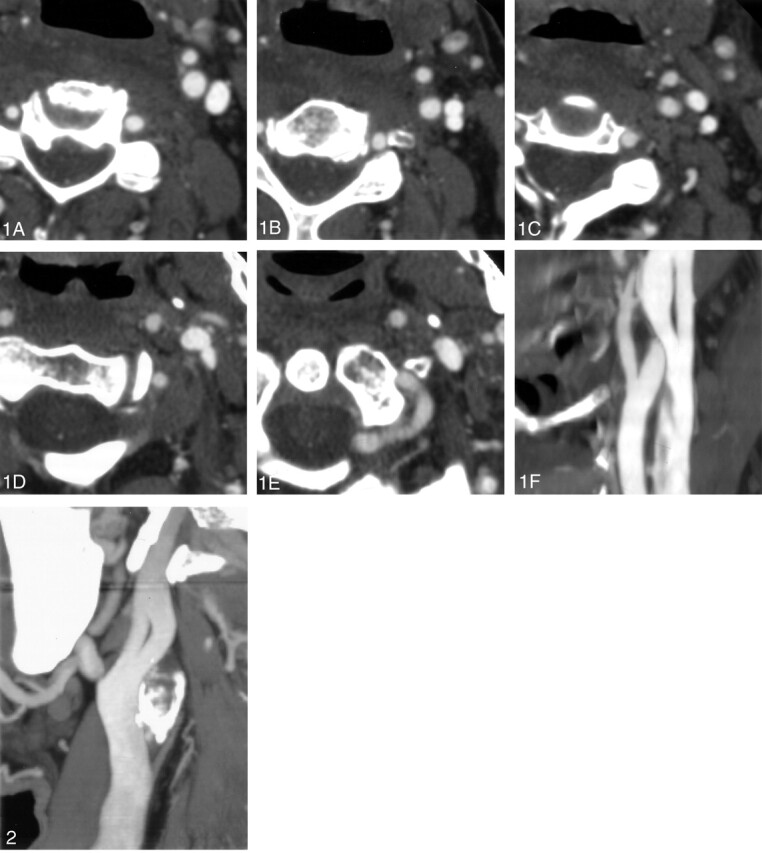
The fenestrated internal jugular vein in our second patient is seen in a single oblique plane.
Discussion
The internal jugular vein is the great collecting vein of the cranium, face, and anterior neck. It is the continuation of the sigmoid sinus beginning at the jugular foramen, where it drains most of the venous blood from the brain as well as CSF. The internal jugular vein continues inferiorly from the skull base until it joins the subclavian vein to form the brachiocephalic vein.
Fenestration of the internal jugular vein is uncommon. There have been five previously published reports of seven cases of a fenestrated internal jugular vein (2–6). One study estimated that fenestration of the internal jugular vein occurs in as much as 0.4% of the population (2).
Fenestrated arteries are associated with an increased incidence of aneurysm formation at the fenestration. As with aneurysms that tend to occur at any vessel bifurcation, the two theories that are most commonly presented to explain the association of increased incidence of aneurysm formation at fenestrations include turbulent flow at the bifurcation point and a defect in the media at both the proximal and distal branch points (7).
Fenestrated jugular veins have been associated in other reports with phlebectasia, a local fusiform dilatation (2–4). The jugular veins were not dilated in our cases. The cause of phlebectasia is unknown. There are no other anomalies associated with jugular fenestration. There is likely no clinical significance of a fenestrated jugular vein, although a detailed knowledge of anatomic variants can be helpful to the surgeon. Furthermore, an awareness that fenestrations of the jugular vein, although rare, can occur will help avoid radiologic misinterpretations or misidentifications of the vascular anatomic structures encountered in digital or conventional angiography.
References
- 1.Wollschlaeger G, Wollschlaeger PB, Lucas FV, Lopez VF. Experience and result with postmortem cerebral angiography performed as a routine procedure of the autopsy. AJR Am J Roentgenol 1967;101:68–87 [DOI] [PubMed] [Google Scholar]
- 2.Prades JM, Timoshenko A, Dumollard JM, et al. High duplication of the internal jugular vein: clinical incidence in the adult and surgical consequences, a report of three clinical cases. Surg Radiol Anat 2002;24:129–132 [DOI] [PubMed] [Google Scholar]
- 3.Som PM, Shugar JMA, Sacher M, Lanzieri CF. Internal jugular vein phlebectasia and duplication: CT features. J Comput Assist Tomogr 1985;9:390–392 [DOI] [PubMed] [Google Scholar]
- 4.Rossi A, Tortoni-Donati P. Internal jugular vein phlebectasia and duplication: case report with magnetic resonance angiography features. Pediatr Radiol 2001;31:134. [DOI] [PubMed] [Google Scholar]
- 5.Sylaidis P, Bardsley A, Montgomery P. Duplication of the internal jugular vein [letter]. Arch Otolaryngol Head Neck Surg 1997;123:1358. [DOI] [PubMed] [Google Scholar]
- 6.Zukschwerdt L. Seltene lokalisation einer venektasie. Dtsch Z Chir 1929;216:283–285 [Google Scholar]
- 7.Sanders WP, Sorek PA, Mehta BA. Fenestration of intracranial arteries with special attention to associated aneurysms and other anomalies. AJNR Am J Neuroradiol 1993;14:675–680 [PMC free article] [PubMed] [Google Scholar]


