Abstract
BACKGROUND AND PURPOSE: Some cerebral aneurysms that have been coiled reopen over time and additional treatment should be considered to reduce the risk of recurrent hemorrhage. Our purpose was to assess procedural complications and angiographic results of additional coiling in patients with previously coiled but reopened aneurysms and to evaluate protection against (re)bleeding.
METHODS: We compared procedural complications of initial coiling of 488 aneurysms in 439 patients with those of 53 additional coiling procedures in 41 reopened aneurysms in 40 patients. Angiographic results of additional coiling were assessed. We compared episodes of (re)bleeding in patients with complete or near-complete aneurysm occlusion after additional coiling with those of patients with incomplete aneurysm occlusion at 6-month follow-up angiography who were not additionally treated or who still had incomplete occlusion after additional coiling.
RESULTS: Thirty-five procedural complications occurred in 488 initial coiling procedures, and no complications occurred in 53 additional procedures. Complete or near-complete angiographic occlusion after additional coiling was obtained in 31 (76%) of 41 aneurysms. Rebleeding occurred in two of 29 patients with incomplete aneurysm occlusion but in none of the 31 patients with complete or near-complete occlusion after additional coiling.
CONCLUSION: Additional coiling of previously coiled aneurysms has a low procedural complication rate and leads to sufficient occlusion in most aneurysms. The data indicate that successful additional coiling decreases the risk of rebleeding.
Endovascular treatment with detachable coils is a safe and effective treatment for cerebral aneurysms (1–3). Main concerns of this treatment are the fate of aneurysms not completely occluded in the initial procedure and the possibility of reopening of the lumen of the aneurysm over time, which expose the patient to the risk of recurrent hemorrhage (3–5). In aneurysms that have become partially occluded, additional endovascular or surgical therapy can be considered. In this study, we assessed procedural complications and angiographic results of additional coiling in patients with previously coiled but reopened aneurysms and evaluated protection against rebleeding episodes.
Methods
Patients and Data
Between November 1994 and August 2002, 488 aneurysms in 439 consecutive patients were coiled. A total of 359 patients with 400 aneurysms underwent follow-up angiography at a median of 6 months. Eighty patients with 88 aneurysms did not undergo follow-up angiography for the following reasons: 1) Forty-four patients had 50 aneurysms and died (procedural death in 10 patients with 11 aneurysms, sequelae of subarachnoid hemorrhage [SAH] in 27 patients with 28 aneurysms, and unrelated death in seven patients with 11 aneurysms), 2) seven patients had seven aneurysms and underwent surgical clip placement or parent-vessel occlusion after incomplete initial coiling, and 3) 29 patients had 31 aneurysms and declined follow-up angiography.
Angiographic results of 359 patients with 400 aneurysms at 6-month follow-up were dichotomized into those with complete or near-complete occlusion (90–100%) and those with incomplete occlusion (<90%). At follow-up, 73 of 400 aneurysms were incompletely occluded. Four aneurysms were additionally treated with parent vessel balloon occlusion, and three, with surgical clip placement. In 25 of the remaining 66 aneurysms, no additional therapy was performed for the following reasons: One patient declined further therapy, eight were older than 70 years, three were in poor clinical condition, and second coiling was technically impossible or had a high anticipated risk in 13. Reasons in this last group were vessels arising from the aneurysm sac in eight patients, a small lobe at the base of the aneurysm in two, an aneurysm that was too small for additional coils despite its filling with contrast agent in one, failure of electrolytic detachment of coils in one (3), and unfavorable parent-vessel geometry in one. The remaining 41 incompletely occluded aneurysms in 40 patients were additionally treated with detachable coils (Fig 1).
Fig 1.
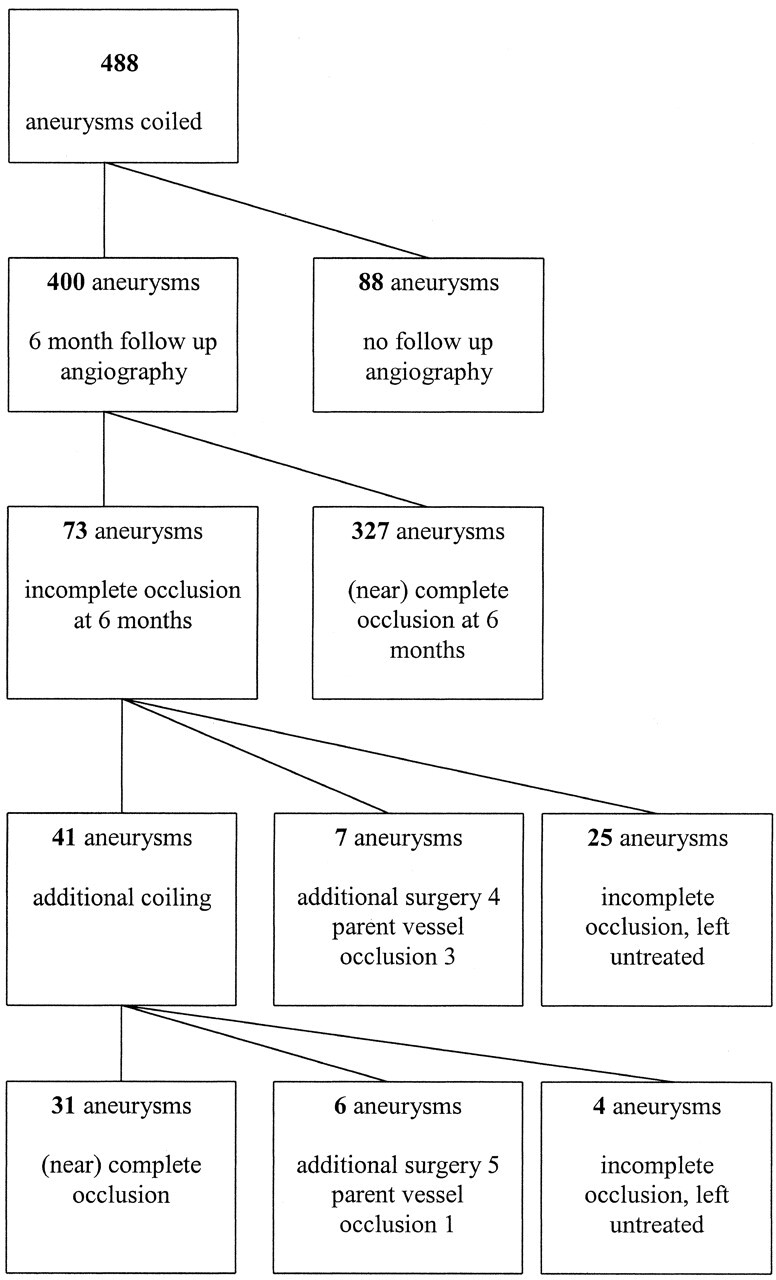
Flowchart shows angiographic results and additional treatments in 488 coiled cerebral aneurysms.
We compared baseline characteristics (sex, age, previous SAH, aneurysm size, aneurysm location, and incomplete aneurysm occlusion after initial coiling) between 327 completely or nearly completely occluded aneurysms in 291 patients with characteristics in 73 incompletely occluded aneurysms in 72 patients at 6-month follow-up angiography.
Procedural complications per treatment were defined as any complication leading to permanent neurologic deficit or death. The frequency of procedural complications during additional coiling in the 40 patients with 41 aneurysms was compared with that of first coiling in all 439 patients with 488 aneurysms. Immediate postembolization occlusion after additional coiling was dichotomized into complete or near-complete (90–100%) and incomplete (<90%) categories, as were the occlusion rates at every follow-up angiographic study after each additional coiling.
Within the group of patients with incomplete aneurysm occlusion at 6-month follow-up angiography, we compared the occurrence of episodes of (re)bleeding between patients with complete or near-complete occlusion after additional coiling and the occurrence in patients who were not additionally treated or who still had incomplete aneurysmal occlusion after additional coiling. The indication for initial coiling, particularly previous SAH, was assessed in both groups.
Internal review board approval or patient informed consent was not required for this retrospective study.
Statistical Analysis
Baseline characteristics were compared between 291 patients with 327 aneurysms and complete or near-complete occlusion and 72 patients with 73 aneurysms incompletely occluded at 6-month follow-up angiography. Sex, aneurysm rupture, location of the aneurysm, and initial incomplete angiographic results were analyzed by using the chi-squared test. Differences in median aneurysm size were analyzed by using the Mann-Whitney U test, and differences in age, by using the Student t test. P values <.05 were considered to indicate a statistically significant difference.
Procedural complication rates for initial and additional coiling were assessed and corresponding 95% CI calculated.
Rebleeding was calculated as an incidence rate. To compare the incidence of rebleeding in patients with incomplete aneurysm occlusion with that of patients with complete or near-complete occlusion after additional coiling, we calculated 95% CI with Poisson methods.
Results
The frequency of additional coiling was 41 (8.4%) of 488 coiled aneurysms.
The Table lists the baseline characteristics of the patients and aneurysms at 6-month follow-up angiography. Of the 327 completely or nearly completely occluded aneurysms, 229 (70%) had previously ruptured versus 50 (68%) aneurysms of 73 incompletely occluded aneurysms.
Characteristics of patients and aneurysms at 6-month follow-up angiography
| Complete or Near-Complete Occlusion | Incomplete Occlusion | P value | |
|---|---|---|---|
| No. of patients | 291 | 72 | NA |
| No. of aneurysms | 327 | 73 | NA |
| Men/Women | 81/210 (28/72) | 27/45 (38/62) | .13 |
| Mean age ± SD | 51.2 ± 10.7 | 53.9 ± 11.9 | .06 |
| Ruptured aneurysms | 229 (70) | 50 (68) | .80 |
| Aneurysm size (mm) | <.001 | ||
| Median | 7 | 14 | |
| Range | 2–35 | 2–55 | |
| Anterior circulation | 217 (66) | 43 (59) | .23 |
| Initial incomplete embolization | 6 (2) | 16 (22) | <.001 |
Note.—Data in parentheses are percentages.
Large aneurysm size and incomplete initial occlusion were significant predictors for incomplete occlusion at 6-month follow-up. In 41 aneurysms that were coiled more than once, 53 additional coiling procedures were performed: Thirty-three aneurysms were coiled twice, four were coiled three times, and four were coiled four times. No procedure-related complications (0%) occurred in these 53 additional procedures (0%; 95% CI: 0%, 6.7%). Thirty-five procedure-related complications occurred in 488 aneurysms that were coiled for the first time (7.2%; 95% CI: 5.1%, 9.8%), including 13 procedural ruptures. At last angiographic follow-up of the 41 additionally coiled aneurysms, 31 (76%) had complete or near-complete occlusion; two patients declined follow-up angiography after second coiling, and one patient was scheduled for follow-up angiography. Ten aneurysms (24%) were incompletely occluded. In total, 59 follow-up angiographic studies were performed after last coiling for a mean follow-up of 15.1 months (median, 6 months; range, 6–71 months). Of the 10 incompletely occluded aneurysms, five aneurysms (in four patients) were coiled, and one was treated with parent-vessel occlusion. Four of these 10 aneurysms (in four patients) were left untreated.
Clinical follow-up of the 31 patients with completely or nearly completely occluded aneurysms after additional coiling totaled 1393 months after additional coiling (median, 45 months; range, 7–96 months). Twenty (65%) of 31 aneurysms had initially ruptured, and 11 had not; two were additional aneurysms, five aneurysms presented with symptoms of mass effect, three were truly incidental aneurysms, and one aneurysm was coiled after failed surgery. Completely or nearly completely occluded aneurysms had a mean size of 18.6 mm (median, 16 mm; range 2–35, mm).
Clinical follow-up of the 25 patients with an incomplete occlusion that were left untreated and the four patients with incomplete occlusion after additional coiling was 791 months (median, 22 months; range, 1–90 months).
Among incompletely occluded aneurysms, 23 (79%) had initially ruptured, and six had not. Two aneurysms were additional aneurysms, three presented with symptoms of mass effect, and one was truly incidental. The mean size of the incompletely occluded aneurysms was 12.6 mm (median, 11 mm; range, 2–35 mm).
During follow-up, no rebleeding occurred over 116 person years (0%; 97.5% CI 0%, 3.2%) in patients with complete or near-complete occlusion after additional coiling. Two episodes of rebleeding occurred over 66 person years (3.0%; 95% CI 0.4%, 10.9%) in patients with incompletely occluded aneurysms.
Discussion
Additional coiling in reopened aneurysms after initial coiling carries a low risk of complications and leads to satisfactory aneurysm occlusion in most patients. Moreover, we found no episodes of (re)bleeding after additional coiling, whereas rebleeding did occur in patients with reopened aneurysms that were not treated further.
We did not observe any complications of additional coiling. This finding is partially explained by inclusion bias: aneurysms with a highly anticipated risk of a second coiling were not selected for additional coiling. A further explanation is that the risk of procedural rupture is low for additional coiling; the delay between a presenting SAH and second coiling is usually more than 6 months, and the risk of procedural rupture is then lower than in recently ruptured ones (6,7). Moreover, aneurysms that were additionally coiled were generally large, and the risk of procedural rupture in large aneurysms is lower than that of small aneurysms (7). Another factor accounting for the low risk of procedural rupture of aneurysms during recoiling may have been that much of the confines of the space to be catheterized and coiled were metal.
Additional coiling procedures led to a satisfactory occlusion in most patients, but in many of these patients, two or more additional coiling procedures were needed. The proportion of patients undergoing additional coiling in our study is in concordance with that of previous studies (3,5,8,9). Large aneurysmal size and incomplete initial occlusion were risk factors for incomplete occlusion at 6-month follow-up angiography, as reported in previous studies (3,4,8,10,11). Our results show that in approximately 10% of patients, coiling of an aneurysm is not a once-only procedure, but rather, a phased treatment. This phasing of treatment implies that when the angiographic results of coiling are considered, follow-up should be extended beyond the initial 6 months, as additional coiling leads to a higher proportion of completely or nearly completely occluded aneurysms.
After additional coiling, we did not observe any episode of bleeding from aneurysms with complete or near-complete occlusion. However, episodes of bleeding did occur in the patients with incompletely occluded aneurysms. The proportion of patients with ruptured aneurysms was slightly higher in this group than in those with complete or near-complete occlusion after additional coiling. Intuitively, the risk of bleeding seems higher in the group with previously ruptured aneurysms than in patients with unruptured aneurysms. However, our period for assessing risk of bleeding started at least 6 months after the onset of SAH, and from that stage on, the risk of bleeding of previously ruptured aneurysms is low. Completely or nearly completely occluded aneurysms were larger than the incompletely occluded aneurysms. Because size is the most important risk factor for bleeding of aneurysms, the prior likelihood of rupture after additional coiling based on size alone is increased for completely occluded aneurysms. However, bleeding did not occur in this group. Because the frequency of late rebleeding is low, large numbers of patients and many follow-up years are needed for a sound assessment of the effectiveness of additional coiling in preventing rebleeding. Although we studied a large number of patients undergoing additional coiling, CIs were still wide, and no definitive conclusion could be drawn. Nevertheless, the absence of rebleeding in a large series of additionally coiled patients with sufficient aneurysmal occlusion—combined with rebleeding in patients with reopened aneurysms not additionally treated and other observations that rebleeding occurs exclusively in incompletely occluded aneurysms (3,12–16)—indicates that additional coiling decreases the risk of further bleeding.
Conclusion
The low procedural risk, the favorable angiographic results, and the decreased rate of rebleeding are all factors in favor of additional coiling of reopened aneurysms in carefully selected patients
References
- 1.Brilstra EH, Rinkel GJ, van der Graaf Y, van Rooij WJ, Algra A. Treatment of intracranial aneurysms by embolization with coils: a systematic review. Stroke 1999;30:470–476 [DOI] [PubMed] [Google Scholar]
- 2.Molyneux A, Kerr R, Stratton I, et al. International Subarachnoid Aneurysm Trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised trial. Lancet 2002;360:1267–1274 [DOI] [PubMed] [Google Scholar]
- 3.Sluzewski M, van Rooij WJ, Rinkel GJ, Wijnalda D. Endovascular treatment of ruptured intracranial aneurysms with detachable coils: long term clinical and serial angiographic results. Radiology 2003;227:720–724 [DOI] [PubMed] [Google Scholar]
- 4.Byrne JV, Sohn MJ, Molyneux AJ, Chir B. Five-year experience in using coil embolization for ruptured intracranial aneurysms: outcomes and incidence of late rebleeding. J Neurosurg 1999;90:656–663 [DOI] [PubMed] [Google Scholar]
- 5.Cognard C, Weill A, Castaings L, Rey A, Moret J. Intracranial berry aneurysms: angiographic and clinical results after endovascular treatment. Radiology 1998;206:499–510 [DOI] [PubMed] [Google Scholar]
- 6.Cloft HJ, Kallmes DF. Cerebral aneurysm perforations complicating therapy with Guglielmi detachable coils: a meta-analysis. AJNR Am J Neuroradiol 2002;23:1706–1709 [PMC free article] [PubMed] [Google Scholar]
- 7.Sluzewski M, Bosch JA, van Rooij WJ, Nijssen PCG, Wijnalda D. Rupture of intracranial aneurysms during treatment with Guglielmi detachable coils: incidence, outcome, and risk factors. J Neurosurg 2001;94:238–240 [DOI] [PubMed] [Google Scholar]
- 8.Sluzewski M, Menovsky T, van Rooij WJ, Wijnalda D. Coiling of very large or giant cerebral aneurysms: long-term clinical and serial angiographic results. AJNR Am J Neuroradiol 2003;24:257–262 [PMC free article] [PubMed] [Google Scholar]
- 9.Cognard C, Weill A, Spelle L, et al. Long-term angiographic follow-up of 169 intracranial berry aneurysms occluded with detachable coils. Radiology 1999;212:348–356 [DOI] [PubMed] [Google Scholar]
- 10.Gruber A, Killer M, Bavinzski G, Richling B. Clinical and angiographic results of endosaccular coiling treatment of giant and very large intracranial aneurysms: a 7-year, single-center experience. Neurosurgery 1999;45:793–803 [DOI] [PubMed] [Google Scholar]
- 11.Kim SJ, Choi IS. Midterm outcome of partially thrombosed intracranial aneurysms treated with Guglielmi detachable coils. Intervent Neuroradiol 2000;6:13–18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Byrne JV, Molyneux AJ, Brennan RP, Renowden SA. Embolisation of recently ruptured intracranial aneurysms. J Neurol Neurosurg Psychiatry 1995;59:616–620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Graves VB, Strother CM, Duff TA, Perl J. Early treatment of ruptured aneurysms with Guglielmi detachable coils: effect on subsequent bleeding. Neurosurgery 1995;37:640–647 [DOI] [PubMed] [Google Scholar]
- 14.Malisch TW, Guglielmi G, Vinuela F, et al. Intracranial aneurysms treated with the Guglielmi detachable coil: midterm clinical results in a consecutive series of 100 patients. J Neurosurg 1997;87:176–183 [DOI] [PubMed] [Google Scholar]
- 15.Moret J, Pierot L, Boulin A, Castaings L, Rey A. Endovascular treatment of anterior communicating artery aneurysms using Guglielmi detachable coils. Neuroradiology 1996;38:800–805 [DOI] [PubMed] [Google Scholar]
- 16.Raymond J, Roy D. Safety and efficacy of endovascular treatment of acutely ruptured aneurysms. Neurosurgery 1997;41:1235–1245 [DOI] [PubMed] [Google Scholar]


