Abstract
Summary: A new, very compliant remodeling balloon microcatheter has been developed for the treatment of difficult wide-neck intracranial aneurysms (eg, arterial bifurcation or small artery aneurysms). We report selective embolization by the use of the remodeling technique with the HyperForm balloon in 16 consecutive patients with a wide-neck intracranial aneurysm located on an arterial bifurcation or a small artery or both.
Endovascular treatment of intracranial aneurysms by endosaccular coiling has become an accepted alternative to surgical clipping (1). In cases of wide-neck aneurysms, selective embolization is difficult because of the risk of coil protrusion into the parent vessel. Several authors (2–6) have reported successful treatment of these aneurysms by using the “remodeling technique ” (2). A small balloon-occlusion microcatheter is used to protect the parent artery lumen during coil deployment within the lesion. In the case of intracranial aneurysms located on arterial bifurcations or small arteries, however, the standard remodeling technique remains challenging. Baldi et al (7) recently reported the use of a new, more compliant balloon (HyperForm, Micro Therapeutics, Irvine, CA) for the treatment of difficult aneurysms and showed the feasibility of this technique. We report our experience with selective embolization of 16 consecutive wide-neck intracranial aneurysms—located on an arterial bifurcation or a small artery or both—by use of the remodeling technique with the HyperForm balloon microcatheter.
Technique
Between September 2002 and September 2003, 146 patients with 162 aneurysms were treated by the endovascular approach in our department. In 35 patients with 36 aneurysms, the aneurysmal neck size was more than 4 mm or the neck-sac ratio was more than 0.7. Of them, 19 patients (with 20 aneurysms) had aneurysms located on the carotid siphon and were excluded from the present series, because they were treated with another balloon (HyperGlide, Micro Therapeutics). The remaining 16 patients were treated by use of the HyperForm balloon for a wide-neck aneurysm located on an arterial bifurcation and/or a small artery, including nine patients for a ruptured aneurysm. Locations of the aneurysms were as follows: five on the basilar artery (BA), three on the anterior cerebral artery origin (ACA), two on the anterior communicating artery (AcomA), two on the middle cerebral artery (MCA) bifurcation, one on the ACA-MCA bifurcation, one on the distal posterior communicating artery (PcomA), one on the posterior cerebral artery (PCA), and one on the posterior and inferior cerebellar artery (PICA). All endovascular procedures were performed under general anesthesia and systemic heparinization. All patients were treated by selective embolization with Guglielmi detachable coils (GDCs). The technique of the GDC procedure has been published elsewhere (8,9). To avoid coil protrusion into the parent vessel, a HyperForm balloon was placed with its Xpedion guidewire (Micro Therapeutics) in front of the aneurysm neck under road mapping. When a normal artery was located next to the aneurysm neck, the balloon was positioned at the origin of this artery, to protect it. When catherization difficulties were encountered during balloon navigation, two types of guidewires were used and then exchanged with the Xpedion wire for inflation: the Transend 0.010-inch wire (Target Therapeutics, Fremont, CA) and the Agility 0.010-inch wire (Cordis, Miami Lakes, FL). For endosaccular coiling, another microcatheter was placed in the aneurysmal sac and coils were then deployed while the balloon was inflated temporarily. Patients were evaluated by angiography to document aneurysm obliteration. Angiographic results were classified as complete occlusion (no contrast material filling the aneurysmal sac), neck remnant (residual contrast material filling the aneurysmal neck), and residual flow (residual contrast filling the aneurysmal body). A senior neurosurgeon recorded the clinical course, including worsening of symptoms and death, at 3 months after the treatment. Clinical outcome was graded according to a modified Glasgow outcome scale (10), as follows: excellent (neurologically intact); good (mild hemiparesis, cranial nerve palsy, or other deficit that does not interfere with daily functioning or work); fair (significant hemiparesis, aphasia, confusion, or other deficit that interferes with daily activities or prevents a return to work); and poor (coma or severe neurologic deficit rendering the patient dependent on family or nursing staff).
Results
Selective embolization was successfully performed in 15 of 16 patients and resulted in 15 excellent clinical outcomes. In most cases, the HyperForm balloon microcatheter was easily positioned with its guidewire in front of the aneurysm neck. In four patients, however, we failed to position the balloon, and a stiffer microguidewire (Transend 0.010 inch [Target] or Agility 0.010 inch [Cordis]) was required to place it optimally. In these patients, aneurysms were located on the MCA bifurcation in two cases, the PICA in one, and the AcomA in one. In all cases, the HyperForm balloon appeared very stable while inflated and bulged into arterial bifurcation to optimally seal the aneurysm neck (Fig 1). Neither thromboembolic complication nor arterial dissection, rupture, or spasm occurred in the present series during balloon inflation.
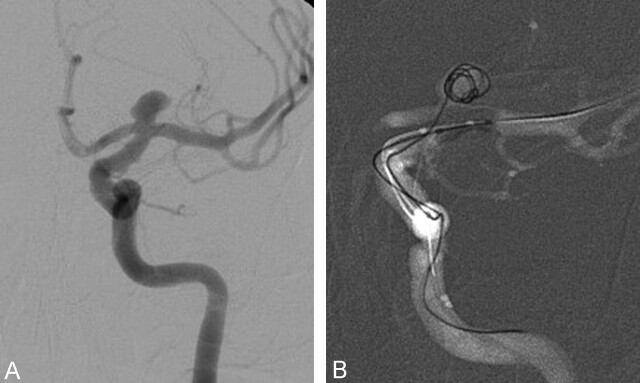
Fig 1.
Incidental aneurysm in a 43-year-old woman.
A, Left ICA angiogram shows a wide-neck ICA bifurcation aneurysm.
B, The Hyper Form balloon microcatheter is placed at the middle cerebral artery origin. Road-mapping during cell deployment shows the Hyper Form balloon bulging into the ICA bifurcation to optimally seal the aneurysm neck.
In one 39-year-old male patient with a 3 × 3 mm ruptured AcomA aneurysm, the deployment of the third coil resulted in the extrusion of the first two coils into the ACA when the balloon was deflated. We attempted to retrieve the coils with a lasso but failed because of catheterization difficulties. The patient was treated by surgical clipping 24 hours later and kept a significant hemiparesis. Angiographic results in 15 patients consisted of 13 complete occlusions and two neck remnants.
Discussion
Several authors (2–6) have reported on the feasibility and efficacy of balloon-assisted coiling in wide-neck intracranial aneurysms. Most of their treated lesions, however, were internal carotid artery (ICA) sidewall aneurysms and were treated with standard oval guide-dependent balloons. In our department, wide-neck aneurysms of the ICA are treated with the HyperGlide balloon microcatheter: this low-compliance balloon is indicated for sidewall aneurysms but does not have the propensity to adapt to the anatomy of arterial bifurcation because it does not bulge through the aneurysm neck. Baldi et al (7) recently reported four bifurcation aneurysms treated with the HyperForm balloon. This new, very compliant balloon has the advantage to change easily from its cylindrical shape to bulge into the origin of the arterial bifurcation and seal the aneurysm neck (Fig 1). Because of its Xpedion microguidewire, the HyperForm balloon is also very stable while inflated, compared with round balloons that are not guide dependent. Another advantage of its great suppleness and compliance is that the HyperForm balloon can be used in small arteries (eg, PICA, PCA, AcomA, etc). Indeed, the balloon-assisted technique has proved to be effective and safe (2–6), although it may increase risks of aneurysm or vessel rupture (11). To avoid these complications, precise control of balloon placement and inflation is mandatory and is facilitated by the technical properties of the HyperForm balloon. Our series confirms these findings and suggests that it is possible to treat wide-neck aneurysms located on small arteries or arterial bifurcations by selective embolization.
In our department, patient selection criteria for the remodeling technique with the HyperForm balloon mainly include wide-neck aneurysms located on bifurcations or small arteries of the circle of Willis. Wide-neck intracranial aneurysms that are not located on the ICA are treated with the HyperForm balloon microcatheter.
During endovascular procedures, some catheterization difficulties may be encountered with the HyperForm balloon because of the low stiffness of its microguidewire (Xpedion, Micro Therapeutics). In four cases (MCA bifurcation aneurysms in two cases, PICA in one, and AcomA in one), we used other, 0.010-inch, wires for better navigability. Thus, in case of intracranial arterial anatomy, including tortuosities or acute angles, a stiffer microguidewire may be useful. Nevertheless, after catheterization, the guidewire is exchanged and the Xpedion wire must be used to close the inner lumen of the HyperForm catheter to allow for balloon inflation and deflation.
Complications associated with the balloon-assisted technique include a higher rate of thromboembolic events (12) and increased risks of aneurysm or vessel rupture (11). None of these complications occurred in our series. The risk of delayed coil herniation into the parent vessel must also be considered, because it occurred in one of our patient. This patient had a ruptured 3 × 3 mm AcomA aneurysm involving the second segment of the left ACA. We tried to place the HyperForm balloon via the right ICA to have the best anatomic balloon position to seal the neck, but we failed. The remodeling balloon was thus positioned in the AcomA and the right ACA without completely sealing the aneurysm neck. After placement of the first two coils, a stable conformation of coils did not occur that may explain the extrusion of coils during deployment of the third one. In such a case when the balloon cannot be positioned optimally, it may be better to stop the procedure and refer the patient to a neurosurgeon.
Conclusion
This series shows that the HyperForm balloon microcatheter is a very useful tool for the treatment of difficult wide-neck intracranial aneurysms. It supports the conclusions drawn by Baldi et al (7) that the HyperForm balloon allows treatment of wide-neck intracranial aneurysms located on arterial bifurcations or small arteries. Further studies with long-term follow-up will be necessary to better define the place of this new balloon in the therapeutic armamentarium of complex cerebral aneurysms.
References
- 1.International Subarachnoid Aneurysm Trial (ISAT) Collaborative Group. ISAT of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomized trial. Lancet 2002;360:1267–1274 [DOI] [PubMed] [Google Scholar]
- 2.Moret J, Cognard C, Weill A, et al. The “remodeling technique” in the treatment of wide neck intracranial aneurysms. Intervent Neuroradiol 1997;3:21–35 [DOI] [PubMed] [Google Scholar]
- 3.Lefkowitz MA, Gobin YP, Akiba Y, et al. Balloon-assisted Guglielmi detachable coiling of wide-necked aneurysms. II. Clinical results. Neurosurgery 1999;45:531–536 [DOI] [PubMed] [Google Scholar]
- 4.Aletich VA, Debrun GM, Misra M, et al. The remodeling technique of balloon-assisted Guglielmi detachable coil placement in wide-necked aneurysms: experience at the University of Illinois at Chicago. J Neurosurg 2000;93:388–396 [DOI] [PubMed] [Google Scholar]
- 5.Nelson PK, Levy DI. Balloon-assisted coil embolization of wide-necked aneurysms of the internal carotid artery: medium-term angiographic and clinical follow-up in 22 patients. AJNR Am J Neuroradiol 2001;22:19–26 [PMC free article] [PubMed] [Google Scholar]
- 6.Cottier JP, Pasco A, Gallas S, et al. Utility of balloon-assisted Guglielmi detachable coiling in the treatment of 49 cerebral aneurysms: a retrospective, multicenter study. AJNR Am J Neuroradiol 2001;22:345–351 [PMC free article] [PubMed] [Google Scholar]
- 7.Baldi S, Mounayer C, Piotin M, et al. Balloon-assisted coil placement in wide-neck bifurcation aneurysms by use of a new, compliant balloon microcatheter. AJNR Am J Neuroradiol 2003;24:1222–1225 [PMC free article] [PubMed] [Google Scholar]
- 8.Gulielmi G, Vinuela F, Dion J, Duckwiler G. Electrothrombosis of saccular aneurysms via endovascular approach. Part 2. Preliminary clinical experience. J Neurosurg 1991;75:8–14 [DOI] [PubMed] [Google Scholar]
- 9.Guglielmi G, Vinuela F, Duckwiler G, et al. Endovascular treatment of posterior circulation aneurysms by electrothrombosis using electrically detachable coils. J Neurosurg 1992;77:515–524 [DOI] [PubMed] [Google Scholar]
- 10.Jennett B, Bond M. Assessment of outcome after severe brain damage: a practical scale. Lancet 1975;1:480–484 [DOI] [PubMed] [Google Scholar]
- 11.Phatouros CC, Halbach VV, Malek AM, et al. Simultaneous subarachnoid hemorrhage and carotid cavernous fistula after rupture of a paraclinoid aneurysms during balloon-assisted coil embolization. AJNR Am J Neuroradiol 1999;20:1100–1102 [PMC free article] [PubMed] [Google Scholar]
- 12.Soeda A, Sakai N, Sakai H, et al. Thromboembolic events associated with Guglielmi detachable coil embolization of asymptomatic cerebral aneurysms: evaluation of 66 consecutive cases with use of diffusion-weighted MR imaging. AJNR Am J Neuroradiol 2003;24:127–132 [PMC free article] [PubMed] [Google Scholar]