Abstract
BACKGROUND AND PURPOSE: Mechanical disruption of a clot with a microcatheter and a guidewire has not been detailed in conjunction with intra-arterial thrombolysis in patients with acute ischemic stroke. The purpose of this study was to evaluate the efficacy of mechanical disruption of an embolus in the carotid artery distribution.
METHODS: We analyzed clinical and radiologic findings and functional outcomes 3 months after thrombolysis with mechanical disruption. Outcomes were classified as good for modified Rankin scale (mRS) scores of 0–2, moderate for mRS scores of 3, and poor for death and mRS scores of 4 or 5.
RESULTS: Twenty-three consecutive patients with severe hemispheric symptoms were treated with several methods of mechanical embolus disruption during the intra-arterial administration of urokinase. Twelve patients had occlusions of the proximal middle cerebral artery (MCA), and 11 had occlusions of the distal internal carotid artery (ICA). Recanalization was observed in all patients with MCA occlusions and in 10 (91%) with ICA occlusions. Outcomes were good in nine patients (75%) with MCA occlusions and in four (36.4%) with ICA occlusions. Early management of vessel perforation, caused by a microguidewire tip in two patients, resulted in early hemostasis. Neither patient had a major deficit attributable to the complication.
CONCLUSION: A high incidence of recanalization and clinical improvement can be observed in patients with occlusions of not only the proximal MCA but also the distal ICA. This method might be an effective additional option to intra-arterial thrombolysis for acute distal ICA and proximal MCA occlusions.
The effectiveness of intra-arterial thrombolytic therapy for acute middle cerebral artery (MCA) occlusion has been demonstrated in many reports, including several randomized controlled studies (1–3). The reported rates of recanalization and favorable outcomes with intra-arterial thrombolytic therapy depend on various factors such as the technical approach, thrombolytic agent, occlusion site, and clot volume. Various techniques have been reported for the administration of fibrinolytic agents (ie, continuous infusion; pulse spray; and via the catheter tip within, distal to, or proximal to the clot), and assisted methods of mechanical disruption include use of a microcatheter, guidewire, balloon catheter, or snare (4–8). Mechanical disruption with a microcatheter and a guidewire, which are available during ordinary intra-arterial thrombolysis without special preparation (as with balloon catheters), might facilitate pharmacologic thrombolysis by fragmenting the clot and increasing the surface area exposed to lytic agents. This method appears to be effective for improving the rate of recanalization. However, to our knowledge, no reports have described in detail how to use the microcatheter and the guidewire for the mechanical disruption of clots. The final goal of thrombolytic therapy in acute stroke is the rescue of brain tissue from ischemic damage to preserve neuronal function. In theory, the most important step in this therapeutic strategy is recanalization of occluded intracranial arteries to restore cerebral blood flow (9). The rate of recanalization should be improved to prevent severe disability and death, especially in patients with embolic occlusion of the distal internal carotid artery (ICA) and the proximal MCA. Failure of recanalization frequently results in fatal outcomes.
We used several techniques to mechanically disrupt clots by using a microcatheter and a guidewire during intra-arterial thrombolysis. The purpose of this study was to assess the efficacy and safety of these techniques in patients with embolic occlusion of major arteries in the carotid territory. To our knowledge, this is the first report to describe practical methods of mechanical disruption by using a microcatheter and a guidewire in an attempt to increase the likelihood of arterial recanalization.
Methods
Our inclusion criteria on admission for intra-arterial thrombolytic therapy in this study were as follows: sudden-onset severe hemiparesis, arrival to our hospital within 4 hours of stroke onset, and patient age less than 85 years. Clinical exclusion criteria were the following: critical systemic condition or serious disabling disease, recent surgery, and known bleeding tendency. The patient’s initial neurologic examination was rated by using the National Institutes of Health Stroke Scale (NIHSS) (10), which was not used in the inclusion or exclusion criteria.
CT scanning was performed in all patients. Exclusion criteria for CT scanning were evidence of any intracranial hemorrhage and early, clear hypoattenuation. All patients were initially treated with hypervolemic therapy (250 mL of a colloid solution) and heparin (3000-U bolus). MR imaging, diffusion-weighted (DW) imaging, and MR angiography were performed to evaluate early ischemic changes, occlusion sites, and collateral flow via the circle of Willis. Patients were excluded when the hyperintense area on DW images was larger than half of the affected vessel territory or when MR angiograms demonstrated no occlusion of a major artery occlusion. Informed consent was obtained from family members of the patients.
Endovascular Technique
A 5F guidecatheter was placed in the ICA proximal to the occlusion site. The procedure was performed with the patient under local anesthesia, with sedatives if necessary. Digital subtraction angiography (DSA) was performed only for the affected artery. Because MR angiograms can demonstrate an outline of collateral circulation via the circle of Willis, we did not evaluate potential leptomeningeal collaterals on DSA images to avoid additional, time-consuming catheterization of the other arteries. A microcatheter (Renegade-18; Boston Scientific Corporation, Natick, MA) was introduced through the guiding catheter beyond the embolus, and local angiography from the microcatheter was performed to assess the precise site of occlusion and the size of the embolus before we initiated the procedure. Two types of guidewires were used: one with a 45°-angle tip and one with a double-angle tip (0.016-inch Radifocus GT; Terumo, Tokyo, Japan). Diluted contrast medium with a double amount of heparinized normal sodium chloride solution was used for local angiography, which was performed under fluoroscopy to evaluate the state of the arteries and emboli after each maneuver. The microcatheter and microguidewire were manipulated under fluoroscopic observation to avoid vascular damage.
The mechanical disruption techniques shown in Figure 1 were applied until the embolus was dislodged into the distal arteries. In each case, the primary surgeon selected a technique at his or her discretion. As a guideline, injection of the urokinase solution was performed first. If the dose of urokinase was close to the maximal limit, heparinized normal sodium chloride solution was injected. Then, mechanical disruption was undertaken by moving the microcatheter over the guidewire. If occlusion persisted after these procedures, mechanical disruption was performed by moving a J-shaped guidewire tip and by rotating the J-shaped guidewire tip, in this order. When the embolus was moved to the distal vessels, these procedures were repeated at the new occlusion sites in the same manner. Thrombolysis was discontinued when 1) adequate recanalization was achieved (all of the M2 and A3 segments and the M3 segment supplying to the motor area were opened), 2) extravasation of contrast material was noted at local angiography, 3) 6 hours elapsed since symptom onset, or 4) angiographic improvement was not achieved by mechanical disruption after a maximum dose of urokinase (600,000 U) had been administered.
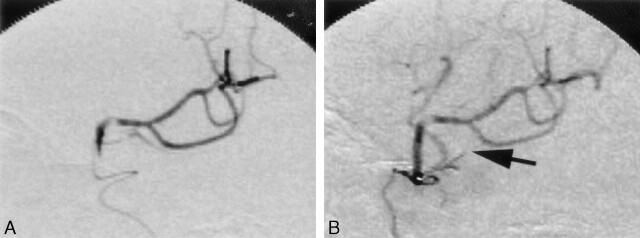
Fig 1.
Techniques of mechanical disruption. A, Microcatheter tip is advanced to the distal end of the embolus. Urokinase in 10 mL of normal or heparinized normal sodium chloride solution is manually injected into the embolus as forcefully as possible while the tip is slowly withdrawn into the proximal end of the embolus. B, Microcatheter tip is passed back and forth through the clot over a microguidewire several times. For an embolus at a bifurcation, the microcatheter is introduced into both distal arteries to disrupt clot entering them. C, Tip of a double-angled microguidewire is flexed into a J shape in the arterial lumen near the embolus and moved gently in the embolus along the vasculature several times. D, Rotation of a J-shaped guidewire tip in the embolus several times.
Forceful injection of urokinase solution in the embolus.—
A dose of 60,000 or 120,000 U of urokinase was dissolved in 10 mL of normal sodium chloride solution (prepared in 10-mL syringes) (Fig 1A). After the microcatheter was advanced into the distal end of the embolus, 10 mL of urokinase solution in a 10-mL syringe was injected into the embolus as forcefully as possible by hand while the microcatheter was slowly withdrawn to the proximal end of the embolus. For the initial three injections, a dose of 120,000 U was used. Then, 60,000 U of urokinase was injected repeatedly as needed to achieve recanalization, with the total dose limited to 600,000 U.
Forceful injection of heparinized normal sodium chloride solution in the embolus.—
Normal sodium chloride solution containing 1% heparin was injected into the embolus as forcefully as possible by hand while the microcatheter was slowly withdrawn from the distal end to the proximal end of the embolus. Injections were repeated several times.
Mechanical disruption by movement of a microcatheter over a guidewire along the vasculature.—
The embolus was disrupted by passing the microcatheter through the entire clot over a preceding guidewire (Radifocus GT guidewire, 45° tip; Terumo) several times (Fig 1B). The clot was broken mainly by the tip of the microcatheter. During catheter manipulation, contact of the guidewire tip with the vessel wall was carefully avoided to prevent vessel perforation. For an embolus at a bifurcation, advancing the microcatheter into both of the distal arteries disrupted both parts of the clot entering the distal arteries.
Mechanical disruption by movement of a J-shaped guidewire tip along the vasculature.—
The tip of the microguidewire (Radifocus GT guidewire, double-angle tip; Terumo) was formed into a J shape by manipulation in the arterial lumen close to the embolus (Fig 1C). Penetration and fragmentation of the clot was achieved by gently advancing the convex border of the J-shaped guidewire several times.
Mechanical disruption by rotation of a J-shaped guidewire tip in the embolus.—
Fragmentation of the clot was achieved by several rotations of the convex border of the J-shaped guidewire tip in the embolus (Fig 1D).
To avoid vessel perforation by the guidewire tip, repeated hand-injected local angiography from a microcatheter was performed after each maneuver to assess the state of the emboli and distal vessels. Early detection of vessel damage was also achieved by means of repeated local angiography. The guidewire was not advanced beyond the M3 segment of the MCA. To prevent hemorrhagic complications, the dose of urokinase was kept to a minimum, and intravenously administered heparin was discontinued when the procedure was complete. When adequate recanalization was achieved, we performed strict blood pressure control to <160/90 mm Hg with neither anticoagulation nor antiplatelet treatment after reperfusion therapy for at least 3 days. When extravasation was suggested by local angiography, blood pressure was controlled to <140 mm Hg systolic. The patient was then moved to the CT suite immediately after reperfusion therapy was discontinued, with the catheter sheath kept in the femoral artery. If extravasation was confirmed on CT scans, protamine sulfate was administered to reverse the heparinization, and systolic blood pressure was maintained at <140 mm Hg.
Analysis of Mechanical Disruption Techniques
All fluoroscopic monitoring procedures were recorded on videotape for later evaluation. After each reperfusion treatment, the frequency with which each mechanical disruption technique was used, the number of embolus dislodgements and cases of vessel damage, and the arterial sites of embolus were analyzed on the videotape.
Evaluation of Outcomes
Arterial recanalization was evaluated by means of DSA at the end of the thrombolytic therapy. Arteries in which DSA showed persistent occlusions were evaluated, provided that occlusion of the distal M4 segment was regarded as no occlusion.
All patients were evaluated by using the NIHSS at 24 hours and at 3 months after treatment. CT scans were obtained approximately 30 minutes after treatment. Outcomes at 3 months after treatment were assessed according to the modified Rankin scale (mRS), a disability scale on which grades are assigned with reference to the patient’s previous lifestyle; these scores ranged from 0 (absence of symptoms) to 5 (bedridden) (11). Outcomes were grouped into three categories: good for those patients who were functionally independent (mRS score, 0–2), moderate for those who were almost independent (mRS score, 3), or poor for those who had died or who were dependent (mRS score, 4–5). The first author (T.S.) performed the angiographic and outcome evaluations.
Results
Between May 2001 and March 2003, 23 consecutive patients (mean age ± SD, 73.0 ± 7.1 years; 15 men, eight women) were treated with mechanical disruption in conjunction with intra-arterial thrombolysis. The clinical characteristics of the patients are presented in Tables 1 and 2. The occlusion sites of the MCA (n = 12) were the proximal M1 segment, the distal M1 segment, and the proximal M2 segment in six patients, five patients, and one patient, respectively (Table 1). The occlusion sites of the ICA (n = 11) were the C1, C2, C3, and C4 segments in three, three, three, and two patients, respectively (Table 2). In all patients with ICA occlusion, clots extended from the intracranial part of the ICA to the MCA. The interval from the onset of symptoms to the patients’ arrival at the hospital ranged from 40 to 190 minutes (79.8 ± 45.0 minutes). The interval from their arrival to the start of angiography ranged from 30 to 60 minutes (43.0 ± 12.7 minutes). The embolic source, including atrial fibrillation, was confirmed in 22 patients. In patient 4, the guidecatheter could not be advanced to the carotid artery via the transfemoral approach, and a 4F guidecatheter was introduced through the common carotid artery by means of direct cervical puncture.
TABLE 1:
Clinical features of 12 patients with MCA occlusion
| Patient/Age(y)/Sex | Initial Occlusion Site | Urokinase Dose (U) | Time from Onset (min) | Occlusion Site after Procedure | NIHSS Score | mRS Score at 3 mo | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Admission | Start of Angiography | End of Procedure | Initial | 24 h | 3 mo | |||||
| –1/73/M | L M1 proximal | 480,000 | 40 | 70 | 210 | FM3 | 23 | 19 | 1 | 1 |
| –2/70/F | L M1 distal | 480,000 | 60 | 90 | 150 | FP M4 | 25 | 0 | 0 | 0 |
| –3/70/F | R M1 proximal | 480,000 | 60 | 90 | 160 | No | 18 | 2 | 0 | 0 |
| –4/81/F* | L M1 distal | 540,000 | 40 | 70 | 180 | FT M3 | 27 | 27 | 23 | 5 |
| –5/84/M† | L M1 proximal | 480,000 | 120 | 165 | 265 | F M3 | 25 | 17 | Dead | Dead |
| –6/66/M | L M1 proximal | 480,000 | 60 | 120 | 180 | F M4 | 25 | 2 | 3 | 1 |
| –7/70/M | R M1 distal | 360,000 | 65 | 105 | 165 | No | 16 | 1 | 0 | 0 |
| –8/74/M | L M1 proximal | 600,000 | 95 | 130 | 210 | F M3 C M4 | 20 | 13 | 13 | 4 |
| –9/74/F‡ | L M1 distal | 360,000 | 45 | 95 | 150 | P M3 | 24 | 5 | 0 | 0 |
| 10/84/M | L FP M2 proximal | 360,000 | 60 | 90 | 180 | F M3 | 25 | 19 | 9 | 2 |
| 11/78/M | R M1 proximal | 420,000 | 150 | 210 | 300 | PT M3 | 19 | 3 | 0 | 0 |
| 12/71/M | R M1 distal | 480,000 | 120 | 180 | 230 | P M4 | 19 | 5 | 0 | 0 |
Note.—C indicates central; F, frontal; P, parietal; T, temporal; M1, horizontal segment of the MCA; M2, insular segment of the MCA; M3, opercular segment of the MCA; and M4, cortical segment of the MCA.
Direct puncture.
Multiple organ failure.
Perforation.
TABLE 2:
Clinical features of 11 patients with ICA occlusion
| Patient/Age(y)/Sex | Initial Occlusion Site* | Urokinase Dose (U) | Time from Onset (min) | Occlusion Site after Procedure | NIHSS Score | mRS Score at 3 mo | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Admission | Start of Angiography | End of Procedure | Initial | 24 h | 3 mo | |||||
| 13/69/M | R C3/prox M1 | 600,000 | 60 | 120 | 240 | C M3 | 20 | 13 | 7 | 3 |
| 14/73/F | R C1/prox M1 | 420,000 | 180 | 210 | 270 | P M3 | 16 | 2 | 0 | 0 |
| 15/76/M | L C2/prox M1 | 420,000 | 40 | 70 | 150 | Angular M4 | 25 | 21 | 11 | 2 |
| 16/69/F | R C4/prox M1 | 600,000 | 120 | 150 | 240 | C4 | 19 | 11 | 7 | 3 |
| 17/82/F | L C3/mid M1 | 600,000 | 60 | 110 | 210 | Angular M4 | 28 | 25 | 24 | 5 |
| 18/66/M | R C1/mid M1 | 480,000 | 60 | 100 | 170 | No | 21 | 8 | 0 | 0 |
| 19/58/M | L C1/mid M1 | 420,000 | 50 | 80 | 150 | No | 26 | 13 | 5 | 2 |
| 20/78/F† | L C4/prox M1 | 480,000 | 190 | 240 | 300 | M2 | 26 | 18 | 14 | 3 |
| 21/83/M | L C3/distal M1 | 420,000 | 40 | 100 | 180 | Angular M4 A4 | 28 | 23 | 23 | 5 |
| 22/69/M‡ | R C2/mid M1 | 480,000 | 70 | 120 | 220 | C M4 | 17 | 13 | 11 | 4 |
| 23/61/M§ | L C2/distal M1 | 600,000 | 50 | 110 | 300 | FCM2 A4 | 29 | 28 | Dead | Dead |
Note.—A4 indicates the supracallosal segment of the anterior cerebral artery; C1, knee portion of the ICA; C2, cisternal portion of the ICA; C3, anterior knee of the ICA; C4, cavernous portion of the ICA; dist M1, distal third of the M1; prox M1, proximal third of the M1; mid M1, middle third of the M1.
Proximal end/distal end of clot.
Perforation.
L leg embolism.
Massive cerebral infarct.
NIHSS scores at the time of initial evaluation were 16 in two patients, 17 in one, 18 in one, 19 in three, 20 in two, 21 in one, 23 in one, 24 in one, 25 in five, 26 in two, 27 in one, 28 in two, and 29 in one. Initial NIHSS scores ranged from 16 to 29 (22.7 ± 4.1). All patients had severe hemispheric neurologic deficits, including hemiplegia and gaze palsy to the hemiplegic side. MR images were unavailable for two patients. The interval from the start of angiography to the completion of thrombolytic therapy ranged from 55 to 190 minutes (86.3 ± 32.1 minutes). The interval from the onset of symptoms to the completion of thrombolytic therapy ranged from 150 to 300 minutes (209.1 ± 51.0 minutes).
Analysis of the Mechanical Disruption Technique
All videotapes of the procedures were analyzed after each reperfusion treatment. Table 3 shows the frequency with which each mechanical disruption technique was used, the frequency of embolus dislodgments immediately after each technique was applied, and the arterial sites of embolus in which each technique was used. For all patients, the mechanical disruption technique was applied a mean of 19.4 times, and the embolus was moved a mean of 5.9 times (30.4%) after application of the technique. Vessel damage was observed in two cases; this was induced by movement of the microcatheter over the guidewire in one case and movement of a J-shaped guidewire in the other.
TABLE 3:
Application of mechanical disruption techniques and embolus dislodgments
| Embolus Location | Forceful Injection |
Movement of Microcatheter over Guidewire | Movement of J-shaped Guidewire Tip | Rotation of J-shaped Guidewire Tip | |
|---|---|---|---|---|---|
| Urokinase Solution | Heparinized Normal Saline | ||||
| ICA | 37/6 | 9/0 | 30/8 | 14/5 | 3/3 |
| M1 segment of MCA | 55/11 | 22/1 | 51/15 | 27/14 | 4/3 |
| M2 segment of MCA | 21/0 | 51/10 | 85/39 | 22/13 | 2/2 |
| M3 segment of MCA | 0/0 | 0/0 | 11/5 | 0/0 | 0/0 |
| Anterior cerebral artery | 1/0 | 0/0 | 1/1 | 0/0 | 0/0 |
| Total | 114/17 | 82/11 | 178/68 | 63/32 | 9/8 |
Note.—Data are the number of applications/number of embolus dislodgments.
Recanalization Rate
The occluded vessel was recanalized successfully in 22 patients, corresponding to a recanalization rate of 95.7%. For MCA and ICA occlusions, recanalization was achieved in 12 (100%) of 12 patients and in 10 (91%) of 11 patients, respectively. In all 22 patients in whom recanalization was achieved, distal migration of an embolus occurred. At the newly occluded location, we also obtained recanalization in all 22 patients, although the embolus again migrated into the further-distal arteries. In one patient with a right ICA occlusion (case 16), the procedure was discontinued without any recanalization. In this patient, the embolus extended from the C4 segment to the proximal M1 segment, as shown at initial local angiography. After 600,000 U of urokinase was injected in the embolus with the various mechanical disruption procedures, local angiography from a microcatheter in the C4 segment showed the ICA and MCA, with severe stenosis in the C2 segment. However, angiography from the guide catheter showed no filling of the ICA distal to the C4 segment. Thrombolytic therapy was discontinued, because the maximum dose of urokinase had been administered. MR angiograms demonstrated recanalization of the ICA and occlusion of the proximal M1 segment immediately after hemostasis. Twelve hours after the procedure, MR angiograms showed recanalization of the entire ICA and MCA, and the patient’s left hemiparesis moderately improved. Recanalization after the procedure might be facilitated by thrombolytic therapy.
Clinical Outcome
All 23 patients treated with mechanical disruption survived for 24 hours, but two died within 3 months. NIHSS scores at 24 hours ranged from 0 to 28 (12.5 ± 9.0), and scores at 3 months among the 21 survivors ranged from 0 to 24 (7.2 ± 8.3). The mean mRS score at 3 months among the survivors was 1.9 ± 1.9. Outcomes were good in nine patients with MCA occlusions (75%) and in four patients with ICA occlusions (36.4%).
Local angiography showed extravasation of contrast medium in two patients. In a 74-year-old woman (case 9) with a left M1 distal occlusion, the embolus was moved to the distal M2 segment during thrombolysis with mechanical disruption (movement of the microcatheter over the guidewire). Extravasation was demonstrated after mechanical disruption. This procedure also removed the embolus in the M3 segment of the parietal artery. The guidewire tip seemed to penetrate the orifice of the small artery in the wall of M2 segment. Another iatrogenic perforation occurred in the arteriosclerotic vessel wall of a 78-year-old woman (case 20) with a history of diabetes mellitus. The embolus, initially located in the left C4 segment, was moved to the distal M1 segment during thrombolysis with mechanical disruption. After several movements of a J-shaped guidewire tip through the embolus, local angiography demonstrated movement of the embolus to the M2 segment and extravasation of contrast medium. The blood pressure of both patients was controlled to <140 mm Hg systolic immediately after local angiograms showed extravasation, which was confirmed on CT scans. Protamine sulfate was administered to reverse the heparinization, and the patients’ systolic blood pressure was maintained at <140 mm Hg. In patient 9, normal-pressure hydrocephalus developed subsequent to the iatrogenic subarachnoid hemorrhage. Placement of a ventricular peritoneal shunt resolved the symptoms, and the patient was discharged home free of any neurologic deficit 2 months later. In patient 20, right hemiplegia improved gradually. She was able to walk without assistance but needed help because of her moderate aphasia and mild right hemiparesis.
Two patients (cases 5 and 23) died after thrombolytic therapy. An 84-year-old man (case 5) had total aphasia and right hemiplegia due to left M1 occlusion. Before thrombolytic therapy, no history of his illness was recognized. Thrombocytopenia (platelet count, 57,000/μL) was revealed during the procedure from the results of the emergency blood count determination on admission. The patient, who demonstrated some evidence of neurologic recovery, died secondary to multiple organ failure on post-thrombolysis day 6. A 61-year-old man (case 23) with a left C2 occlusion aspirated vomitus and oral secretions during the thrombolytic therapy, and developed aspiration pneumonia that required additional procedures, including tracheal intubation, which delayed thrombolytic therapy. The procedure was discontinued 5 hours after the onset of symptoms, although the M2 segment of the frontal and central distribution was persistently occluded. Extensive ischemic brain edema associated with cerebral infarction developed 2 days after treatment. He died of transtentorial herniation the following day.
Illustrative Case
Case 18 involved a 66-year-old, right-handed man with a history of atrial fibrillation who presented to the emergency department 60 minutes after the acute onset of drowsiness, eyeball deviation to the right side, and left hemiplegia. CT results were unremarkable, except for increased attenuation in the right MCA. Emergency DW imaging showed faintly abnormal diffusion in the right frontal and parietal lobe. MR angiograms revealed occlusion of the right ICA. Emergency angiography performed 100 minutes after the onset of symptoms confirmed the right C1 occlusion (Fig 2A). Local angiograms from the microcatheter showed the embolus extending from the ICA just distal to orifice of the posterior communicating artery to the mid-M1 segment (Fig 2C and D). During slow withdrawal of the microcatheter, 120,000 U of urokinase dissolved in 10 mL of normal sodium chloride solution was forcefully injected into the embolus by hand. This maneuver was repeated three times for total injection of 360,000 U of urokinase; however, no recanalization was achieved. An attempt to disrupt the clot with several movements of the microcatheter over a guidewire through the embolus had no effect on the occlusion. To-and-fro movements in the embolus with a J-shaped tip of a double-angle microguidewire (Fig 3A and B) resulted in no change of the occlusion. We elected to perform rotations of the J-shaped tip of the microguidewire in the embolus (Fig 2C). Local angiograms obtained after this maneuver showed recanalization of the ICA and anterior cerebral artery, but occlusion of the proximal M1 segment persisted 130 minutes after onset of the symptoms (Fig 3D). The microcatheter was advanced into the right M1 segment, and an additional 60,000 U of urokinase was injected in the embolus. Heparinized sodium chloride solution was injected into the embolus three times, and several movements of the microcatheter were performed. Persistent occlusion of the proximal M1 segment was shown at local angiography after each procedure. Several movements of the J-shaped microguidewire tip in the embolus recanalized the M1 segment 150 minutes after symptom onset and removed the embolus to the proximal M2 segment (Fig 3E). Local angiograms in the lateral view demonstrated fragments of the emboli located in both the parietal and angular branches of the proximal M2 segment (Fig 3F). Injection of 60,000 U urokinase into the clot located in the parietal artery had no effect. The microcatheter was moved into the embolus over a guidewire several times; this procedure removed the embolus to the distal M2 segment. Two injections of 10 mL of heparinized sodium chloride solution in the distal M2 clot brought no improvement. Several microcatheter movements over the guidewire fragmented the clot with recanalization of the entire parietal artery (Fig 4A and B). For the embolus in the M2 segment of the angular artery, several movements of the microcatheter through the clot opened the segment, and the embolus was moved to the distal M4 segment. DSA images from the guide catheter showed complete recanalization of the ICA and most parts of the MCA; however, the distal M4 segment of the angular distribution remained occluded (Fig 2B). Intra-arterial thrombolysis was terminated 170 minutes after stroke onset. The patient could raise his left limbs and keep them raised 24 hours after the procedure. One month after stroke onset, the patient was discharged home free of any neurologic deficits, and he returned to his previous work.
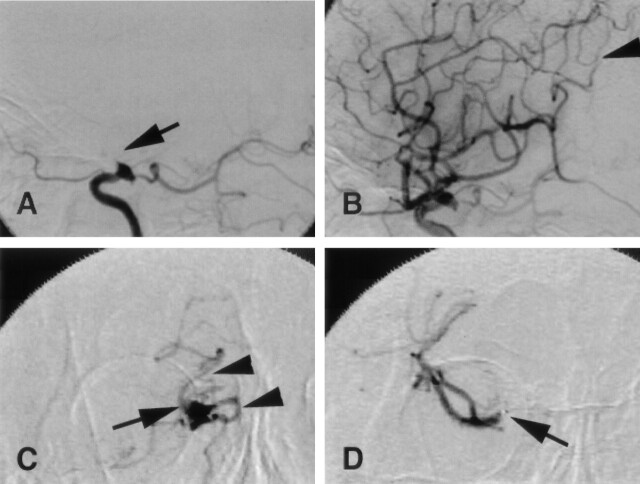
Fig 2.
Case 18. Right internal carotid angiograms, lateral view, before (A) and after (B) thrombolysis and local angiograms from a microcatheter (C and D).
A, Right ICA is occluded distal to the orifice of the posterior communicating artery (arrow).
B, ICA is recanalized. Distal M4 segment of the angular artery is persistently occluded by the fragmented embolus (arrowhead).
C, AP view from a microcatheter proximal to the embolus shows that the ICA is occluded (arrow) distal to the orifice of the posterior communicating artery (arrowheads).
D, AP view from a microcatheter in the distal end of the embolus shows no filling of contrast medium in the proximal MCA M1 segment (arrow). Findings indicate that the embolus extends from the distal ICA to the mid-M1 segment.
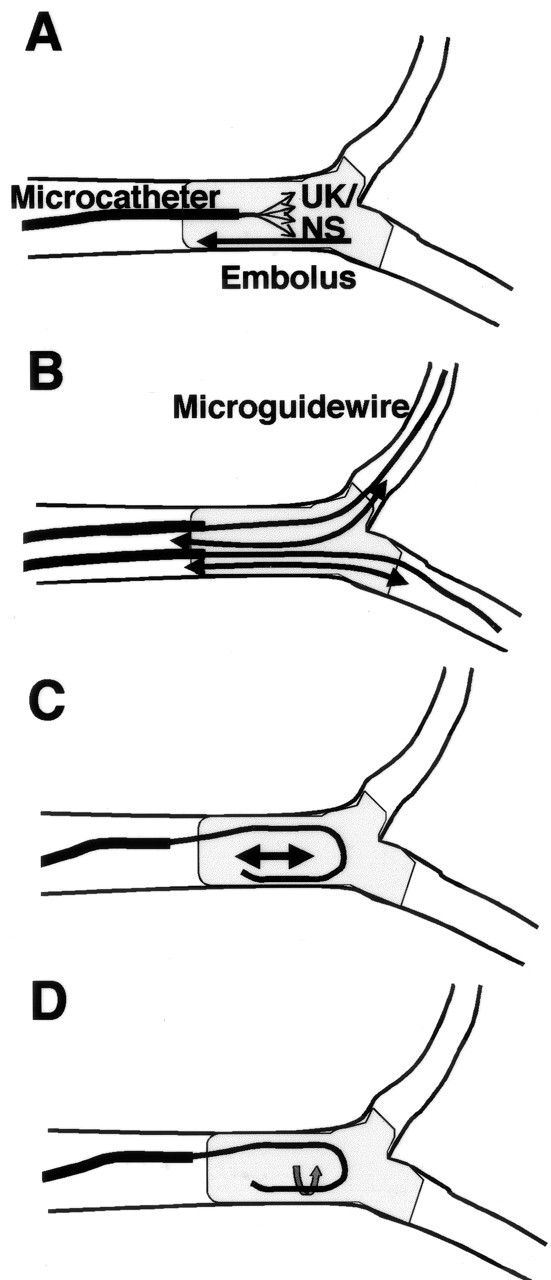
Fig 3.
Case 18. Mechanical disruption with a J-shaped microguidewire during thrombolytic therapy (A–C) and local angiograms from a microcatheter (D–F).
A and B, J-shaped tip (arrows) is moved from a position proximal to the embolus (A) to a distal position (B).
C, J-shaped tip (arrow) is rotated in the embolus.
D, AP view shows that the MCA M1 segment is occluded (arrow) just distal to the orifice of the anterior cerebral artery (arrowheads). Dislodgment of the embolus from the distal ICA to the mid-M1 segment is indicated.
E, AP view shows dislodgment of the embolus to the MCA M2 segment (arrow). The exact location of the embolus is difficult to identify on this view.
F, Lateral view shows fragmented emboli in the M2 segments of the parietal (arrow) and angular (arrowhead) arteries.
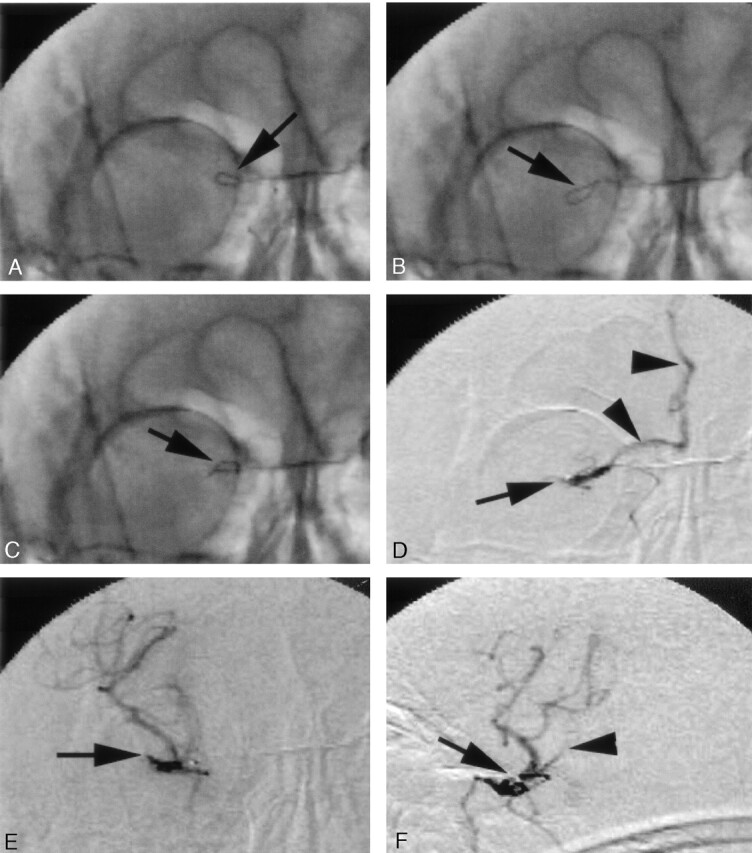
Fig 4.
Case 18. Local angiograms, lateral view, from a microcatheter.
A, Recanalization of the parietal artery.
B, Embolus in the M2 segment of the angular artery (arrow).
Discussion
Although local intra-arterial thrombolysis has been more effective than intravenous therapy in recanalizing occluded arteries responsible for acute ischemic stroke, recanalization is unsuccessful in about one-third of occluded arteries (12). With such a failure rate of pharmacologic therapy, other techniques must be considered to improve results. A high rate of recanalization was achieved in 22 (95.7%) of 23 patients in this study with thrombolysis and mechanical disruption by using a microcatheter and a microguidewire.
Techniques of Mechanical Disruption with a Microcatheter or Microguidewire
We used several techniques for mechanical clot disruption involving a microcatheter and a microguidewire during intra-arterial thrombolysis.
Forceful injection of urokinase solution.—
Forceful local infusion of fibrinolytic agent disrupts the clot mechanically, increases its surface area, and thereby hastens enzyme action compared with constant-agent infusion methods, which are time consuming (13). We tried to administer 360,000 U of urokinase at the early stage of fibrinolytic therapy to prolong the duration of the enzymatic reaction and the progress of the fibrinolysis during the procedure. Forceful injection of urokinase solution was mainly used for emboli in the ICA and the M1 segment (Table 3). This procedure removed the embolus in 17 (14.9%) of 114 applications. This procedure was safely performed without any complications.
Forceful injection of heparinized normal sodium chloride solution.—
A mechanical effect of the ejection pressure from the microcatheter on the clot was expected. This procedure was frequently used for emboli located in the M2 segment (Table 3). Emboli were moved after 11 (13.4%) of 82 applications. No vessel damage was caused by this procedure.
Mechanical disruption by movement of a microcatheter over a guidewire along the vasculature.—
The diameter of the microcatheter (0.83 mm) is more than twice of that of the microguidewire (0.41 mm). The large contact surface to embolus is advantageous to the microcatheter for destruction of the clot. We used a fiber-braided microcatheter (Renegade; Boston Scientific Corporation), because the pressure induced by an operator’s manipulation at the proximal end can be transmitted easily to the distal end that contacts the embolus. When an embolus is located at a bifurcation, it usually enters both distal branches. If a part of the embolus in one distal branch is fragmented, the anchored part of the embolus entering another branch prevents the entire embolus from movement. To achieve recanalization, it is important to fragment both parts of the embolus entering the distal branches by advancing the microcatheter into the both distal arteries. Emboli were moved in 68 (38.2%) of 178 applications. Vessel-wall perforation by a tip of a microguidewire (not by a microcatheter) occurred once (0.6%). This technique should be performed carefully to avoid vessel damage. A microguidewire should not be pushed against resistance because its tip might migrate into a small artery, and it should not be advanced into the M4 segment of the MCA because the vessel wall is usually thin.
Mechanical disruption by movement of a J-shaped microguidewire tip along the vasculature.—
To fragment an embolus, the convex border of a J-shaped guidewire tip is advantageous because of its large contact surface. Emboli were moved in 32 (52.2%) of 63 applications. Vascular damage occurred once (1.6%). Pressure might be easily transmitted to the vessel wall as well as to the embolus; therefore, the risk of vessel damage should be considered whenever this procedure is performed. We used this procedure when no recanalization was achieved by means of the three previously described techniques.
Mechanical disruption by rotation of a J-shaped microguidewire tip in the embolus.—
This method was so effective that recanalization was achieved in eight (88.9%) of nine applications. However, this technique might induce arterial-wall dissection; therefore, we did not choose this method when severe arteriosclerotic changes were found in the vessel wall or when the embolus was located in arteries distal to the M2 segment. Although no complications were observed with this procedure in this study, this approach should be selected only for patients with no response to the other mechanical disruption methods.
Comparison with Other Methods
Comparison with intra-arterial pharmacologic thrombolysis alone.—
Direct comparison of our results with those of previous studies was not possible because of crucial differences in patient selection, recanalization grades, and definitions of neurologic deterioration. An indirect comparison with results from the Prolyse in Acute Cerebral Thromboembolism (PROACT) II study suggests a higher incidence of recanalization associated with the use of intra-arterially administered urokinase with mechanical disruption of clot (95.7%) than with intra-arterial prourokinase without mechanical disruption (66%) (1). This difference was observed despite the fact that PROACT II included only patients with occlusions of the M1 or M2 division of the MCA. In our series, 11 patients had an occlusion of the ICA, which is associated with a lower incidence of recanalization than MCA occlusion. Although mechanical disruption has some technical difficulties, this procedure is apparently superior to intra-arterial infusion alone with regard to reestablishing blood flow (1, 3, 5, 12, 14, 15).
Mechanical disruption holds several theoretical advantages over chemical thrombolysis in the treatment of acute stroke. One potential advantage of mechanical thrombolysis is the rapidity with which the vessel is opened. Thrombolysis with continuous infusion may take longer than one-time injection, and it may delay reopening of the occluded artery, leading to reperfusion hemorrhage. A major shortcoming of intra-arterial thrombolysis is the time from when the decision is made to the start of thrombolysis. The techniques of mechanical thrombolysis may restore blood flow to ischemic tissue in less time. Another potential benefit of mechanical thrombolysis compared with chemical thrombolysis is a theoretically lower risk of symptomatic hemorrhage due to the ability to reduce the amount of lytic agent administered.
Comparison with angioplasty by using balloon catheters.—
Mechanical lysis of the clot by using balloon catheters has been reported to promote the frequency of recanalization. The 95.7% rate of symptomatic vessel recanalization in this study is not at all inferior to that reported with angioplasty (7, 16). This method requires only a microcatheter and a microguidewire, which are usually used in intra-arterial local fibrinolysis, and no special equipment is necessary. The disadvantage of angioplasty is its cost. For emergency angioplasty to be available to treat acute ischemic stroke, the equipment, which includes several types of balloon catheters, must be in constant readiness. This requirement reduces the number of hospitals that can offer this therapy in time and delays treatment, potentially limiting its efficacy and use in large numbers of patients. Mechanical disruption with a microcatheter and a guidewire can be applied for an extensive portion of the artery. Intracranial balloon angioplasty, particularly in bending arteries or arteries beyond the M1 segment of the MCA, is perceived to be a riskier endovascular technique (17). It is more difficult to access distal arteries with a balloon catheter than with a microcatheter. More severe vascular injury might result from balloon angioplasty, because higher pressures on the vessel wall are used to achieve mechanical thrombolysis. In this series, complications of mechanical disruption with a microcatheter and aguidewire were caused by perforation of the vessel wall. Intracranial balloon angioplasty can lead to arterial dissection or catastrophic vascular rupture. Balloon angioplasty of the distal ICA and proximal M1 segment can occlude the anterior choroidal artery origin or lenticulostriates by pressing the clot into these small arteries. Compared with a microcatheter technique, balloon angioplasty has an additional delay related to selective balloon catheterization and to changing the sheath and guide catheter for those of larger size. In addition, hemostasis can easily be achieved after a smaller sheath is removed.
Comparison with previously reported mechanical disruption by using a microcatheter and guidewire.—
Several groups have reported mechanical disruption of clots by using microcatheters or guidewires, or both, in combination with intra-arterial thrombolysis for acute ischemic stroke (4, 6, 18–21). However, to our knowledge, no previous studies detailed the mechanical disruption technique. In our experience, simple traverse movement of the microcatheter or microguidewire into the thrombus alone never disrupted the clot. Jansen et al (22) likewise reported no significant fragmentation of the thrombus or any change in the overall angiographic appearance by passing a microcatheter through the thrombus.
Intra-Arterial Thrombolysis of Distal ICA Occlusion
Mechanical disruption with a microcatheter and a guidewire with intra-arterial thrombolysis resulted in a high rate of recanalization (91%) in patients with distal ICA occlusion. This rate was higher than that of the most previous studies (19–25). In our series, four patients (36.4%) had poor outcomes: One patient died, two patients were bedridden (mRS score, 5), and one patient was not able to walk because of an embolism in the left leg (mRS score, 4). The natural history of acute ICA occlusion is poor, with estimated mortality rates of 16–55% and significant morbidity rates of 40–69% (26). This condition has been consistently associated with high rates of brain swelling, frequently followed by herniation and death (22, 27).
Most studies on thrombolytic therapy have dealt mainly with MCA occlusion. Previous studies (15, 23–25, 28, 29) have shown that an acute occlusion of the distal ICA treated with intra-arterial thrombolysis has a poor prognosis; this lesion commonly leads to death, with morbidity and mortality rates substantially higher than those for acute MCA occlusion (22). Despite the increased use of intravenous and intra-arterial thrombolysis, the incidence of recanalization in intracranial ICA occlusion remains low. In patients with embolic ICA occlusion, the embolus is often so large that it is resistant to thrombolysis, and time-consuming therapy with high doses of thrombolytic agents may be required; this may result in an unfavorable outcome with hemorrhagic complications. Some authors have concluded that patients with a distal occlusion of the ICA have little potential benefit from thrombolysis and that they should be excluded on the basis of findings at angiography, CT angiography, or MR angiography (28).
The proposed explanation for the dismal outcomes after carotid distal occlusion is partly related to the size and composition of the clot. It has been postulated that large, cohesive, and rigid emboli are more prone to occlude the distal carotid artery as the first major narrowing in the high-flow anterior circulation. Smaller, more flexible emboli are able to reach more distal branches of the arterial tree with or without previous fragmentation. The larger emboli are probably composed of aged thrombotic material that might be intrinsically less responsive to fibrinolytic agents.
In this series of distal ICA occlusion, one patient (case 23) died of transtentorial herniation 3 days after thrombolytic therapy. The M2 segment of the frontal and central distribution was persistently occluded immediately after treatment. Extensive brain edema associated with cerebral infarction developed 2 days after treatment and seemed to be caused by delayed recanalization of the occluded segment. Recanalization of at least the distal M2 segment during thrombolytic therapy was considered to be important for preventing fatal brain swelling.
Preventive Measures Against Complications
Mechanical disruption therapy poses considerable risk to the patient. Therefore, it should be performed with caution to prevent complications. Comprehension of the shape and direction of target arteries is important to prevent vascular damage. To avoid vessel perforation, repeated local angiography from a microcatheter with manual injections was performed after each maneuver to assess the state of emboli and distal vessels. Early detection of vascular damage was also achieved by means of repeated local angiography. Catheterization of thin-walled vessels might induce vascular damage. Manipulation of the microcatheter and guidewire in the M2 and more distal segments was carefully and gently performed, and advancement of the guidewire beyond the M3 segment was avoided. Because arteriosclerotic vessels seem to be vulnerable to wall damage, movement and rotation of a J-shaped guidewire tip was minimized, especially in elderly patients or patients with diabetes mellitus.
Blood pressure was controlled in the two patients with hemorrhagic complications immediately after extravasation was found at angiography, and the extravasation was confirmed on the basis of CT findings. Protamine sulfate was administered to reverse the heparinization. In both cases, the hemorrhage did not lead to a fatal outcome. In this study, extravasation originated from vessel-wall perforation not due to dissection or rupture, as might happen in balloon angioplasty. When a major artery with a thick muscular layer is perforated, rapid hemostasis might be achieved with the early management previously described.
Delayed recanalization after thrombolytic therapy can lead to poor outcomes from hemorrhagic infarct. No symptomatic deterioration due to hemorrhagic infarct was seen in our study. Hemorrhagic infarct is the result of severe ischemic injury that extends to the degradation of the basal lamina (30, 31). Hemorrhagic infarct could be prevented by performing recanalization before this ischemic damage occurs in the vessel wall. Differentiating early contrast enhancement and bleeding on CT scans obtained immediately after the procedure is important, because reversal of heparinization and strict blood pressure control should be performed in cases of hemorrhage. To reduce the incidence of staining, the contrast medium for local angiography was diluted three times.
Disconnection of a guidewire tip during manipulation has been reported in the instructions for the guidewire (Radifocus; Terumo). According to the manufacturer’s instructions, continuous rotation of a 0.018-inch guidewire with a 90° flexed tip (radius of curvature, 3.5 mm) for 50 minutes could possibly induce disconnection of the distal part of the guidewire. Mechanical disruption by using the tip of the microguidewire might be better if it is limited to emboli for which the forceful injection of urokinase solution or heparinized sodium chloride solution and the movement of a microcatheter do not work. Although a certain percentage of patients have iatrogenic hemorrhage, arterial occlusion resistant to thrombolysis has a poor prognosis, and higher-risk maneuvers may be justified in some.
Study Limitations
We used 600,000 U of urokinase as the maximum doses of a fibrinolytic agent. In Japan, urokinase up to 600,000 U is the only currently available and approved thrombolytic agent for use in stroke patients. The Japanese Ministry of Health and Welfare has not approved the use of tissue plasminogen activator (tPA) for stroke treatment, although thrombolysis with intravenously administered tPA is the standard treatment for the acute ischemic stroke within 3 hours of symptom onset in the United States (32). Therefore, in Japan, it is impossible to perform a controlled study to compare the standard therapy in the United States with our treatment.
We did not perform perfusion studies at the time of the MR imaging examinations. Our inclusion criteria, including major artery occlusion and sudden onset of severe hemiparesis, often indicate compromised blood flow in a large part of the territory of the affected vessel. It usually takes 20–30 minutes to prepare an injector connected to a patient, to perform a perfusion study, and to analyze the results. We considered an early start of thrombolytic therapy to be more important than performing the perfusion study. However, evaluating the dissociation between DW images, MR images, and perfusion images might be useful for improving outcomes.
We did not evaluate leptomeningeal collaterals with DSA because the circle of Willis had already been evaluated with MR angiography. Patients with poor proximal collateral via the circle of Willis may have a robust leptomeningeal collateral that is not detectable on MR angiograms. Because such collaterals may markedly affect the outcomes of patients with proximal occlusions, this factor might have influenced the outcome of some subjects. This is also one potential limitation of the study.
Because of the small sample size, our results are preliminary and preclude us from reaching completely generalized conclusions. We believe that future, larger studies including control groups are needed.
Conclusion
A high rate of recanalization and clinical improvement can be observed in patients with ischemic stroke after treatment with thrombolytic agents and adjunctive mechanical disruption of clots by using a microcatheter and a guidewire. We achieved recanalization in 100% of patients with proximal MCA occlusion and in 91% with distal ICA occlusion. The results of this study indicate that distal ICA and proximal MCA occlusion in patients with severe neurologic deficits may be treated with mechanical thrombolysis, with a potential for substantial neurologic improvement. However, the risk of arterial perforation must be considered, and further study is needed.
Acknowledgments
We thank Mr Kenichi Miyoshi for his excellent technical assistance.
References
- 1.Furlan A, Higashida R, Wechsler L, et al. Intra-arterial prourokinase for acute ischemic stroke, the PROACT II study: a randomized controlled trial—Prolyse in Acute Cerebral Thromboembolism. JAMA 1999;282:2003–2011 [DOI] [PubMed] [Google Scholar]
- 2.Lewandowski CA, Frankel M, Tomsick TA, et al. Combined intravenous and intra-arterial r-TPA versus intra-arterial therapy of acute ischemic stroke: emergency management of stroke (EMS) bridging trial. Stroke 1999;30:2598–2605 [DOI] [PubMed] [Google Scholar]
- 3.Del Zoppo GJ, Higashida RT, Furlan AJ, Pessin MS, Rowley HA, Gent M. PROACT: a phase II randomized trial of recombinant pro-urokinase by direct arterial delivery in acute middle cerebral artery stroke. Stroke 1998;29:4–11 [DOI] [PubMed] [Google Scholar]
- 4.Barnwell S, Clark WM, Nguyen TT, O’Neill OR, Wynn ML, Coull BM. Safety and efficacy of delayed intraarterial urokinase therapy with mechanical clot disruption for thromboembolic stroke. AJNR Am J Neuroradiol 1994;15:1817–1822 [PMC free article] [PubMed] [Google Scholar]
- 5.Edwards MT, Murphy MM, Geraghty JJ, Wulf JA, Konzen JP. Intra-arterial cerebral thrombolysis for acute ischemic stroke in a community hospital. AJNR Am J Neuroradiol 1999;20:1682–1687 [PMC free article] [PubMed] [Google Scholar]
- 6.Nesbit GM, Clark WM, O’Neill O, Barnwell SL. Intracranial intraarterial thrombolysis facilitated by microcatheter navigation through an occluded cervical internal carotid artery. J Neurosurg 1996;84:387–392 [DOI] [PubMed] [Google Scholar]
- 7.Qureshi AI, Ali Z, Siddiqui AM, et al. Aggressive mechanical clot disruption and low-dose intra-arterial third-generation thrombolytic agent for ischemic stroke: a prospective study. Neurosurgery 2002;51:1319–1329 [DOI] [PubMed] [Google Scholar]
- 8.Tsai FY, Berberian B, Matovich V, Lavin M, Alfieri K. Percutaneous transluminal angioplasty adjunct to thrombolysis for acute middle cerebral artery rethrombosis. AJNR Am J Neuroradiol 1994;15:1823–1829 [PMC free article] [PubMed] [Google Scholar]
- 9.Sasaki O, Takeuchi S, Koizumi T, Koike T, Tanaka R. Complete recanalization via fibrinolytic therapy can reduce the number of ischemic territories that progress to infarction. AJNR Am J Neuroradiol 1996;17:1661–1668 [PMC free article] [PubMed] [Google Scholar]
- 10.Brott T, Adams HP, Olinger CP, et al. Measurement of acute cerebral infarction: a clinical examination scale. Stroke 1989;20:864–870 [DOI] [PubMed] [Google Scholar]
- 11.Van Swieten JC, Koudstaal PJ, Visser MC, Schouten HJ, Van Gigin J. Interobserver agreement for the assessment of handicap in stroke patients. Stroke 1988;19:604–607 [DOI] [PubMed] [Google Scholar]
- 12.Lisboa RC, Jovanovic BD, Alberts MJ. Analysis of the safety and efficacy of intra-arterial thrombolytic therapy in ischemic stroke. Stroke 2002;33:2866–2871 [DOI] [PubMed] [Google Scholar]
- 13.Kandarpa K, Drinker PA, Singer SJ, Caramore D. Forceful pulsatile local infusion of enzyme accelerates thrombolysis: in vivo evaluation of a new delivery system. Radiology 1988;168:739–744 [DOI] [PubMed] [Google Scholar]
- 14.Qureshi AI, Ali Z, Suri FK, et al. Intra-arterial third-generation recombinant tissue plasminogen activator (Reteplase) for acute ischemic stroke. Neurosurgery 2001;49:41–50 [DOI] [PubMed] [Google Scholar]
- 15.Sasaki O, Takeuchi S, Koike T, Koizumi T, Tanaka R. Fibrinolytic therapy for acute embolic stroke: intravenous, intracarotid, and intra-arterial local approaches. Neurosurgery 1995;36:246–253 [DOI] [PubMed] [Google Scholar]
- 16.Nakano S, Iseda T, Yoneyama T, Kawano H, Wakisaka S. Direct percutaneous transluminal angioplasty for acute middle cerebral artery trunk occlusion: an alternative option to intra-arterial thrombolysis. Stroke 2002;33:2872–2876 [DOI] [PubMed] [Google Scholar]
- 17.Takis C, Kwan ES, Pessin MS, Jacobs DH, Caplan DH. Intracranial angioplasty: experience and complications AJNR Am J Neuroradiol 1997;18:1661–1668 [PMC free article] [PubMed] [Google Scholar]
- 18.Arnold M, Schroth G, Nedeltchev K, et al. Intra-arterial thrombolysis in 100 patients with acute stroke due to middle cerebral artery occlusion. Stroke 2002;33:1828–1833 [DOI] [PubMed] [Google Scholar]
- 19.Ernst R, Pancioli A, Tomsick T, et al. Combined intravenous and intra-arterial recombinant tissue plasminogen activator in acute ischemic stroke. Stroke 2000;31:2552–2557 [DOI] [PubMed] [Google Scholar]
- 20.Suarez JI, Zaidat OO, Sunshine JL, Tarr R, Selman WR, Landis D. Endovascular administration after intravenous infusion of thrombolytic agents for the treatment of patients with acute ischemic strokes. Neurosurgery 2002;50:251–260 [DOI] [PubMed] [Google Scholar]
- 21.Zaidat OO, Suarez JI, Santillan C, et al. Response to intra-arterial and combined intravenous and intra-arterial thrombolytic therapy in patients with distal internal carotid artery occlusion. Stroke 2002;33:1821–1827 [DOI] [PubMed] [Google Scholar]
- 22.Jansen O, von Kummer R, Forsting M, Hacke W, Sartor K. Thrombolytic therapy in acute occlusion of the intracranial internal carotid artery bifurcation. AJNR Am J Neuroradiol 1995;16:1977–1986 [PMC free article] [PubMed] [Google Scholar]
- 23.Gonner F, Remonda L, Mattle H, et al. Local intra-arterial thrombolysis in acute ischemic stroke. Stroke 1998;29:1894–1900 [DOI] [PubMed] [Google Scholar]
- 24.Jahan R, Duckwiller GR, Kidwell CS, et al. Intraarterial thrombolysis for treatment of acute stroke: experience in 26 patients with long-term follow-up. AJNR Am J Neuroradiol 1999;20:1291–1299 [PMC free article] [PubMed] [Google Scholar]
- 25.Von Kummer R, Holle R, Rosin L, Forsting M, Hacke W. Does arterial recanalization improve outcome in carotid territory stroke? Stroke 1995;26:581–587 [DOI] [PubMed] [Google Scholar]
- 26.Meyer FB, Piepgras DG, Sandok BA, Sundt TM Jr., Forbes G. Emergency carotid endarterectomy for patients with acute carotid occlusion and profound neurological deficits. Ann Surg 1986;203:82–89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Toni D, Fiorelli M, Gentile M, et al. Progressing neurological deficit secondary to acute ischemic stroke: a study on predictability, pathogenesis, and prognosis. Arch Neurol 1995;52:670–675 [DOI] [PubMed] [Google Scholar]
- 28.Kucinski T, Koch C, Grzyska U, Freitag HJ, Kromer H, Zeumer H. The predictive value of early CT and angiography for fatal hemispheric swelling in acute stroke. AJNR Am J Neuroradiol 1988;19:839–846 [PMC free article] [PubMed] [Google Scholar]
- 29.Suarez JI, Sunshine JL, Tarr R, et al. Predictors of clinical improvement, angiographic recanalization, and intracranial hemorrhage after intra-arterial thrombolysis for acute ischemic stroke. Stroke 1999;30:2094–2100 [DOI] [PubMed] [Google Scholar]
- 30.Cambell JK, Houser OW, Steven JC, et al. Computed tomography and radionuclide imaging in the evaluation of ischemic stroke. Radiology 1978;126:695–699 [DOI] [PubMed] [Google Scholar]
- 31.Del Zoppo GJ, von Kummer R, Hamann GF. Ischaemic damage of brain microvessels: inherent risks for thrombolytic treatment in stroke. J Neurol Neurosurg Psychiatry 1998;65:1–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. Tissue plasminogen activator for acute ischemic stroke: The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. N Engl J Med 1995;333:1581–1587 [DOI] [PubMed] [Google Scholar]