Abstract
Objectives
To measure the effect of social distancing on reducing daily deaths, infections and hospital resources needed for coronavirus disease 2019 (COVID-19) patients during the first wave of the pandemic in Nordic countries.
Methods
The observations of social distancing, daily deaths, infections along with the needed hospital resources for COVID-19 patient hospitalizations including the numbers of all hospital beds, beds needed in ICUs and infection wards, nursing staffs needed in ICUs and infection wards were collected from the Institute for Health Metrics and Evaluation (IHME) by the University of Washington. The observations of social distancing were based on the reduction in human contact relative to background levels for each location quantified by cell phone mobility data collected from IHME. The weighted data per 100,000 population gathered in a 40-day period of the first wave of the pandemic in Denmark, Finland, Iceland, Norway and Sweden. Statistical technique of panel data analysis is used to measure the associations between social distancing and COVID-19 indicators in long-run.
Results
Results of dynamic long-run models confirm that a 1% rise in social distancing by reducing human contacts may decline daily deaths, daily infections, all hospital beds needed, beds/nurses needed in ICUs and beds/nurses needed in infection wards due COVID-19 pandemic by 1.13%, 15.26%, 1.10%, 1.17% and 1.89%, respectively. Moreover, results of error correction models verify that if the equilibriums between these series are disrupted by a sudden change in social distancing, the lengths of restoring back to equilibrium are 67, 62, 40, 22 and 49 days for daily deaths, daily infections, all hospital beds needed, nurses/beds needed in ICUs and nurses/beds needed in infection wards, respectively.
Conclusion
Proper social distancing was a successful policy for tackling COVID-19 with falling mortality and infection rates as well as the needed hospital resources for patient hospitalizations in Nordic countries. The results alert governments of the need for continuously implementing social distancing policies while using vaccines to prevent national lockdowns and reduce the burden of patient hospitalizations.
Keywords: COVID-19, Intensive care units, Health resources, Hospitalization, Mortality, Nursing staff, Pandemics, Physical distancing
What is known?
-
•
Social distancing is mentioned as a success policy to prevent the spread of coronavirus disease 2019 (COVID-19) during the first wave of pandemic, although there is a lack of empirical research to measure the role of social distancing on tackling pandemic and reducing the burden of patient hospitalizations in Nordic region.
What is new?
-
•
There were meaningful associations between the level of social distancing and daily deaths, infections and the needed hospital resources during the first peak of pandemic in Nordic region.
-
•
A 1% rise in social distancing may reduce daily deaths, daily infections, all hospital beds needed, nurses/beds needed in ICUs and nurses/beds needed in infection wards due COVID-19 pandemic by 1.13%, 15.26%, 1.10%, 1.17% and 1.89%, respectively.
-
•
If the equilibriums between social distancing and COVID-19 indicators is disrupted by a sudden change in social distancing, the lengths of restoring back to the equilibrium are at least 62 days for daily deaths and infections and 40 days for the needed hospital resources.
-
•
Proper social distancing was a successful policy for prevention and management of COVID-19 pandemic and reducing the burden of patient hospitalizations on nursing and medical staffs in Nordic countries.
1. Introduction
As of December 2020, over 75 million confirmed cases of coronavirus disease 2019 (COVID-19) along with more than 1.7 million patients’ deaths have been reported worldwide, the US with about 17,515,000, India with 10,055,000, and Brazil by 7,213,000 new cases have the most dramatic situation in the tragedy of COVID-19 pandemic [1]. By the end of 2020, the severity of COVID-19 expansions based on confirmed cases among the WHO regions was at the highest level in the Americas with more than 33 million cases, Europe with more than 23 million cases, and South-East Asia with more than 11 million cases [2]. To manage these amounts of coronavirus infections, countries need to use a huge amount of hospital resources i.e. slightly more than a million hospital beds, more than 230,000 ICU beds, 161,000 nurses in ICUs, 1,770,000 nurses in infection wards, and about 160,000 invasive ventilators worldwide [3]. Due to analysis of the International Council of Nurses (ICN), about 7% of all COVID-19 infection cases worldwide has been reported among nurses and healthcare workers worldwide which certifies that nurses and other medical staffs are at a high risk of coronavirus infections i.e. more than 230,000 positive cases found among nurses and other healthcare staffs along with more than 600 nurses died by 3-June-2020 [4].
While any specific treatment has not been founded for COVID-19, social distancing has been mentioned as the efficient way to tackle the expansion of pandemic [5]. Specifically, the implementation of strict social distance policies by governments during the first wave of pandemic successfully prevented the spread of coronavirus infections and consequently saved millions of lives [6,7]. As Maloney and Taskin [8] stated, social distancing is a non-pharmaceutical intervention that is implemented by governments due to the shout-down of nonessential businesses, stay-at-home orders, school closings etc. and mainly depends on the people’s response to voluntarily avoid public places. Amongst the negative effects of social distancing i.e. side effects on mental and physical health of populations, major disruptions across multiple dimensions of life together with suppressing economic activities [[9], [10], [11]], social distancing was a beneficial policy for reducing the burden of patient hospitalizations due to COVID-19 and preventing national lockdowns.
However, the severity of social distancing varies in different countries due to different responses of governments to the pandemic [12]. In the Nordic region, all countries except Sweden were pioneering to start severe pandemic lockdown policies from the very first days of observed positive infections during the first wave of the pandemic. Nordic countries especially Finland and Iceland can now be seen as Europe’s success story in tackling COVID-19 pandemic using active restrictions along with proper social distancing policies. While millions of people worldwide faced a severe lockdown, Finland, Iceland, Denmark and Norway reduced the trend of coronavirus infection and mortality rates by implementing a track-and-trace system to keep the level of social distancing at the proper level with the aim of preventing COVID-19 patient hospitalizations and reducing its burden on healthcare systems. This clearly explains the low level of COVID-19 infections in these countries, i.e. five times below other European countries [13]. To our knowledge, it is verified that the number of infection cases rose when social distancing policies were relaxed [14] and experts alert that different types of social distancing policies may be needed to implement for up to several years while using vaccines to manage and control the expansion of pandemic [15,16].
This study aims to measure the effect of social distancing on pandemic management due to reducing daily deaths, infections and the needed hospital resources, i.e. the number of hospitals beds in ICUs and infection wards as well as nursing staffs needed to treat infected patients during a 40-day period of the first wave of the pandemic in Nordic countries.
2. Data description
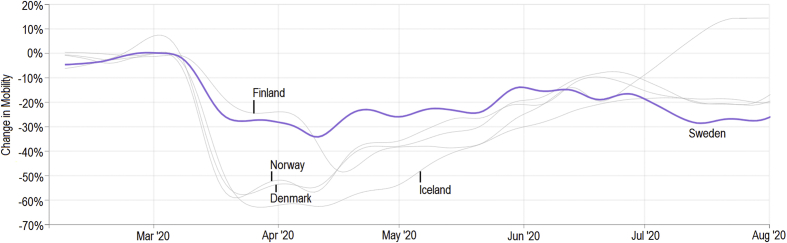
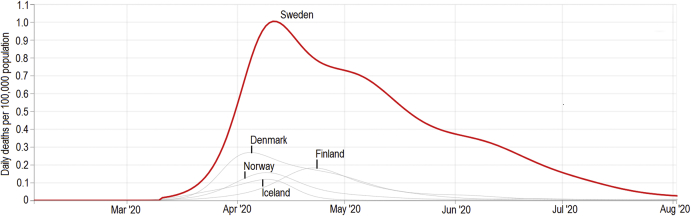
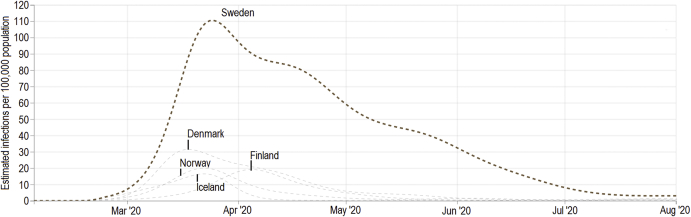
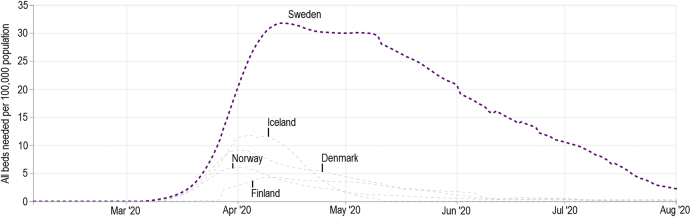
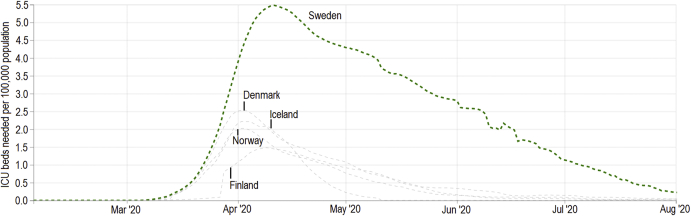
The observations of social distancing were based on the reduction in human contact relative to background levels for each location quantified by cell phone mobility data collected from the Institute for Health Metrics and Evaluation (IHME), COVID-19 Projections by the University of Washington [3]. For more explanations about measuring social distancing, see IHME [17]. The observations of daily deaths per 100,000 population due to COVID-19 infection, daily infections which is the number of people per 100,000 population estimated to be infected with COVID-19, the total number of hospital beds and ICU beds needed to treat COVID-19 patients per 100,000 population were collected from IHME [3]. The number of needed beds in infection wards per 100,000 population is calculated by the total number of hospital beds needed minus the ICU beds needed to treat COVID-19 patients. The number of nurses needed in ICUs generated based on 7.06 overall nurses per bed at capacity [18] and the nursing staffs needed in infection wards estimated based on 2.30 nurses per bed [19]. All the observations were collected in a 40-day period of the first pandemic wave in Denmark, Finland, Iceland, Norway and Sweden when the wave in each country was at its peak based on the hospital resources used per day. The durations of data collections were 2020-03-13 to 2020-04-21 in Denmark and Norway, 2020-03-22 to 2020-04-30 in Finland, 2020-03-16 to 2020-04-24 in Iceland, and 2020-03-26 to 2020-05-04 in Sweden, respectively. The days of the peak of pandemic considered to be in the middle of data periods for each country. Fig. 1, Fig. 2, Fig. 3, Fig. 4, Fig. 5 depict the trends of each series during the first wave of the pandemic in Nordic countries.
Fig. 1.
Social distancing quantified by change in mobility and reducing human contact measured by cell phone mobility data in Nordic region during the first wave of pandemic. Source: IHME [3].
Fig. 2.
Total number of daily deaths observed specific to COVID-19 patients per 100,000 population in Nordic region during the first wave of pandemic. Source: IHME [3].
Fig. 3.
Total number of estimated daily infections specific to COVID-19 per 100,000 population in Nordic region during the first wave of pandemic. Source: IHME [3].
Fig. 4.
Total number of hospital beds needed for COVID-19 patients per 100,000 population in Nordic region during the first wave of pandemic. Source: IHME [3].
Fig. 5.
Total number of ICU beds needed for COVID-19 patients per 100,000 population in Nordic region during the first wave of pandemic. Source: IHME [3].
3. Panel data analysis
The statistical technique of panel data is applied to analyze and quantify the associations social distancing and our COVID-19 indicators in long-run. Due to the nature of our data, i.e. we have the observations of 40 days period in five countries, the statistical technique of panel data analysis is the efficient method of analyzing our series. Stationarity test following by co-integration analysis, dynamic long-run models and error corrections models in the form of panel data are applied here to study the impact of social distancing in tackling pandemic due to reducing mortality and infection rates as well as the needed hospital resources during the first wave of the pandemic in Nordic countries. For more explanation and application of time series and panel data analysis in nursing and health sciences, review refs. [[20], [21], [22], [23], [24], [25], [26], [27], [28]].
3.1. Stationarity test
Unit root test is an essential examination in panel data analysis to study the possible effect of time on panel series. Based on the results of unit root test, panel series divide to two subgroups of stationary and nonstationary series and this effect on the modeling and model structure of other panel analyses like dynamic long-run and error correction models. Here, three common types of panel unit root tests including Levin, Lin & Chu t-test [29], ADF - Fisher Chi-square test [30] and PP - Fisher Chi-square test [31] applied to conclude about the stationarity of our panel series. Results of panel unit root tests are presented in Table 1 and verify that all panel series had stochastic trends, i.e. there is not any correlation between our series and time trend. Hence, time trend is not an essential factor in measuring the effectiveness of social distancing on COVID-19 indicators in long-run.
Table 1.
Panel unit-root test (Nordic region in a 40-day period of the first wave of pandemic).
| Null hypothesis: Unit root |
Level |
1st difference |
Conclusion | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Intercept |
Intercept & trend |
None |
Intercept |
||||||
| Method | Statistic | P | Statistic | P | Statistic | P | Statistic | P | |
| Social distancing | |||||||||
| Levin, Lin & Chu t | −1.97 | 0.024 | −10.09 | <0.001 | −2.52 | 0.005 | −7.49 | <0.001 | Stationary |
| ADF - Fisher Chi-square | 47.83 | <0.001 | 290.57 | <0.001 | 16.80 | 0.078 | 58.67 | <0.001 | |
| PP - Fisher Chi-square | 44.92 | <0.001 | 101.64 | <0.001 | 2.42 | 0.992 | 61.89 | <0.001 | |
| Daily deaths | |||||||||
| Levin, Lin & Chu t | −3.74 | <0.001 | −1.30 | 0.096 | 1.68 | 0.954 | −2.11 | 0.017 | Stationary |
| ADF - Fisher Chi-square | 52.67 | <0.001 | 30.85 | <0.001 | 5.53 | 0.852 | 14.00 | 0.172 | |
| PP - Fisher Chi-square | 40.02 | <0.001 | 44.23 | <0.001 | 68.17 | <0.001 | 97.89 | <0.001 | |
| Daily infections | |||||||||
| Levin, Lin & Chu t | 11.60 | 1.000 | 5.65 | 1.000 | −7.54 | <0.001 | −5.25 | <0.001 | Stationary |
| ADF - Fisher Chi-square | 9.66 | 0.470 | 46.18 | <0.001 | 60.73 | <0.001 | 96.22 | <0.001 | |
| PP - Fisher Chi-square | 10.20 | 0.422 | 36.94 | <0.001 | 40.19 | <0.001 | 30.34 | <0.001 | |
| All hospital beds needed | |||||||||
| Levin, Lin & Chu t | −2.37 | 0.008 | −4.15 | <0.001 | −2.67 | 0.003 | −6.09 | <0.001 | Stationary |
| ADF - Fisher Chi-square | 62.43 | <0.001 | 61.44 | <0.001 | 33.04 | <0.001 | 51.41 | <0.001 | |
| PP - Fisher Chi-square | 65.28 | <0.001 | 317.12 | <0.001 | 6.65 | 0.757 | 68.76 | <0.001 | |
| ICU beds needed/Nurses needed in ICUs | |||||||||
| Levin, Lin & Chu t | 3.72 | 0.999 | 0.11 | 0.547 | −2.76 | 0.002 | −2.04 | 0.020 | Stationary |
| ADF - Fisher Chi-square | 15.78 | 0.106 | 199.72 | <0.001 | 40.41 | <0.001 | 39.76 | <0.001 | |
| PP - Fisher Chi-square | 66.39 | <0.001 | 273.63 | <0.001 | 44.03 | <0.001 | 48.12 | <0.001 | |
| Beds needed in infection wards/Nurses needed in infection wards | |||||||||
| Levin, Lin & Chu t | 0.37 | 0.645 | −2.87 | 0.002 | −2.26 | 0.011 | −5.98 | <0.001 | Stationary |
| ADF - Fisher Chi-square | 45.77 | <0.001 | 52.49 | <0.001 | 43.56 | <0.001 | 48.67 | <0.001 | |
| PP - Fisher Chi-square | 65.59 | <0.001 | 324.40 | <0.001 | 11.60 | 0.312 | 71.31 | <0.001 | |
Notes: The optimum lags were automatically selected by Schwarz Info Criterion (SIC). Probabilities for Fisher tests were computed using an asymptotic Chi-square distribution, whereas other tests assumed an asymptotic normality.
3.2. Panel co-integration analysis
Here, panel co-integration analysis is used to investigate the possible associations between social distancing and other COVID-19 indicators. Results of Pedroni panel co-integration test based on Engle-Granger model proposed by Pedroni [32,33] are available in Table 2 and confirm the existence of significant associations between the level of social distancing and daily deaths, daily infections, all hospital beds, ICU beds needed, beds needed in infection wards along with nurses needed in ICUs and infection wards in Nordic region during the first wave of the pandemic.
Table 2.
Pedroni residual co-integration test (Nordic region in a 40-day period of the first wave of pandemic).
| Variables | Deterministic trend specification | Methods | No weight |
Weighted |
Conclusion | ||
|---|---|---|---|---|---|---|---|
| Statistic | P | Statistic | P | ||||
| Daily deaths & social distancing | Individual intercept & trend | Panel PP-Statistic | −3.56 | <0.001 | −2.63 | 0.004 | Co-integrated |
| Panel ADF-Statistic | −4.22 | <0.001 | −4.79 | <0.001 | |||
| Group PP-Statistic | −2.60 | 0.004 | |||||
| Group ADF-Statistic | −4.21 | <0.001 | |||||
| Daily infections & social distancing | Individual intercept | Panel PP-Statistic | −2.79 | 0.002 | −2.67 | 0.003 | Co-integrated |
| Panel ADF-Statistic | −1.40 | 0.080 | −1.66 | 0.048 | |||
| Group PP-Statistic | −3.46 | <0.001 | |||||
| Group ADF-Statistic | −1.50 | 0.065 | |||||
| All hospital beds needed & social distancing | No intercept & no trend | Panel PP-Statistic | −3.92 | <0.001 | −4.05 | <0.001 | Co-integrated |
| Panel ADF-Statistic | −2.63 | 0.004 | −1.31 | 0.094 | |||
| Group PP-Statistic | −4.74 | <0.001 | |||||
| Group ADF-Statistic | −2.91 | 0.001 | |||||
| ICU beds needed & social distancing | No intercept & no trend | Panel PP-Statistic | −4.02 | <0.001 | −4.23 | <0.001 | Co-integrated |
| Panel ADF-Statistic | −2.54 | 0.005 | −2.07 | 0.019 | |||
| Group PP-Statistic | −5.64 | <0.001 | |||||
| Group ADF-Statistic | −3.35 | <0.001 | |||||
| Beds needed in infection wards & social distancing | No intercept & no trend | Panel PP-Statistic | −4.02 | <0.001 | −4.10 | <0.001 | Co-integrated |
| Panel ADF-Statistic | −2.92 | 0.001 | −1.48 | 0.068 | |||
| Group PP-Statistic | −4.79 | <0.001 | |||||
| Group ADF-Statistic | −2.59 | 0.004 | |||||
| Nurses needed in ICUs & social distancing | No intercept & no trend | Panel PP-Statistic | −3.48 | <0.001 | −3.61 | <0.001 | Co-integrated |
| Panel ADF-Statistic | −2.92 | 0.001 | −1.97 | 0.024 | |||
| Group PP-Statistic | −4.52 | <0.001 | |||||
| Group ADF-Statistic | −4.18 | <0.001 | |||||
| Nurses needed in infection wards & social distancing | No intercept & no trend | Panel PP-Statistic | −4.75 | <0.001 | −4.58 | <0.001 | Co-integrated |
| Panel ADF-Statistic | −3.74 | <0.001 | −3.00 | 0.001 | |||
| Group PP-Statistic | −5.86 | <0.001 | |||||
| Group ADF-Statistic | −3.61 | <0.001 | |||||
Notes: Null Hypothesis of Pedroni test: No cointegration. Trend assumption was the existence of no deterministic trend. Automatic lag length selection used based on SIC with a max lag of 9. Newey-West automatic used to estimate bandwidth and Bartlett was calculated by kernel.
3.3. Dynamic long-run models
According to the results of panel co-integration analysis, there were meaningful associations and/or relationships between social distancing and other COVID-19 indicators in long-run. Hence, the magnitudes of these relationships may be quantified by dynamic long-run models in the form of panel data analysis. The results of different types of dynamic long-run models based on the meaningfulness of each equation and coefficients of exogenous variables are presented in Table 3. As can be seen, the magnitude of impact social distancing had on daily deaths, daily infections, all hospital beds, beds/nurses needed in ICUs and beds/nurses needed in infection wards were −1.126761, −15.262468, −1.100327, −1.174918 and −1.886183, respectively. In other words, the results of dynamic long-run models confirm that a 1% rise in social distancing by reducing human contacts may decline daily deaths, daily infections, all hospital beds needed, beds/nurses needed in ICUs and beds/nurses needed in infection wards due COVID-19 pandemic by 1.13%, 15.26%, 1.10%, 1.17% and 1.89%, respectively. These findings certify that the proportion of daily infections was 13 times more sensitive to the level of social distancing than daily deaths and this is the logical result based on the epidemiological characteristics of coronavirus. Moreover, the magnitudes of social distancing on the number of needed nurses and hospital beds for ICUs and infection wards, which are typically dependent on each other and had a same trend during the time, were similar during the first wave of the pandemic.
Table 3.
Panel dynamic long-run models (Nordic region in a 40-day period of the first wave of pandemic).
| Dependent variable | Independent variable | Coefficient | Std. Error | t | P | r2 | Durbin-Watson stat |
|---|---|---|---|---|---|---|---|
| Daily deaths | Constant | 0.100221 | 0.06 | 1.65 | 0.098 | 0.99 | 1.24 |
| Social distancing | −0.03247 | 0.01 | −1.89 | 0.059 | |||
| Daily deaths (−1) | 0.971182 | 0.00 | 163.72 | <0.001 | |||
| Elasticity: −0.03247/(1–0.971182) = −1.126761 | |||||||
| Method: Panel EGLS (Period weights) with linear estimation after one-step weighting matrix | |||||||
| Daily infections | Constant | 0.38403 | 0.05 | 6.90 | <0.001 | 0.99 | 1.27 |
| Social distancing | −0.10833 | 0.01 | −7.82 | <0.001 | |||
| Daily infections (−1) | 0.992902 | 0.00 | 265.64 | <0.001 | |||
| Elasticity: −0.10833/(1–0.992902) = −15.262468 | |||||||
| Method: Panel EGLS (Cross-section weights) with linear estimation after one-step weighting matrix | |||||||
| All hospital beds needed | Constant | 0.39294 | 0.05 | 6.85 | <0.001 | 0.99 | 0.70 |
| Social distancing | −0.06199 | 0.01 | −4.55 | <0.001 | |||
| All hospital beds needed (−1) | 0.943664 | 0.00 | 171.28 | <0.001 | |||
| Elasticity: −0.06199/(1–0.943664) = −1.100327 | |||||||
| Method: Panel EGLS (Cross-section SUR) with linear estimation after one-step weighting matrix | |||||||
| ICU beds needed | Constant | 0.434276 | 0.05 | 7.28 | <0.001 | 0.99 | 0.81 |
| Social distancing | −0.09481 | 0.01 | −5.95 | <0.001 | |||
| ICU beds needed (−1) | 0.919305 | 0.00 | 161.89 | <0.001 | |||
| Elasticity: −0.09481/(1–0.919305) = −1.174918 | |||||||
| Method: Panel EGLS (Cross-section SUR) with linear estimation after one-step weighting matrix | |||||||
| Beds needed in infection wards | Constant | 0.398096 | 0.08 | 4.84 | <0.001 | 0.99 | 0.61 |
| Social distancing | 0.940888 | 0.15 | 6.14 | <0.001 | |||
| Social distancing (−1) | −1.01671 | 0.14 | −6.99 | <0.001 | |||
| Beds needed in infection wards (−1) | 0.959804 | 0.00 | 138.68 | <0.001 | |||
| Elasticity: (0.940888–1.01671)/(1–0.959804) = −1.886183 | |||||||
| Method: Panel EGLS (Cross-section weights) with linear estimation after one-step weighting matrix | |||||||
| Nurses needed in ICUs | Constant | 0.59199 | 0.06 | 8.63 | <0.001 | 0.99 | 0.50 |
| Social distancing | −0.09481 | 0.01 | −5.95 | <0.001 | |||
| Nurses needed in ICU (−1) | 0.919305 | 0.00 | 161.89 | <0.001 | |||
| Elasticity: –0.09481/(1–0.919305) = −1.174918 | |||||||
| Method: Panel EGLS (Cross-section weights) with linear estimation after one-step weighting matrix | |||||||
| Nurses needed in infection wards | Constant | 0.431575 | 0.08 | 4.96 | <0.001 | 0.99 | 0.49 |
| Social distancing | 0.940888 | 0.15 | 6.14 | <0.001 | |||
| Social distancing (−1) | −1.01671 | 0.14 | −6.99 | <0.001 | |||
| Nurses needed in infection wards (−1) | 0.959804 | 0.00 | 138.68 | <0.001 | |||
| Elasticity: (0.940888–1.01671)/(1–0.959804) = −1.886183 | |||||||
| Method: Panel EGLS (Cross-section weights) with linear estimation after one-step weighting matrix | |||||||
Notes: The optimum lag lengths were selected using Schwarz Info Criterion (SIC) from 0 to 2. “(−1)” in each variable means a lagged series.
3.4. Panel error correction models
In the last analysis, we analyze the effect of a shock in social distancing on its lung-run equilibrium with COVID-19 deaths, infections and hospital resources needed using error correction models in the form of panel data analysis. Results of error correction models for the first wave of pandemic are available in Table 4 and show that if the long-run equilibriums between social distancing and COVID-19 indicators were disrupted by a shock in social distancing, then the time spams of restoring back to previous equilibriums are about 67, 62, 40, 23 and 49 days for daily deaths, daily infections, all hospital beds needed, beds/nurses needed in ICUs and beds/nurses needed in infection wards, respectively.
Table 4.
Panel error correction models (Nordic region in a 40-day period of the first wave of pandemic).
| Dependent variable | Independent variable | Coefficient | Std. Error | t | P | r2 | Durbin-Watson stat |
|---|---|---|---|---|---|---|---|
| Δ Daily deaths | Constant | 0.055817 | 0.01 | 5.15 | <0.001 | 0.06 | 1.67 |
| Δ Social distancing | 0.492877 | 0.21 | 2.26 | 0.024 | |||
| Error correction (−1) | −0.014955 | 0.00 | −2.11 | 0.035 | |||
| The length of restoring back to equilibrium (days): 1/0.014955 = 66.867268 | |||||||
| Method: Panel EGLS (Cross-section SUR) with linear estimation after one-step weighting matrix | |||||||
| Δ Daily infections | Constant | −0.033482 | 0.00 | −7.24 | <0.001 | 0.09 | 1.67 |
| Δ Social distancing | 0.267803 | 0.10 | 2.65 | 0.008 | |||
| Error correction (−1) | 0.016096 | 0.00 | 3.51 | <0.001 | |||
| The length of restoring back to equilibrium (days): 1/0.016096 = 62.127237 | |||||||
| Method: Panel EGLS (Cross-section weights) with linear estimation after one-step weighting matrix | |||||||
| Δ All hospital beds needed | Constant | 0.052983 | 0.00 | 6.29 | <0.001 | 0.22 | 0.75 |
| Δ Social distancing | 0.628493 | 0.13 | 4.60 | <0.001 | |||
| Error correction (−1) | −0.024803 | 0.00 | −4.06 | <0.001 | |||
| The length of restoring back to equilibrium (days): 1/0.024803 = 40.317704 | |||||||
| Method: Panel EGLS (Cross-section weights) with linear estimation after one-step weighting matrix | |||||||
| Δ Beds/Nurses needed ICUs | Constant | 0.053300 | 0.00 | 8.93 | <0.001 | 0.45 | 0.56 |
| Δ Social distancing | 0.935694 | 0.14 | 6.27 | <0.001 | |||
| Error correction (−1) | −0.043789 | 0.00 | −5.95 | <0.001 | |||
| The length of restoring back to equilibrium (days): 1/0.043789 = 22.836785 | |||||||
| Method: Panel EGLS (Cross-section weights) with linear estimation after one-step weighting matrix | |||||||
| Δ Beds/Nurses needed in infection wards | Constant | 0.053543 | 0.00 | 6.29 | <0.001 | 0.24 | 0.81 |
| Δ Social distancing | 0.772321 | 0.14 | 5.50 | <0.001 | |||
| Error correction (−1) | −0.020388 | 0.00 | −3.41 | <0.001 | |||
| The length of restoring back to equilibrium (days): 1/0.020388 = 49.048460 | |||||||
| Method: Panel EGLS (Cross-section SUR) with linear estimation after one-step weighting matrix | |||||||
Notes: The optimum lag lengths were selected using Schwarz Info Criterion (SIC) from 0 to 2. “(−1)” in each variable means a lagged series. Error corrections calculated by the residual series gained from ordinary regressing each variable on social distancing.
4. Discussion
Social distancing and reducing human contact mentioned as a successful policy to prevent the spread of COVID-19 and reduce the burden of patient hospitalizations in the first wave of the pandemic in the absence of any special treatment or vaccine for tackling the expansion of pandemic [[5], [6], [7]]. However, the level of social distancing based on governments’ respond to pandemic varies from country to country [12]. Across the negative effects of national lockdown, social distancing was a beneficial policy for reducing the burden of patient hospitalizations on healthcare systems and healthcare workers who have been placed in the frontline of fight against COVID-19. Although the COVID-19 vaccination has been started in a few countries like UK, US and Nordic countries and it will begin in many countries soon, experts believe that different types of social distancing policies may be needed to implement for up to several years with the aim of managing pandemic in a proper way and preventing national lockdowns [15,16].
This study started a new attempt to quantify the role of social distancing in reducing daily deaths and infections as well as the needed hospital resources due to hospital beds and nurses needed in ICUs and infection wards using the observations of COVID-19 Projections provided by IHME in the University of Washington. The statistical technique of panel data analysis was used to study the observations of the Nordic region during the first wave of the pandemic. Results of co-integration analysis verified that there were meaningful associations between social distancing and COVID-19 mortality and infection rates as well as the needed hospital resources. In addition, results of dynamic long-run models showed that a 1% rise in social distancing by reducing human contacts in the Nordic region might decline daily deaths, daily infections, all hospital beds needed, beds/nurses needed in ICUs and beds/nurses needed in infection wards due COVID-19 pandemic by 1.13%, 15.26%, 1.10%, 1.17% and 1.89%, respectively. This finding clarifies that the proportion of daily infections was 13 times more sensitive to the level of social distancing than daily deaths in the first wave of the pandemic in Nordic countries. Furthermore, results of error correction models proved that if the equilibriums between these series disrupt by a sudden reduction in social distancing, the lengths of restoring back to the previous equilibriums are at least 62 days for daily deaths and infections and 40 days for the needed hospital resources that are quite long for staying in national lockdown and may have huge economic consequences in the Nordic region.
In all, the findings of this study highlight the role of proper social distancing as a successful policy for pandemic management and prevention in Nordic countries which leads to reducing patient hospitalizations, the needed hospital resources as well as the needed healthcare workers, specially nurses who are at the high risk of infecting with coronavirus. The recommendation for future research would be adding other key factors that affect the level of social distancing, e.g., the level of mask using and different lockdown policies during the second and third waves of the pandemic. More related indicators may be added to this kind of big data analysis like the levels of COVID-19 testing and vaccination by countries while these data are available.
5. Conclusion
Proper social distancing was a successful policy for tackling COVID-19 resulting from falling mortality and infection rates together with fewer hospital resources needed – i.e. nurses and hospital beds in infection wards and ICUs – for patient hospitalizations in Nordic countries. Moreover, our results alert governments the necessity of continuously implementing social distancing policies while using vaccines to prevent national lockdowns and reduce the burden of patient hospitalization on healthcare systems and healthcare staffs.
Funding
No fund received for this article.
Permissions
No permission was required for this research article because all of the instruments and measures are available in public domain and their references mentioned in the article.
Declaration of competing interest
The author has declared that no conflicts of interest exist.
Footnotes
Peer review under responsibility of Chinese Nursing Association.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijnss.2021.03.010.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.World Health Organization. WHO coronavirus disease (COVID-19) dashboard. https://covid19.who.int/. [Accessed 2020-12-22].
- 2.World Health Organization. Coronavirus disease (COVID-19) pandemic. https://www.who.int/emergencies/diseases/novel-coronavirus-2019. [Accessed 2020-12-22].
- 3.Institute for Health Metrics and Evaluation (IHME). COVID-19 Projections. University of Washington. https://covid19.healthdata.org/global?view=total-deaths&tab=trend. [Accessed 2020-12-22].
- 4.International Council Nurses. More than 600 nurses die from COVID-19 worldwide. ICN News. https://www.icn.ch/news/more-600-nurses-die-covid-19-worldwide. [Accessed 2020-12-22].
- 5.Ferguson N., Laydon D., Nedjati Gilani G., Imai N., Ainslie K., Baguelin M. vol. 10. Imperial College London; 2020. Report 9: impact of non-pharmaceutical interventions (NPIs) to reduce COVID19 mortality and healthcare demand; pp. 1–20. [DOI] [Google Scholar]
- 6.Lyu W., Wehby G.L. Shelter-in-place orders reduced COVID-19 mortality and reduced the rate of growth in hospitalizations. Heal Aff Proj Hope. 2020;39(9):1615–1623. doi: 10.1377/hlthaff.2020.00719. [DOI] [PubMed] [Google Scholar]
- 7.Siedner M.J., Harling G., Reynolds Z., Gilbert R.F., Haneuse S., Venkataramani A.S. Social distancing to slow the US COVID-19 epidemic: longitudinal pretest–posttest comparison group study. PLoS Med. 2020;17(8) doi: 10.1371/journal.pmed.1003244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Maloney W, Taskin T. Determinants of social distancing and economic activity during COVID-19: a global view. World Bank. https://openknowledge.worldbank.org/handle/10986/33754. [Accessed 2020-12-22].
- 9.Peçanha T., Goessler K.F., Roschel H., Gualano B. Social isolation during the COVID-19 pandemic can increase physical inactivity and the global burden of cardiovascular disease. Am J Physiol Heart Circ Physiol. 2020;318(6):H1441–H1446. doi: 10.1152/ajpheart.00268.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Loades E.M., Chatburn E., Higson-Sweeney N., McManus M.N., Borwick C., Crawley E. Rapid systematic review: the impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID-19. J Am Acad Child Adolesc Psychiatry. 2020;59(11):1218–1239. doi: 10.1016/j.jaac.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nicola M., Alsafi Z., Sohrabi C., Kerwan A., Al-Jabir A., Iosifidis C. The socio-economic implications of the coronavirus pandemic (COVID-19): a review. Int J Surg. 2020;78:185–193. doi: 10.1016/j.ijsu.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang Y. Government Policies, National culture and social distancing during the first wave of the COVID-19 pandemic: International Evidence. Saf Sci. 2021;135:105138. doi: 10.1016/j.ssci.2020.105138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Finnish Institute for Health and Welfare Infectious diseases and vaccinations. https://thl.fi/en/web/infectious-diseases-and-vaccinations/what-s-new/coronavirus-covid-19-latest-updates/situation-update-on-coronavirus [Accessed 2020-12-22]
- 14.Zhang W.Q., Oltean A., Nichols S., Odeh F., Zhong F. Epidemiology of reopening in the COVID-19 pandemic in the United States, Europe and Asia. medRxiv. 2020 doi: 10.1101/2020.08.05.20168757. [DOI] [Google Scholar]
- 15.Kissler S.M., Tedijanto C., Lipsitch M., Grad Y.H. Social distancing strategies for curbing the COVID-19 epidemic. medRxiv. 2020 doi: 10.1101/2020.03.22.20041079. [DOI] [Google Scholar]
- 16.Lonergan M., Chalmers J.D. Estimates of the ongoing need for social distancing and control measures post-“lockdown” from trajectories of COVID19 cases and mortality. Eur Respir J. 2020;56(1):2001483. doi: 10.1183/13993003.01483-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Institute for Health Metrics and Evaluation (IHME). COVID-19 model FAQs. University of Washington. http://www.healthdata.org/covid/faqs. [Accessed 2020-12-22].
- 18.Pediatric Intensive Care Society Nurse workforce planning for level 3 pediatric critical care units (PICU) https://pccsociety.uk/wp-content/uploads/2017/01/PICS-Nurse-Workforce-Planning-approved-October-2016-final-V1.2.pdf [Accessed 2020-12-22]
- 19.Nursing Times Higher ratio of nurses per hospital bed linked to fewer patient deaths. https://www.nursingtimes.net/news/hospital/higher-ratio-of-nurses-per-hospital-bed-linked-to-fewer-patient-deaths-18-12-2015/ [Accessed 2020-12-22]
- 20.Amiri A., Ventelou B. Granger causality between total expenditure on health and GDP in OECD: evidence from the Toda–Yamamoto approach. Econ Lett. 2012;116(3):541–544. doi: 10.1016/j.econlet.2012.04.040. [DOI] [Google Scholar]
- 21.Amiri A., Gerdtham U., Ventelou B. HIV/AIDS-GDP nexus? Evidence from panel data for African countries. Econ Bull. 2012;32(1):1060e7. [Google Scholar]
- 22.Amiri A., Linden M. Impact of child health on economic growth: new evidence based on Granger non-causality tests. Econ Bull. 2016;36(2):1127e37. [Google Scholar]
- 23.Amiri A., Solankallio-Vahteri T. Nurse-staffing level and quality of acute care services: evidence from cross-national panel data analysis in OECD countries. Int J Nurs Sci. 2019;6(1):6–16. doi: 10.1016/j.ijnss.2018.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Amiri A., Solankallio-Vahteri T. Nurse staffing and life expectancy at birth and at 65 years old: evidence from 35 OECD countries. Int J Nurs Sci. 2019;6(4):362–370. doi: 10.1016/j.ijnss.2019.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Amiri A., Solankallio-Vahteri T. Analyzing economic feasibility for investing in nursing care: evidence from panel data analysis in 35 OECD countries. Int J Nurs Sci. 2020;7(1):13–20. doi: 10.1016/j.ijnss.2019.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Amiri A., Solankallio-Vahteri T., Tuomi S. Role of nurses in improving patient safety: evidence from surgical complications in 21 countries. Int J Nurs Sci. 2019;6(3):239–246. doi: 10.1016/j.ijnss.2019.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Amiri A., Vehviläinen-Julkunen K., Solankallio-Vahteri T., Tuomi S. Impact of nurse staffing on reducing infant, neonatal and perinatal mortality rates: evidence from panel data analysis in 35 OECD countries. Int J Nurs Sci. 2020;7(2):161–169. doi: 10.1016/j.ijnss.2020.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Amiri A. Role of nurses and midwives in improving patient safety during childbirth: evidence from obstetric trauma in OECD countries. Appl Nurs Res. 2020;56:151343. doi: 10.1016/j.apnr.2020.151343. [DOI] [PubMed] [Google Scholar]
- 29.Levin A., Lin C.F., Chu C. Unit root tests in panel data: asymptotic and finite sample properties. J Econom. 2002;108(1):1–24. doi: 10.1016/S0304-4076(01)00098-7. [DOI] [Google Scholar]
- 30.Dickey D.A., Fuller W.A. Distribution of the estimators for autoregressive time series with a unit root. J Am Stat Assoc. 1979;74(366):427–431. doi: 10.1080/01621459.1979.10482531. [DOI] [Google Scholar]
- 31.Phillips P.C.B., Perron P. Testing for a unit root in time series regression. Biometrika. 1988;75(2):335–346. doi: 10.1093/biomet/75.2.335. [DOI] [Google Scholar]
- 32.Pedroni P. Critical values for co-integration tests in heterogeneous panels with multiple regressors. Oxf Bull Econ Stat. 1999;61(S1):653–670. doi: 10.1111/1468-0084.0610s1653. [DOI] [Google Scholar]
- 33.Pedroni P. Panel co-integration; Asymptotic and finite sample properties of pooled time series tests with an application to the PPP hypothesis. Econ Theory. 2004;20(3):597–625. doi: 10.1017/S0266466604203073. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.