Abstract
Background:
Clinical outcomes of surgical repairs for tears of the lateral meniscus posterior root (LMPR) in patients undergoing anterior cruciate ligament (ACL) reconstruction (ACLR) have not been comprehensively investigated.
Purpose:
To systematically review the clinical, radiographic, and arthroscopic results of surgical repairs for tears of the LMPR in patients undergoing ACLR.
Study Design:
Systematic review; Level of evidence, 4.
Methods:
A systematic electronic search of the PubMed and Embase databases was performed to identify studies reporting clinical, radiographic, or arthroscopic results of surgical repairs for tears of the LMPR in patients undergoing ACLR. Each included study was abstracted regarding study characteristics, patient characteristics, surgical technique, and outcome measures. The methodological quality of the included studies was analyzed according to the Methodological Index for Non-Randomized Studies (MINORS) criteria.
Results:
Nine studies were included in this systematic review, representing a total of 215 knees in 215 patients. Overall, 123 side-to-side repairs and 89 pullout repairs were performed for tears of the LMPR during ACLR. After a mean follow-up of 33.9 months, significant improvements (P < .05) were found in the mean Lysholm score (from 58.3 to 91.4) as well as the mean International Knee Documentation Committee subjective score (from 61.1 to 87.2). Weightbearing anteroposterior radiographs of 41 patients showed no significant narrowing of lateral joint space width. On magnetic resonance imaging scans, 31 patients demonstrated no significant progression of chondral lesions, and no significant decreases in meniscal extrusion on coronal planes were reported in another 76 patients. The complete/partial healing was 93.6% on second-look arthroscopy after side-to-side repairs for radial tears of the LMPR. The MINORS value showed a high risk of bias for all 9 studies.
Conclusion:
Patients with tears of the LMPR associated with ACL injuries achieved favorable functional scores after ACLR and LMPR repairs, and the side-to-side repair for radial tears of the LMPR succeeded in a high meniscal healing rate of >90%. However, the authors of this review were unable to definitively conclude whether LMPR repairs fully restore the hoop stress of the lateral meniscus.
Keywords: anterior cruciate ligament reconstruction, lateral meniscus, meniscal root, meniscal repair, outcomes
Meniscal lesions are commonly associated with anterior cruciate ligament (ACL) injuries and frequently involve the posterior horn of the lateral meniscus. 5,19,26 During ACL reconstruction (ACLR), tears of the lateral meniscus posterior root (LMPR) are found in up to 14% of the patients. 7 As the integrity of the LMPR is critical for the meniscal function to convert the axial load to a radially directed hoop stress and control the rotational stability of ACL-deficient knees, 4,9,23,28,31 such particular meniscal lesions should be carefully treated during ACLR.
Some previous studies have recommended leaving tears of the LMPR in situ with a view to their spontaneous healing, 14,22 but corresponding results were unsatisfactory in preventing the progression of lateral joint space narrowing. 22 Current biomechanical studies showed that the surgical repair of tears of the LMPR would better restore the normal tibiofemoral contact mechanics and knee kinematics. 6,8,9,12,21,28 Therefore, in recent years, interest in the surgical treatment of tears of the LMPR during ACLR has increased.
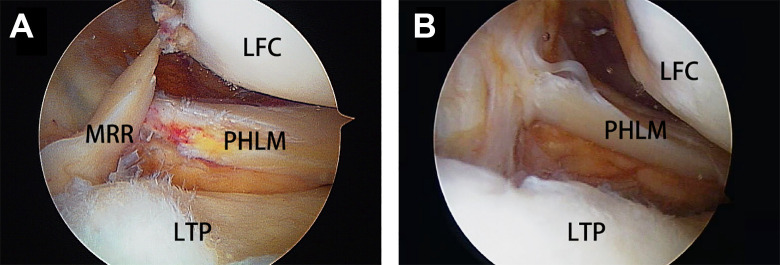
Clinically, tears of the LMPR occur with variable patterns from radial tears near the root to root avulsions (Figure 1). 7,11 Different surgical techniques, including the pullout repair for LMPR avulsions and the side-to-side repair for radial tears of the LMPR, have been applied in previous studies. 5 However, a comprehensive assessment of the available evidence on the surgical outcomes of LMPR repairs in patients undergoing ACLR is lacking.
Figure 1.
Arthroscopic views of tears of the lateral meniscus posterior root (LMPR) in 2 separate left knees. (A) A tear of the LMPR of the radial tear pattern. (B) A tear of the LMPR of the root avulsion pattern, with a meniscal root remnant completely lost. LFC, lateral femoral condyle; LTP, lateral tibial plateau; MRR, meniscal root remnant; PHLM, posterior horn of lateral meniscus.
Given this lack of data, the purpose of this study was to systematically summarize the clinical, radiographic, and arthroscopic results of surgical repairs for tears of the LMPR in patients undergoing ACLR. We hypothesized that surgically repairing tears of the LMPR during ACLR would result in good functional scores, no progression of lateral compartment degenerations, and high meniscal healing rates.
Methods
Search Strategy
This systematic review was performed following the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. 17 An electronic search of the PubMed and Embase databases was performed on July 6, 2020, to identify studies that reported the clinical, radiographic, or arthroscopic outcomes after surgical treatments for tears of the LMPR in patients undergoing ACLR. The following terms were used for the electronic search: (lateral meniscus posterior OR posterolateral meniscus) AND (root OR insertion OR attachment OR detachment). Inclusion and exclusion criteria are detailed in Table 1.
Table 1.
Study Inclusion and Exclusion Criteria a
| Inclusion Criteria | Exclusion Criteria |
|---|---|
|
|
| |
|
|
|
|
|
|
|
|
a ACL, anterior cruciate ligament; LMPR, lateral meniscus posterior root.
Two authors (G.S. and Y.L.) independently screened all articles for relevance, and all articles identified by the search terms were generally reviewed and then discussed according to the inclusion or exclusion criteria. Full-text articles were then critically reviewed, and reference lists of all included studies were reviewed for potential studies not identified by the electronic search. If there was any disagreement among the authors about a study’s inclusion, a final decision was made by the senior author (H.Z.).
Data Extraction
Each full-text article ultimately included was abstracted regarding study characteristics, patient data, surgical techniques, and outcome measures. Original data were extracted by 1 author and verified by another (Z.Z. and Q.N., respectively). Any disagreement on the data extraction was resolved by consensus between the 2 authors.
Study characteristics included author name, publication date, study design, level of evidence, number of patients/knees, and length of follow-up. Patient data consisted of sex, age, time from injury to surgery, and tear pattern of the LMPR. Surgical techniques for LMPR repairs and ACLRs were summarized according to the specific descriptions in the included studies.
Outcome measures consisted of pre- and postoperative clinical, radiographic, and arthroscopic evaluations. Clinical assessments included all subjective function scores (eg, Lysholm score, International Knee Documentation Committee [IKDC] subjective score, and Tegner score) as well as objective knee stability (eg, Lachman test, KT-1000/2000 arthrometer test, and pivot-shift test). Radiographic measurements included joint space narrowing based on weightbearing anteroposterior (AP) radiographs and cartilaginous degeneration based on magnetic resonance imaging (MRI). The lateral meniscal extrusion was also evaluated on MRI and could be measured on the coronal or sagittal plane. ACL graft and meniscal signals on follow-up MRI were extracted if recorded in original articles. The arthroscopic results were the meniscal healing status, ACL graft status, and chondral status on second-look arthroscopy.
Given the heterogeneity in patient selection, clinical interventions, and outcome measures, a quantitative comparison across studies (meta-analysis) was inappropriate. Descriptive statistics were used to report the aforementioned data.
Quality Assessment
The methodological quality of all included studies was analyzed according to the Methodological Index for Non-Randomized Studies (MINORS). 24 The items in the MINORS criteria for nonrandomized studies were scored as 2 when reported and adequate, 1 when reported but inadequate, and 0 if not reported. For noncomparative studies, the ideal MINORS score was 16, and a study was considered to have a low risk of bias when it scored 13 to 15 and a high risk of bias when it scored ≤12. In comparative studies, the corresponding thresholds were 24, 21 to 23, and ≤20, respectively. 24 Two authors (Y.C. and Z.F.) independently calculated the MINORS score of each study and discussed articles in which differences existed until consensus was reached.
Results
Literature Search and Quality Assessment
Of the 469 articles initially identified by electronic searches, 9 studies were ultimately included (Figure 2). Of the 9 studies included, 5 were retrospective cohort studies (level 3), 10,13,18,20,30 and the remaining 4 were case series (level 4). 2,3,27,32 The general features of each included study are summarized in Table 2.
Figure 2.

Flowchart of search strategy following the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. ACL, anterior cruciate ligament; LMPR, lateral meniscus posterior root.
Table 2.
Study Features a
| Lead Author | Year | Study Design | LOE | MINORS | Functional Score | Radiographic Evaluation | Second-Look Arthroscopy |
|---|---|---|---|---|---|---|---|
| Ahn 2 | 2010 | Case series | 4 | 8/16 | Lysholm, IKDC | Yes | Yes |
| Anderson 3 | 2010 | Case series | 4 | 10/16 | Lysholm, IKDC, Tegner | Yes | Yes |
| Song 27 | 2014 | Case series | 4 | 11/16 | Lysholm, Tegner | No | Yes |
| Zhuo 32 | 2020 | Case series | 4 | 10/16 | Lysholm, IKDC, Tegner | Yes | Yes |
| Tsujii 30 | 2019 | Cohort study b | 3 | 19/24 | None | Yes | Yes |
| LaPrade 13 | 2017 | Cohort study c | 3 | 16/24 | Lysholm, Tegner, WOMAC, SF-12 | No | No |
| Krych 10 | 2020 | Cohort study c | 3 | 18/24 | Lysholm, IKDC, Tegner | No | No |
| Okazaki 18 | 2020 | Cohort study d | 3 | 17/24 | IKDC | Yes | No |
| Pan 20 | 2015 | Cohort study e | 3 | 18/24 | Lysholm, IKDC | Yes | No |
a IKDC, International Knee Documentation Committee; LOE, level of evidence; MINORS, Methodological Index for Non-Randomized Studies; SF-12, 12-Item Short Form Health Survey; WOMAC, Western Ontario and McMaster Universities Osteoarthritis Index.
b This study compared the results of patients undergoing surgical repairs for lateral meniscus posterior root tears and patients without meniscal tears.
c This study compared the results of surgical repairs treating posterior root tears of the lateral and medial meniscus.
d This study compared the results of tears of the lateral meniscus posterior root treated by different repair techniques.
e This study compared the results of tears of the lateral meniscus posterior root treated by surgical repairs and left in situ.
The mean MINORS value was 17.6 ± 1.0 (range, 16-19) for comparative studies and 9.8 ± 1.1 (range, 8-11) for noncomparative studies. All 9 studies had a high risk of bias. The corresponding values for each study are shown in Table 2.
Patient Characteristics
This systematic review included 215 knees in 215 patients who underwent LMPR repair and ACLR (Table 3). There were 139 (64.7%) men and 76 (35.3%) women with a mean age of 28.7 years (range, 24.6-34.5 years) across all studies. Six studies reported the time from injury to initial surgery with a mean value of 13.0 months (range, 3.3-40.8 months). 2,3,18,27,30,32 The mean clinical follow-up period was 33.9 months (range, 9.9-70.5 months).
Table 3.
Patient Characteristics a
| Lead Author | Surgical Technique | No. of Patients | Sex (F/M) | Age (y) | Time From Injury to Surgery (mo) | Clinical Follow-up (mo) | Tear Pattern of the LMPR (unknown/P1/P2/P3) b |
|---|---|---|---|---|---|---|---|
| Ahn 2 | SSS | 25 | 3/22 | 28.8 (15-58) | 40.8 (0.2-216) | 18.0 (12-48) | 0/7/8/10 |
| Anderson 3 | SSS | 8 | 3/5 | 29.0 (16-58) | 22.4 (0.1-216) | 70.5 (29-168) | 0/8/0/0 |
| POS | 16 | 4/12 | 32.8 (17-59) | 22.4 (0.1-216) | 53.6 (26-116) | 0/0/0/16 | |
| Song 27 | SSS | 15 | 3/12 | 34.5 (18-56) | 3.3 (1.5-12) | 24.0 (12-46) | 0/5/10/0 |
| Zhuo 32 | SSS | 26 | 7/19 | 25.4 (17-39) | 3.4 ± 4.2 | 26.7 (24-36) | 0/26/0/0 |
| Tsujii 30 | SSS | 41 | 23/18 | 29.5 (14-57) | 4.2 (0.9-37.5) | 40.8 (24-75.6) | 0/41/0/0 |
| LaPrade 13 | POS | 10 | 4/6 | 32.2 (19.7-52.7) | NA | 30.0 (24-51.6) | 0/8/1/0 |
| Krych 10 | POS | 26 | 9/17 | 24.6 | NA | 41.0 (24-NA) | 26/0/0/0 |
| Okazaki 18 | SSS | 8 | 4/4 | 27.0 ± 5.8 | 3.3 ± 3.8 | 10.0 ± 3.7 | 0/2/1/5 |
| POS | 9 | 6/3 | 30.1 ± 11.8 | 3.9 ± 6.0 | 9.9 ± 3.2 | 0/3/1/5 | |
| Pan 20 | POS | 31 | 10/21 | 28.0 ± 10.0 | NA | 37.2 (24-NA) | 0/31/0/0 |
| Overall | SSS/POS | 215 | 76/139 | 28.7 | 13.0 | 33.9 | 26/131/21/37 |
| SSS | 123 | 43/80 | 28.9 | 12.5 | 31.1 | 0/89/19/15 | |
| POS | 92 | 33/59 | 28.5 | 15.7 | 37.7 | 26/42/2/22 |
a F, female; LMPR, lateral meniscus posterior root; M, male; NA, not available; POS, pullout suture; SSS, side-to-side suture.
b P1 (pattern 1), radial tears; P2 (pattern 2), longitudinal or T-shaped tears; P3 (pattern 3), avulsed tears (aka root avulsion).
The morphology of tears of the LMPR was documented in 189 patients from 8 studies. 2,3,13,18,20,27,30,32 According to the classification systems introduced by LaPrade et al 11 and Ahn et al 2 for meniscal root tears, tear patterns of the LMPR in this systematic review were summarized as follows (Table 3): pattern 1, radial tears (131/189; 69.3%); pattern 2, longitudinal or T-shaped tears (21/189; 11.1%); and pattern 3, avulsed tears (aka root avulsion) (37/189; 19.6%). No partial tears were included in original studies.
The integrity of the meniscofemoral ligament was assessed in 25 and 17 patients from 2 studies, 2,18 with incidence rates of meniscofemoral ligament tears of 8% and 41%, respectively.
Surgical Technique
A total of 128 autologous hamstring ACLRs and 25 bone–patellar tendon–bone ACLRs were performed among the included studies; the specific techniques of the remaining 62 ACLRs were not described. There were mainly 2 surgical techniques applied in LMPR repairs (Table 4). The side-to-side suture repair (n = 123) was performed in radial tears with a root remnant of adequate tissue quality. 2,3,18,27,30,32 The pullout suture repair (n = 92) was conducted in root avulsions and radial tears of an inadequate meniscal remnant, which included 56 repairs using the same tibial tunnel of ACLR and 36 repairs drilling an additional tunnel at the anatomic attachment of the LMPR. 3,10,13,18,20
Table 4.
Surgical Technique a
| Study | No. of Patients | ACL Reconstruction | LMPR Repair | ||
|---|---|---|---|---|---|
| Graft Choice | Bundle Option | Suture Technique | Pullout Tunnel | ||
| Ahn 2 | 25 | HST | SB | SSS | Not needed |
| Song 27 | 15 | HST | SB | SSS | Not needed |
| Anderson 3 | 8 | HST | SB | SSS | Not needed |
| 16 | HST | SB | POS | ACL tunnel | |
| Tsujii 30 | 16 | HST | TB | SSS | Not needed |
| 25 | BPTB | Rectangular | SSS | Not needed | |
| Zhuo 32 | 26 | NA | NA | SSS | Not needed |
| Okazaki 18 | 8 | HST | DB | SSS | Not needed |
| 9 | HST | DB | POS | ACL tunnel | |
| Pan 20 | 31 | HST | DB | POS | ACL tunnel |
| LaPrade 13 | 10 | NA | NA | POS | Additional tunnel |
| Krych 10 | 26 | NA | NA | POS | Additional tunnel |
a ACL, anterior cruciate ligament; BPTB, bone–patellar tendon–bone; DB, double bundle; HST, hamstring tendon; LMPR, lateral meniscus posterior root; NA, not available; POS, pullout suture; SB, single bundle; SSS, side-to-side suture; TB, triple bundle.
Clinical Outcomes
Overall, 5 different functional scores were utilized (Table 2): the Lysholm score (7 studies 2,3,10,13,20,27,32 ), IKDC subjective score (6 studies 2,3,10,18,20,32 ), Tegner score (5 studies 3,10,13,27,32 ), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) score (1 study 13 ), and 12-Item Short Form Health Survey (SF-12) score (1 study 13 ).
All but 1 of these studies showed significant improvements (P < .05) in each functional score at the final follow-up compared with the preoperative status (Table 5), including the mean Lysholm score (from 58.3 to 91.4), the mean IKDC subjective score (from 61.1 to 87.2), and the Tegner score (from 2.5 to 6.0). The other 2 scores were used in only a single study. 13 They were the WOMAC score (from 52 to 10) and the SF-12 score (from 33.6 to 49.8).
Table 5.
Functional Scores a
| Study | Surgical Technique (n) | Mean Lysholm Score | Mean IKDC Subjective Score | Mean Tegner Score | |||
|---|---|---|---|---|---|---|---|
| Pre- | Post- | Pre- | Post- | Pre- | Post- | ||
| Ahn 2 | SSS (25) | 62.3 ± 17.3 | 92.9 ± 3.4 b | 67.0 ± 15.6 | 90.2 ± 7.3 b | NA | NA |
| Anderson 3 | SSS (8) | NA | 86.9 ± 5.7 b | NA | 81.6 ± 6.8 b | NA | 6.0 ± 1.3 b |
| POS (16) | NA | 86.1 ± 6.5 b | NA | 84.3 ± 8.3 b | NA | 6.7 ± 1.2 b | |
| Song 27 | SSS (15) | 68.9 ± 4.3 | 95.6 ± 3.5 b | NA | NA | 3.1 ± 0.8 | 6.7 ± 1.4 b |
| Zhuo 32 | SSS (26) | 56.3 ± 4.6 | 95.1 ± 2.9 b | 53.4 ± 5.3 | 92.1 ± 2.6 b | 2.4 ± 0.6 | 5.6 ± 0.6 b |
| LaPrade 13 | POS (10) | 35.0 | 75.0 b | NA | NA | 2.0 | 4.0 b |
| Krych 10 | POS (26) | NA | 93.9 b | NA | 89.5 b | NA | 6.5 b |
| Okazaki 18 | SSS (8) | NA | NA | 63.3 ± 18.3 | 73.0 ± 17.7 | NA | NA |
| POS (9) | NA | NA | 61.7 ± 18.4 | 70.7 ± 16.8 | NA | NA | |
| Pan 20 | POS (31) | 59.0 ± 19.1 | 92.3 ± 6.3 b | 62.1 ± 19.2 | 90.1 ± 8.6 b | NA | NA |
| Overall | 174 SSS/POS | 58.3 | 91.4 | 61.1 | 87.2 | 2.5 | 6.0 |
| 82 SSS | 61.4 | 93.6 | 60.5 | 87.9 | 2.7 | 6.0 | |
| 92 POS | 53.1 | 89.5 | 62.0 | 86.6 | 2.0 | 6.1 | |
a IKDC, International Knee Documentation Committee; NA, not available; POS, pullout suture; post-, postoperative; pre-, preoperative; SSS, side-to-side suture.
b Significant difference (P < .05) compared with preoperative status.
A total of 82 patients from 3 studies were evaluated for knee stability, and all of them showed a negative Lachman or pivot-shift test at the final follow-up. 3,18,30 A cohort study reported no significant side-to-side differences in the KT-1000 between knees with LMPR repairs and those with an intact meniscus at 3 years after ACLR. 30
Radiographic Outcomes
Radiographic evaluations were performed in 6 studies, including 1 weightbearing AP radiograph analysis on joint space width, 30 1 MRI investigation on chondral status, 20 3 MRI studies on meniscal extrusion, 2,18,30 and 2 MRI reports on meniscal healing 3,32 (Table 6). No study reported the ACL graft integrity based on follow-up MRI.
Table 6.
Radiographic Evaluations a
| Study | Surgical Technique (n) b | Method | Measure | Radiographic Follow-up (mo) | Results | Significance |
|---|---|---|---|---|---|---|
| Okazaki 18 | SSS (8) | MRI | Meniscal extrusion | 10.0 | Coronal: increased by 1.0 ± 0.9 mm | Yes c |
| POS (9) | MRI | Meniscal extrusion | 9.9 | Coronal: decreased by 0.5 ± 0.7 mm | ||
| Ahn 2 | SSS (18) | MRI | Meniscal extrusion | 8.7 |
Coronal: decreased by 0.39 ± 1.13 mm; Sagittal: decreased by 1.75 ± 2.52 mm |
No; yes d |
| Tsujii 30 | SSS (41) | MRI | Meniscal extrusion | 40.8 |
Coronal: decreased by 0.16 ± 0.88 mm; Sagittal: increased by 1.22 ± 1.54 mm |
No |
| CR | Joint space width | 40.8 | Decreased by 0.04 ± 0.8 mm | Yes d ; no | ||
| Pan 20 | POS (31) | MRI | Chondral status | 37.2 | Post: 81% normal, 16% mild, 3% moderate | No |
| Zhuo 32 | SSS (26) | MRI | Meniscal healing | 26.7 | 96% complete healing, 4% failure to heal | NA |
| Anderson 3 | POS (3) | MRI | Meniscal healing | 25.3 | 100% complete healing | NA |
a CR, conventional radiograph; MRI, magnetic resonance imaging; NA, not available; POS, pullout suture; post, postoperative; SSS, side-to-side suture.
b Number of patients who underwent radiographic evaluations.
c Significant difference (P < .05) between different repair techniques.
d Significant difference (P < .05) between pre- and postoperative values.
In 1 study, weightbearing AP radiographs showed no significant narrowing (0.04 mm) of lateral joint space width in patients undergoing side-to-side repairs for tears of the LMPR. 30 In another study, the chondral status on MRI scans after LMPR pullout repairs was rated as normal in 81% of patients, mild in 16% of patients, and moderate in 3% patients, none of which was significantly different from their preoperative status. 20
The results of lateral meniscal extrusion were reported in 3 studies. 2,18,30 There were no significant reductions of coronal extrusion after LMPR repairs in all 3 studies, but 1 comparative study among them showed significantly greater decreases of coronal extrusion after pullout repairs than after side-to-side repairs. 18 In 2 studies repairing radial tears of the LMPR by the side-to-side suture technique, the sagittal extrusion increased in 1 study but decreased in the other. 2,30
The LMPR signal on follow-up MRI was reported in 2 studies. 3,32 Twenty-five side-to-side repairs as well as 3 pullout repairs achieved complete meniscal healing, and only 1 patient undergoing the LMPR side-to-side repair was evaluated with an abnormal hyperintense signal in the repaired site.
Arthroscopic Outcomes
At the time of tibial hardware (for ACL graft) removal, second-look arthroscopy was performed for diagnostic purposes. The healing rate of repaired tears of the LMPR was assessed in 81 patients across 5 studies. 2,3,27,30,32 Meniscal healing status was classified according to consistent criteria in the 5 studies (Table 7). At a mean follow-up of 22.1 months, the healing status was rated as complete in 59 of 81, partial in 17 of 81, and failed in 5 of 81 repairs. The complete/partial healing rate was 93.8%. Specifically, 78 radial tears achieved 93.6% complete or partial healing after side-to-side repairs. All 3 root avulsions completely healed after pullout repairs.
Table 7.
Meniscal Healing on Second-Look Arthroscopy a
| Study | Surgical Technique (n) b | Arthroscopic Follow-up (mo) | Healing Status on Second-Look Arthroscopy, n (%) | ||
|---|---|---|---|---|---|
| Complete Healing c | Partial Healing d | Failure to Heal e | |||
| Ahn 2 | SSS (9) | 21.3 | 8 (88.9) | 1 (11.1) | 0 (0.0) |
| Anderson 3 | SSS (2) | 49.5 | 2 (100.0) | 0 (0.0) | 0 (0.0) |
| POS (3) | 7.3 | 3 (100.0) | 0 (0.0) | 0 (0.0) | |
| Song 27 | SSS (15) | 24.0 | 9 (60.0) | 4 (26.7) | 2 (13.3) |
| Zhuo 32 | SSS (22) | 13.0 | 19 (86.4) | 3 (13.6) | 0 (0.0) |
| Tsujii 30 | SSS (30) | 27.6 | 18 (60.0) | 9 (30.0) | 3 (10.0) |
| Overall | 81 SSS/POS | 22.1 | 59 (72.8) | 17 (21.0) | 5 (6.2) |
| 78 SSS | 22.6 | 56 (71.8) | 17 (21.8) | 5 (6.4) | |
| 3 POS | 7.3 | 3 (100.0) | 0 (0.0) | 0 (0.0) | |
a POS, pullout suture; SSS, side-to-side suture.
b Number of patients who underwent second-look arthroscopy for meniscal healing evaluations.
c Number of patients with complete healing, no visible surface defect with complete synovial coverage.
d Number of patients with partial healing, a small defect with synovial coverage over more than half of the torn area.
e Number of patients with failure to heal, a large defect with synovial coverage over less than half of the torn area.
The chondral status was evaluated arthroscopically in 1 study, and a significant progression of chondral lesions was found in the lateral tibial plateau at 27.6 months after side-to-side repairs for radial tears of the LMPR. 30
None of the included studies evaluated the ACL graft status arthroscopically.
Discussion
Despite variable outcome measures, the most important findings of this systematic review could be summarized as follows. Patients with tears of the LMPR associated with ACL injuries obtained favorable functional scores after ACLR and simultaneous LMPR repairs. Moreover, most patients in whom meniscal healing was evaluated based on second-look arthroscopy were treated with side-to-side repairs for radial tears, and the complete/partial healing rate was >90%. Additionally, with inconsistent radiographic and arthroscopic results, we were unable to definitively conclude whether LMPR repairs fully restore the hoop stress of the lateral meniscus.
Of late, the management of concomitant tears of the LMPR in ACL injuries has been a hot topic in the field of sports medicine. Authors of previous studies chose to leave the root tear in situ during ACLR. 14,22 In a study by Shelbourne et al, 22 despite improved functional scores, the midterm radiographic follow-up results showed significant progression of lateral joint space narrowing in patients with tears of the LMPR being left in situ compared with those without meniscal lesions. Lee et al 14 left radial tears of the LMPR in situ in 27 patients undergoing ACLR; however, the meniscal healing rate was only 75%. Therefore, there has been great interest regarding surgical repairs of tears of the LMPR. 2,3,10,13,20,27,30
A critical issue for successful repair of tears of the LMPR is proper surgical technique, and meniscal extrusion is a common and objective outcome to measure postsurgical meniscal function. 1,15,18 Currently, there are 2 surgical techniques with clinical follow-up records. The side-to-side technique can be used to repair radial tears with a root remnant of adequate tissue quality. 2,30 For cases of root avulsions or radial tears with tissue remnant of questionable quality, a transtibial pullout repair is recommended. 10,13 Okazaki et al 18 compared the efficacy of the 2 techniques in treating tears of the LMPR associated with ACL injury and found that pullout repair is better in decreasing the lateral meniscal extrusion on the coronal plane than the side-to-side technique but in a relatively short follow-up period (10 months). Meanwhile, Ahn et al 2 and Tsujii et al 30 reported no significant reduction of coronal extrusion after side-to-side repairs. Such findings indicate that extrusion reduction after LMPR repairs might not necessarily be satisfactory, but the pullout repair is likely better for the restoration of the hoop tension of the lateral meniscus. The effect of differences in repair techniques on extrusion reduction should be evaluated in a longer follow-up duration.
Although there is a broad consensus that a tear of the LMPR should be surgically repaired if confirmed during ACLR, the effectiveness of LMPR repairs still requires justification from multiple aspects. For the clinical outcomes, this systematic review showed consistent improvements in all functional scores. The preoperative Lysholm score in 7 of the 9 included studies was around 60, which was considered to be poor and indicated severe symptoms in patients with tears of the LMPR and ACL injuries. After meniscal repair and ACLR, the mean score improved to approximately 90, indicating a significant advancement in subjective symptoms and daily activity. Such improvements were also found in terms of the IKDC subjective score and the Tegner score. Meanwhile, no residual knee mechanical instability was reported at the final follow-up. 3,18,30 However, because of the lack of a control group, there is no clear evidence that repairing tears of the LMPR in ACL-reconstructed knees would lead to better clinical outcomes than leaving them unrepaired.
Regarding the radiographic outcomes, a total of 72 patients showed no significant progression of joint space narrowing or chondral lesions of the lateral tibiofemoral compartment after tears of the LMPR were repaired during ACLR. Tsujii et al 30 found that the lateral joint space width was decreased by only 0.04 mm at a mean 3.4 years after LMPR repairs, and the amount of change was similar to that in isolated ACL-injured knees. Pan et al 20 reported that the postoperative chondral status was normal in 81% of patients after a mean follow-up of 3.1 years. In patients with tears of the LMPR left in situ, though, the significantly progressed lateral compartment narrowing was up to 1.0 mm, 22 and the postoperative chondral status was inferior to that in patients with repaired tears of the LMPR. 20 Such radiographic results supported the necessity of surgical repairs in terms of preventing premature osteoarthritis. However, arthroscopic results from the study of Tsujii et al 30 showed significantly progressed chondral lesions in the lateral tibial plateau after side-to-side repairs for tears of the LMPR, indicating that the hoop tension of the lateral meniscus might be not fully restored after LMPR repairs. Therefore, cartilaginous degeneration might progress after surgeries.
The healing capacity of surgically repaired tears of the LMPR is another important issue. In this systematic review, 78 patients who received the side-to-side repair for radial tears of the LMPR were evaluated for meniscal healing during the second-look arthroscopy. The overall healing rate of radial tears of the LMPR was 93.6%, which was more favorable compared with that of midbody radial tears of the lateral meniscus (61%). 29 Although the capacity of radial tears to heal was low, the bone marrow bleeding from bone tunnels during ACLR may have promoted the healing process of meniscal repair, which provided a favorable environment for meniscal healing. 27,30
Several clinical studies showed that a tear of the LMPR would further destabilize the ACL-injured knee under pivot-shift loading. 16,25 However, the included studies failed to provide enough information about the restoration of anterolateral rotational stability after LMPR repairs and combined ACLR. Despite the inspiring results provided by laboratory trials, 8,28 future studies are necessary to evaluate the effectiveness of LMPR repairs in controlling the dynamic stability of ACL-reconstructed knees in clinical scenarios.
The limitations of this systematic review were largely the result of the included studies. First, the low level of evidence and inconsistent reports of outcome measures is notable. Second, different tear patterns of the LMPR (radial/longitudinal tears near the root and root avulsions) were not clearly separated, and these are clinically unique because of anatomic characteristics and repair techniques. Third, the difference in surgical techniques of ACLR rather than LMPR repair may have a greater influence on postoperative knee stability; however, such an effect has not been clarified in this review due to the limited data available in the original studies, and it awaits further research. Despite these limitations, to our knowledge, this is the first study to systematically review clinical, radiographic, and arthroscopic results of surgical repairs for tears of the LMPR in patients undergoing ACLR. As such, this study could be helpful in directing future studies as the role of LMPR repair in ACLR is explored.
Conclusion
Despite variable outcome measures in this systematic review, patients with tears of the LMPR associated with ACL injuries obtained favorable functional scores after ACLR and simultaneous LMPR repairs, and the side-to-side repair for radial tears of the LMPR achieved a high meniscal healing rate of >90%. However, with inconsistent radiographic and arthroscopic results, we are unable to definitively conclude whether LMPR repairs can fully restore the hoop stress of the lateral meniscus.
Footnotes
Final revision submitted August 14, 2020; accepted October 28, 2020.
One or more of the authors has declared the following potential conflict of interest or source of funding: G.S. has received funding from the National Natural Science Foundation of China (82002288) and the Beijing Talent Work Foundation (2018000021469G227). Y.L. has received funding from the Beijing Natural Science Foundation (7194276) and the Beijing Talent Work Foundation (2018000021469G224). H.Z. has received funding from the Beijing Natural Science Foundation (L192051) and the Capital's Funds for Health Improvement and Research (CFH2020-2-2075). H.F. has received funding from the Capital's Funds for Health Improvement and Research (CFH2020-1-2071). AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Ahn JH, Kang HW, Yang TY, Lee JY. Multivariate analysis of risk factors of graft extrusion after lateral meniscus allograft transplantation. Arthroscopy. 2016;32(7):1337–1345. [DOI] [PubMed] [Google Scholar]
- 2. Ahn JH, Lee YS, Yoo JC, Chang MJ, Park SJ, Pae YR. Results of arthroscopic all-inside repair for lateral meniscus root tear in patients undergoing concomitant anterior cruciate ligament reconstruction. Arthroscopy. 2010;26(1):67–75. [DOI] [PubMed] [Google Scholar]
- 3. Anderson L, Watts M, Shapter O, et al. Repair of radial tears and posterior horn detachments of the lateral meniscus: minimum 2-year follow-up. Arthroscopy. 2010;26(12):1625–1632. [DOI] [PubMed] [Google Scholar]
- 4. Bao HR, Zhu D, Gong H, Gu GS. The effect of complete radial lateral meniscus posterior root tear on the knee contact mechanics: a finite element analysis. J Orthop Sci. 2013;18(2):256–263. [DOI] [PubMed] [Google Scholar]
- 5. Feucht MJ, Salzmann GM, Bode G, et al. Posterior root tears of the lateral meniscus. Knee Surg Sports Traumatol Arthrosc. 2015;23(1):119–125. [DOI] [PubMed] [Google Scholar]
- 6. Forkel P, Herbort M, Sprenker F, Metzlaff S, Raschke M, Petersen W. The biomechanical effect of a lateral meniscus posterior root tear with and without damage to the meniscofemoral ligament: efficacy of different repair techniques. Arthroscopy. 2014;30(7):833–840. [DOI] [PubMed] [Google Scholar]
- 7. Forkel P, Reuter S, Sprenker F, et al. Different patterns of lateral meniscus root tears in ACL injuries: application of a differentiated classification system. Knee Surg Sports Traumatol Arthrosc. 2015;23(1):112–118. [DOI] [PubMed] [Google Scholar]
- 8. Forkel P, von Deimling C, Lacheta L, et al. Repair of the lateral posterior meniscal root improves stability in an ACL-deficient knee. Knee Surg Sports Traumatol Arthrosc. 2018;26(8):2302–2309. [DOI] [PubMed] [Google Scholar]
- 9. Geeslin AG, Civitarese D, Turnbull TL, Dornan GJ, Fuso FA, LaPrade RF. Influence of lateral meniscal posterior root avulsions and the meniscofemoral ligaments on tibiofemoral contact mechanics. Knee Surg Sports Traumatol Arthrosc. 2016;24(5):1469–1477. [DOI] [PubMed] [Google Scholar]
- 10. Krych AJ, Bernard CD, Kennedy NI, et al. Medial versus lateral meniscus root tears: is there a difference in injury presentation, treatment decisions, and surgical repair outcomes? Arthroscopy. 2020;36(4):1135–1141. [DOI] [PubMed] [Google Scholar]
- 11. LaPrade CM, James EW, Cram TR, Feagin JA, Engebretsen L, LaPrade RF. Meniscal root tears: a classification system based on tear morphology. Am J Sports Med. 2015;43(2):363–369. [DOI] [PubMed] [Google Scholar]
- 12. LaPrade CM, Jansson KS, Dornan G, Smith SD, Wijdicks CA, LaPrade RF. Altered tibiofemoral contact mechanics due to lateral meniscus posterior horn root avulsions and radial tears can be restored with in situ pull-out suture repairs. J Bone Joint Surg Am. 2014;96(6):471–479. [DOI] [PubMed] [Google Scholar]
- 13. LaPrade RF, Matheny LM, Moulton SG, James EW, Dean CS. Posterior meniscal root repairs: outcomes of an anatomic transtibial pull-out technique. Am J Sports Med. 2017;45(4):884–891. [DOI] [PubMed] [Google Scholar]
- 14. Lee DW, Jang HW, Lee SR, Park JH, Ha JK, Kim JG. Clinical, radiological, and morphological evaluations of posterior horn tears of the lateral meniscus left in situ during anterior cruciate ligament reconstruction. Am J Sports Med. 2014;42(2):327–335. [DOI] [PubMed] [Google Scholar]
- 15. Matsuo T, Kinugasa K, Sakata K, Ohori T, Mae T, Hamada M. Post-operative deformation and extrusion of the discoid lateral meniscus following a partial meniscectomy with repair. Knee Surg Sports Traumatol Arthrosc. 2017;25(2):390–396. [DOI] [PubMed] [Google Scholar]
- 16. Minami T, Muneta T, Sekiya I, et al. Lateral meniscus posterior root tear contributes to anterolateral rotational instability and meniscus extrusion in anterior cruciate ligament-injured patients. Knee Surg Sports Traumatol Arthrosc. 2018;26(4):1174–1181. [DOI] [PubMed] [Google Scholar]
- 17. Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement. J Clin Epidemiol. 2009;62(10):1006–1012. [DOI] [PubMed] [Google Scholar]
- 18. Okazaki Y, Furumatsu T, Kamatsuki Y, et al. Transtibial pullout repair of the lateral meniscus posterior root tear combined with anterior cruciate ligament reconstruction reduces lateral meniscus extrusion: a retrospective study. Orthop Traumatol Surg Res. 2020;106(3):469–473. [DOI] [PubMed] [Google Scholar]
- 19. Pache S, Aman ZS, Kennedy M, et al. Meniscal root tears: current concepts review. Arch Bone Jt Surg. 2018;6(4):250–259. [PMC free article] [PubMed] [Google Scholar]
- 20. Pan F, Hua S, Ma Z. Surgical treatment of combined posterior root tears of the lateral meniscus and ACL tears. Med Sci Monit. 2015;21:1345–1349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Perez-Blanca A, Espejo-Baena A, Amat Trujillo D, et al. Comparative biomechanical study on contact alterations after lateral meniscus posterior root avulsion, transosseous reinsertion, and total meniscectomy. Arthroscopy. 2016;32(4):624–633. [DOI] [PubMed] [Google Scholar]
- 22. Shelbourne KD, Roberson TA, Gray T. Long-term evaluation of posterior lateral meniscus root tears left in situ at the time of anterior cruciate ligament reconstruction. Am J Sports Med. 2011;39(7):1439–1443. [DOI] [PubMed] [Google Scholar]
- 23. Shybut TB, Vega CE, Haddad J, et al. Effect of lateral meniscal root tear on the stability of the anterior cruciate ligament-deficient knee. Am J Sports Med. 2015;43(4):905–911. [DOI] [PubMed] [Google Scholar]
- 24. Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological Index for Non-Randomized Studies (MINORS): development and validation of a new instrument. ANZ J Surg. 2003;73(9):712–716. [DOI] [PubMed] [Google Scholar]
- 25. Song GY, Zhang H, Liu X, et al. Complete posterolateral meniscal root tear is associated with high-grade pivot-shift phenomenon in noncontact anterior cruciate ligament injuries. Knee Surg Sports Traumatol Arthrosc. 2017;25(4):1030–1037. [DOI] [PubMed] [Google Scholar]
- 26. Song G-Y, Zhang J, Li X, Li Y, Feng H. Current concepts on posterior meniscal root lesion: a treatment algorithm based on the currently available evidence. Asia Pac J Sports Med Arthrosc Rehab Tech. 2014;1(3):81–89. [Google Scholar]
- 27. Song HS, Bae TY, Park BY, Shim J, In Y. Repair of a radial tear in the posterior horn of the lateral meniscus. Knee. 2014;21(6):1185–1190. [DOI] [PubMed] [Google Scholar]
- 28. Tang X, Marshall B, Wang JH, et al. Lateral meniscal posterior root repair with anterior cruciate ligament reconstruction better restores knee stability. Am J Sports Med. 2019;47(1):59–65. [DOI] [PubMed] [Google Scholar]
- 29. Tsujii A, Amano H, Tanaka Y, et al. Second look arthroscopic evaluation of repaired radial/oblique tears of the midbody of the lateral meniscus in stable knees. J Orthop Sci. 2018;23(1):122–126. [DOI] [PubMed] [Google Scholar]
- 30. Tsujii A, Yonetani Y, Kinugasa K, et al. Outcomes more than 2 years after meniscal repair for radial/flap tears of the posterior lateral meniscus combined with anterior cruciate ligament reconstruction. Am J Sports Med. 2019;47(12):2888–2894. [DOI] [PubMed] [Google Scholar]
- 31. Zheng T, Song GY, Feng H, et al. Lateral meniscus posterior root lesion influences anterior tibial subluxation of the lateral compartment in extension after anterior cruciate ligament injury. Am J Sports Med. 2020;48(4):838–846. [DOI] [PubMed] [Google Scholar]
- 32. Zhuo H, Chen Q, Zhu F, Li J. Arthroscopic side-to-side repair for complete radial posterior lateral meniscus root tears. BMC Musculoskelet Disord. 2020;21(1):130. [DOI] [PMC free article] [PubMed] [Google Scholar]