Abstract
Summary: Moyamoya disease is infrequently associated with intracranial aneurysms arising from the circle of Willis vessels or from “peripheral” branches of choroidal and meningeal vessels. We present a rare case of a moyamoya-related aneurysm arising along the dural junction of multiple meningeal branches from the external carotid artery causing intracerebral hemorrhage. Endovascular coil embolization of the middle meningeal artery (MMA) and occipital artery (OA) led to delayed aneurysm obliteration without rehemorrhage.
Moyamoya disease is infrequently accompanied by intracranial aneurysms, with an incidence of 3–14% (1). These aneurysms most commonly originate from the circle of Willis, moyamoya vessels (lenticulostriates) to the basal ganglia, or collaterals via the anterior or posterior choroidal vessels, with a distribution of approximately 3:1:1, respectively (2). The latter two categories of aneurysms, termed “peripheral artery aneurysms,” cause either intraventricular hemorrhage or intracerebral hematoma and have a poor prognosis when left untreated because of rebleeding (3). Treatment options to prevent rebleeding from moyamoya-related aneurysms include direct obliteration of a saccular aneurysm via surgical or endovascular means, parent vessel sacrifice, and/or revascularization to reduce hemodynamic stress on collateral vessels (2–7). We report the first case—to our knowledge—of a moyamoya-associated aneurysm arising from the dural-based junction of middle meningeal artery (MMA) and occipital artery (OA) collaterals causing intracerebral hematoma.
Case Report
A 31 year-old woman with a history of Down syndrome and prior right frontoparietal infarct due to moyamoya disease presented with headache and decreased appetite. She was awake with residual left hemiplegia due to prior cerebral infarct, but without new motor/sensory deficits, and it was unclear whether she had a visual field deficit. CT scanning revealed a left occipito-parietal intracerebral hematoma with intraventricular hemorrhage extension (Fig 1). A cerebral arteriogram demonstrated a 3-mm aneurysm arising at the junction of collateral branches between the left MMA and OA (Fig 2A and B). Superselective catheterization of both the left MMA and the left OA was performed (Fig 2C and D). Multiple platinum coils were deposited as distal as possible to occlude the parent branching vessels, resulting in delayed flow filling the aneurysm from a small external carotid artery branch that could not be catheterized (Fig 2E). The patient recovered to baseline neurologic function at follow-up examination 2 months after embolization, and repeat angiography showed complete aneurysm thrombosis (Fig 2F).
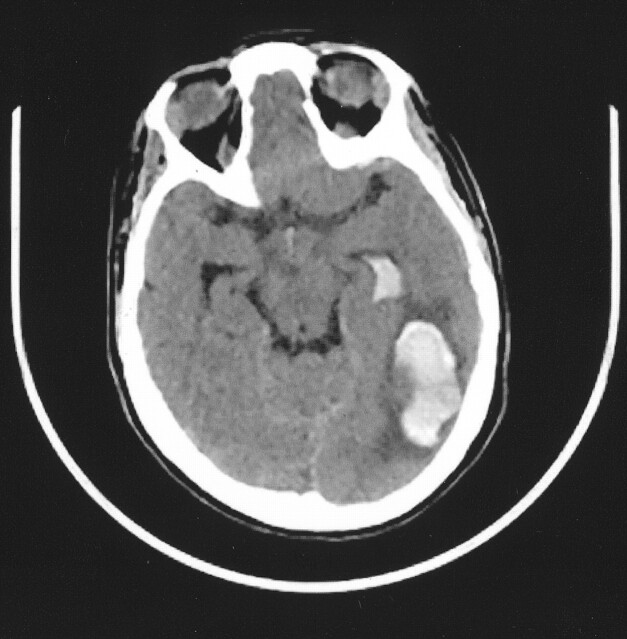
Fig 1.
CT scan, showing left occipito-parietal hematoma with intraventricular hemorrhage.
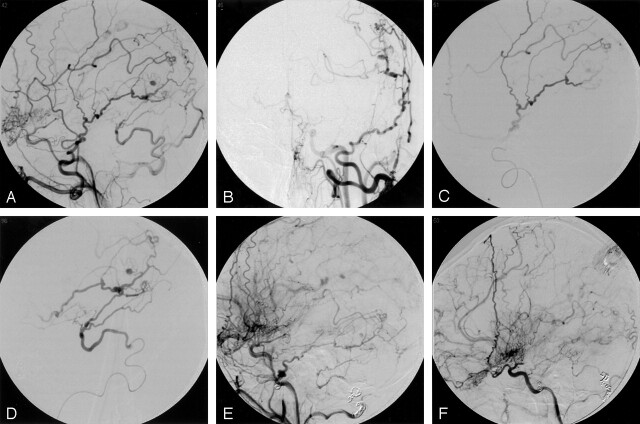
Fig 2.
A and B, Left common carotid artery lateral and AP arteriogram, demonstrating a 3-mm aneurysm arising near collateral branches of the MMA and OA.
C, Superselective arteriogram of the MMA, demonstrating supply to the aneurysm
D, Superselective arteriogram of the OA, demonstrating supply to the aneurysm.
E, Left external carotid arteriogram, lateral view, demonstrating coil deposition in the MMA and OA with delayed aneurysm filling from a small external carotid artery branch unable to be catheterized.
F, Two-month follow-up left external carotid arteriogram, showing complete obliteration of the aneurysm.
Discussion
Aneurysms were first described in association with moyamoya disease by Pool et al in 1967 (8). Adult patients with moyamoya disease present with intracranial hemorrhage either due to rupture of a true saccular aneurysm or from “pseudoaneurysms” secondary to the fragility of the moyamoya vessels under profound hemodynamic stress (9). Rebleeding occurs in 20–30% of patients and is associated with poor outcomes. Thus, prevention of rebleeding is crucial (3). Revascularization procedures have been performed to reduce the hemodynamic load on the fragile moyamoya vessels and thus prevent rebleeding (5). Yoshida et al (3) compared long-term control of rebleeding following revascularization procedures and found the rebleeding rate was lower in the surgical group than that in the nonsurgical control group.
Our case is unique in that it is, to our knowledge, the first reported case of an aneurysm in a patient with moyamoya disease arising from the dural-based junction between collateral branches of the MMA and OA causing an intracerebral hematoma. One previous series reports two moyamoya-associated aneurysms found incidentally without hemorrhage in the same patient at anastomses between the MMA and the internal carotid artery near the sella and between the MMA and anterior cerebral artery over the convexity (10). Ushikoshi et al (11) reported an aneurysm formed on a collateral MMA branch providing blood flow to the posterior cerebral artery (PCA) territory following spontaneous PCA occlusion in a patient with severe atherosclerotic disease that was managed by aneurysm occlusion and resection. Aneurysm obliteration may be performed by direct surgical clipping, surgical trapping of the parent vessel, or endovascular embolization. Without therapy, spontaneous regression is possible. A distal lenticulostriate aneurysm in a moyamoya patient with intracerebral hemorrhage managed by clot removal without revascularization or aneurysm obliteration nearly disappeared 3 weeks later (12). A retrospective review of 111 adult moyamoya patients with 131 aneurysms suggests that aneurysms from the lenticulostriate or distal collateral vessels disappear spontaneously and may not warrant direct surgical intervention (2). Although these peripheral aneurysms are often dismissed as pseudoaneurysms, Lee et al (6) provided histologic confirmation of a true aneurysm along the distal anterior choroidal artery that was successfully trapped and resected surgically. Other patients have true saccular aneurysms of the circle of Willis that should be treated by aneurysm obliteration (7). Hamada et al (4) recommend performing both aneurysm obliteration and cerebral revascularization at the same time in patients in whom the parent vessel is an important collateral source but must be occluded to eliminate the aneurysm from the circulation.
In view of the rare nature of aneurysms associated with moyamoya disease, no clear guidelines exist regarding which aneurysms are best treated by surgical or endovascular means or managed conservatively. An endovascular approach was selected in this case to spare inadvertent loss of collateral supply from meningeal arteries that may have been cut during a surgical procedure. We acknowledge the use of “glue” embolic agents may have provided a more complete distal embolization than we achieved with coils; however, the treatment goal of preventing rehemorrhage without procedural morbidity was achieved. Our case report describes the rare location of a moyamoya-associated aneurysm arising at the dural-based junction of MMA and OA collateral branches causing intracerebral hemorrhage.
References
- 1.Borota L, Marinkovic S, Kovacevic M. Intracranial aneurysms associated with moyamoya disease. Neurol Med Chir (Tokyo) 1996;36:860–864 [DOI] [PubMed] [Google Scholar]
- 2.Kawagushi S, Sakaki T, Morimoto T, et al. Characteristics of intracranial aneurysms associated with moyamoya disease: a review of 111 cases. Acta Neurochir (Wien) 1996;138:1287–1294 [DOI] [PubMed] [Google Scholar]
- 3.Yoshida Y, Yoshimoto T, Shirane R, Sakurai Y. Clinical course, surgical management, and long-term outcome of moyamoya patients with rebleeding after an episode of intracerebral hemorrhage. Stroke 1999;30:2272–2276 [DOI] [PubMed] [Google Scholar]
- 4.Hamada J-I, Hashimoto N, Tsukahara T. Moyamoya disease with repeated intraventricular hemorrhage due to aneurysm rupture. J Neurosurg 1994;80:328–331 [DOI] [PubMed] [Google Scholar]
- 5.Kuroda S, Houkin K, Kamiyama H, Abe H. Effects of surgical revascularization on peripheral artery aneurysms in moyamoya disease: report of three cases. Neurosurgery 2001;49:463–468 [DOI] [PubMed] [Google Scholar]
- 6.Lee J, Lee J, Kim S, Lee M. Distal anterior choroidal artery aneurysm in a patient with moyamoya disease: case report. Neurosurgery 2001;48:222–225 [DOI] [PubMed] [Google Scholar]
- 7.Nagamine Y, Takahashi S, Sonobe M. Multiple intracranial aneurysms associated with moyamoya disease. J Neurosurg 1981;54:673–676 [DOI] [PubMed] [Google Scholar]
- 8.Pool JL, Wood EH, Maki Y. On the cases with abnormal vascular network in the cerebral basal region in the United States. In Kudo T, ed. A disease with abnormal intracranial vascular networks: spontaneous occlusion of the circle of Willis. Tokyo: Igaku Shoin;1967. :63–68
- 9.Konishi Y, Kadowaki C, Hara M, Takeuchi K. Aneurysms associated with moyamoya disease. Neurosurgery 1985;16:484–490 [PubMed] [Google Scholar]
- 10.Takahashi M. Magnification angiography of cerebral aneurysms associated with moyamoya disease. AJNR Am J Neuroradiol 1980;1:547–550 [Google Scholar]
- 11.Ushikoshi S, Houkin K, Itoh F, et al. Ruptured aneurysm of the middle meningeal artery associated with occlusion of the posterior cerebral artery. J Neurosurg 1996;84:269–271 [DOI] [PubMed] [Google Scholar]
- 12.Grabel JC, Levine M, Hollis P, Ragland R. Moyamoya-like disease associated with a lenticulostriate region aneurysm. J Neurosurg 1989;70:802–803 [DOI] [PubMed] [Google Scholar]