Abstract
Summary: We report the progressive otic capsule demineralization around the membranous labyrinth and facial nerve in an adult patient with osteogenesis imperfecta tarda. Whereas the initial CT scan showed bandlike, undermineralized pericochlear areas, 2 years later, repeat CT performed because of hearing deterioration showed progression of these findings to the promontory, the round window niche, and the labyrinthine and tympanic segments of the facial nerve canal. MR imaging demonstrated enhancement of the abnormal otic capsule and of the intratemporal and canalicular facial nerve. The differential diagnosis of osteogenesis imperfecta tarda affecting the temporal bone includes otosclerosis, Paget disease, otosyphilis, and Camurati-Engelmann disease.
Osteogenesis imperfecta (OI) is a rare genetic disorder of connective tissue that is caused by an error in collagen type I formation (1–4). Mutations on chromosome 17 or chromosome 7 result in a decreased synthesis of structurally normal type I collagen, the synthesis of structurally abnormal type I collagen, or both (1–4). The disease is characterized by abnormal bone fragility, osteopenia, blue color of the sclerae, defective dentition, presenile hearing loss, and ligamentous laxity. The triad of fragile bone, blue sclerae, and progressive hearing impairment was first described by van der Hoeve and de Kleyn in 1917 (5) and was thus named Van der Hoeve-de Kleyn syndrome.
According to Sillence et al (2), there are four major types of OI, ranging from mild to severe. The autosomal dominantly inherited type I, the mildest form—which is frequently called “OI tarda”—is characterized by nondeforming fractures, distinctly blue sclerae, and hearing impairment. Type II with autosomal-recessive inheritance is the most severe form and is almost always lethal in the fetal or perinatal period. Types III and IV are moderate to severe forms with bone deformities, whereas hearing impairment is less common in these types.
The imaging findings of the temporal bone on CT in patients with Van der Hoeve–De Kleyn syndrome have been only rarely described (4, 6–10), and the MR imaging findings have been sporadically reported by only three authors (10–12). To our knowledge, serial imaging studies have never been reported in the literature.
We describe serial CT and MR imaging findings of the temporal bone in a patient with genetically proved Van der Hoeve-de Kleyn syndrome and discuss the key distinguishing features in the radiologic and clinical differential diagnosis.
Case Report
A female patient had several episodes of fractured limbs after minor trauma in her childhood. Family medical history revealed that her mother had a history of recurrent bone fractures. Genetic findings when the patient was 10 years old confirmed the diagnosis of OI type I (2). At 24 years old, she presented with bilateral progressive hearing loss. Clinical examination revealed blue sclerae and loose joints. Otoscopy showed normal tympanic membranes bilaterally. A pure-tone audiogram demonstrated profound sensorineural hearing loss on the right side and severe sensorineural hearing loss on the left side. The conductive hearing and vestibular functions were within the normal range. Tympanometry was normal in both ears. The stapedius reflex could not be elicited. The functions of both facial nerves were normal.
A high-resolution CT scan postprocessed with a bone algorithm and viewed with wide windows at that age showed symmetrical, abnormal bandlike areas of lucency surrounding the cochlea. The facial nerve canal showed minimal irregularities along the labyrinthine segment on both sides, but otherwise appeared normal (Fig 1). When the patient was 26 years old, sensorineural hearing loss on the left side progressed and the conductive hearing functions were additionally impaired on both sides. Facial nerve functions were still normal. A CT scan at that age demonstrated a progression of the bandlike undermineralized pericochlear areas, now extending from the promontory to the apical turn of the cochlea. The round window niche was now filled with thickened and undermineralized bone. Further profound progression was present along the labyrinthine and proximal tympanic segments of the facial nerve canal and in the geniculate gangion, which were indistinct and irregular bilaterally (Fig 2). The mastoid segment of the facial nerve canal was normal.
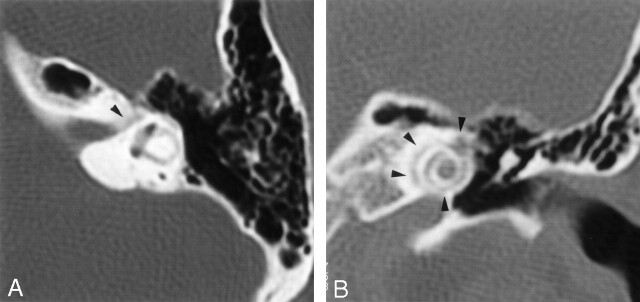
Fig 1.
Initial axial (A) and direct coronal (B) high-resolution CT scans of the temporal bones through the level of the labyrinthine segment of the facial nerve (axial) and the cochlea (coronal) processed with a bone algorithm (2-mm section thickness; 512 × 512 matrix). The facial nerve canal showed slight irregularities along the labyrinthine segment (arrowhead) but otherwise appeared normal. Bandlike, undermineralized areas around the cochlea can be seen (arrowheads).
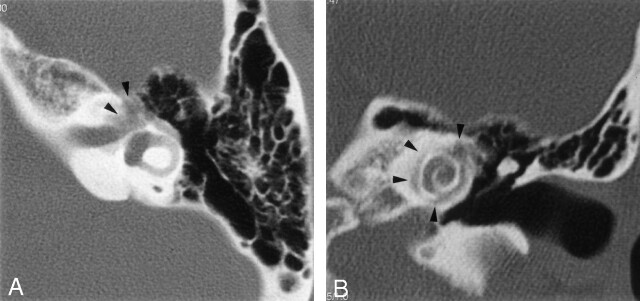
Fig 2.
Further axial (A) and direct coronal (B) high-resolution CT scans through the level of the labyrinthine segment of the facial nerve (axial) and the cochlea (coronal) obtained 2 years after the initial scans (1-mm section thickness; 512 × 512 matrix). The labyrinthine segment, the geniculate ganglion (arrowheads), and the proximal tympanic segment of the facial nerve canal are severely involved and have indistinct, irregular margins. Progression of demineralization is also demonstrated in pericochlear areas (arrowheads).
Pre- and postgadolinium thin-section axial and coronal T1-weighted and high-resolution three-dimensional T2-weighted fast spin-echo (3D-FSE) sequences were performed. T1-weighted MR imaging showed bilateral, symmetric, bandlike pericochlear hypointense lesions within the otic capsule. After intravenous contrast material administration, the lesions showed a homogeneous and symmetric contrast enhancement surrounding the turns of the cochlea. Further enhancement was also depicted in the fundus of the internal auditory canal bilaterally, along the labyrinthine and proximal tympanic segments of both facial nerves, and in the geniculate ganglion on the left side (Fig 3). Maximum intensity projections of the T2-weighted images showed bilateral irregularities of the T2 hyperintense margins of the labyrinthine structures and focal narrowing of the proximal basal cochlear turn. On the 3D-FSE image, the distal intrameatal segment of the facial nerve showed a normal diameter.
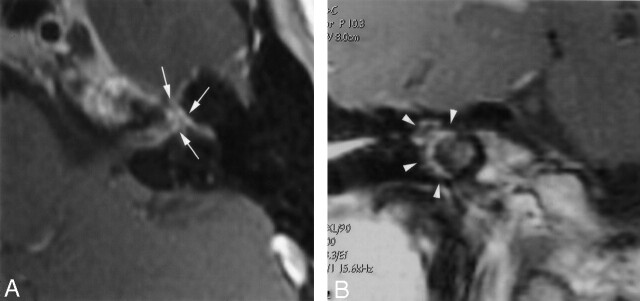
Fig 3.
Axial (A) and coronal (B) T1-weighted gadolinium-enhanced images (TR/TE/NEX, 500/20/3; section thickness, 3 mm) through the level of the distal internal auditory canal (axial) on the left, and the cochlea (coronal) on the right side. Enhancement is depicted in the fundus of the internal auditory canal, along the labyrinthine and proximal tympanic segments of the facial nerve, and in the geniculate ganglion (arrows). Further bandlike, pericochlear contrast enhancement is demonstrated, corresponding to the areas of CT hypoattenuation (arrowheads).
Discussion
OI is a heritable disorder of connective tissue with heterogeneous penetrance that, in addition to bone, may affect tendons, ligaments, fascia, skin, sclera, blood vessels, heart valves, and teeth. Depending on the four types of OI, mild to severe degrees of bone involvement occur (2). OI is histopathologically characterized by thickened and undermineralized bone. The pathologic changes in the temporal bone are qualitatively similar to those occurring in the peripheral skeleton (13). There is deficient bone, as indicated by the presence of numerous and large vascular spaces and lack of bone development causing brittle bony mastoid partitions (14).
In the current patient, postgadolinium T1-weighted MR imaging showed symmetrical, bandlike, homogeneously enhancing pericochlear areas, corresponding to the hypoattenuation detected with CT. This enhancement pattern could have been caused by pooling or leaking of contrast material into the proliferating areas of undermineralized bone or by the associated inflammation. Enhancement of the fundus of the internal auditory canal and of the labyrinthine segment of the facial nerve were additionally depicted on MR images. The pathologic enhancement along the facial nerve in the absence of a focal bulbous nerve swelling in the distal intrameatal segment, in conjunction with normal facial nerve functions, is difficult to explain. This enhancement possibly derives from the pathologic changes affecting the inner margins of the bony facial nerve canal as depicted on CT scans, rather than from an inflammatory edematous nerve thickening itself (15). The T2-weighted 3D-FSE sequence showed bilateral irregularities in the outline of the labyrinthine cavities and focal narrowing at the proximal basal turn of the cochlea. These signal intensity alterations could reflect spongiotic foci, which are known to affect all parts of the otic capsule, including the vestibule and the semicircular canals.
So far, no cure for OI has been found, and treatment options have been limited to symptomatic therapy, such as vitamin or hormonal supplementation, analgesics to alleviate chronic bone pain, or biphosphonate therapy to increase bone density and to reduce fracture rates. In dedicated cases, cochlear implantations have been shown to be successful, resulting in a significant increase in auditory abilities (16). Nevertheless, the unique anatomic aberrations in OI warrant special consideration before undertaking cochlear implantation. Preoperatively, these structural aberrations should be precisely depicted with CT and MR imaging. In particular, before placing the electrode array, the patency of the basal turn of the cochlea should be adequately assessed by using a high-resolution, 3D, T2-weighted sequence.
The differential diagnosis of bilateral otic capsule demineralization as demonstrated in this case of Van der Hoeve-de Kleyn syndrome is otosclerosis, Paget disease, otosyphilis, and Camurati-Engelmann disease.
OI and otosclerosis share many similar histologic and radiographic features, and their relationship has been therefore controversially regarded in the literature, although biochemical data demonstrated dissimilar protein and enzyme concentrations in these two entities (12). Histologic analysis showed that otosclerosis also can be distinguished morphologically, because OI involves all three layers of the otic capsule (ie, endosteum, endochondral layer, and periosteum), whereas otosclerosis is limited to the endochondral layer (12). At CT and MR imaging, the demineralization of the otic capsule in OI is remarkably similar to that occurring in otosclerosis. OI, however, is a generalized bone disorder, whereas otosclerosis is a localized disease of the petrous bone. Furthermore, the severity of the involvement of the bony labyrinth appears to be greater in OI than in otosclerosis (4, 6). The onset of hearing loss is earlier in OI than in otosclerosis, occurring most commonly during the 2nd and 3rd decades of life (4–6, 17). Patients with OI may have conductive, sensorineural, or mixed hearing loss. Conductive hearing loss may be the result of a fracture or localized dehiscence of the stapedial arch, distal atrophy of the long process of the incus, or fixation of the stapedial footplate (1). Sensorineural hearing loss is believed to result from microfractures, hemorrhage, and encroachment of reparative vascular and fibrous tissue in and around the cochlea. The higher incidence of high-frequency loss suggests that involvement of the basal turn of the cochlea occurs frequently in patients with OI (13). By contrast, pure sensorineural hearing loss rarely occurs in otosclerosis.
Paget disease, or osteitis deformans, is a generalized bone disorder primarily affecting the axial skeleton. Involvement of the petrous bone is commonly associated with changes in the skull (6, 18). CT scans show diffuse demineralization of the entire petrous bone in a characteristic washed-out appearance (6, 18). The involvement of the bony labyrinth in Paget disease is often asymmetric, in contrast to the involvement pattern of OI (12).
Otosyphilis, otherwise known as luetic involvement of the temporal bone, can manifest as labyrinthitis, gummatous lesion of the internal auditory canal, or inflammatory resorptive osteitis (19). It manifests with a moth-eaten permeative appearance and can cause secondary involvement of the membranous labyrinth in the late congenital, late latent, and tertiary stages of syphilis (12, 19). Otosyphilis may therefore simulate the demineralized appearance of OI and otosclerosis but is typically accompanied by systemic manifestation of syphilis. An additional key distinguishing feature of otosyphilis is the demineralization of the ossicles, which has never been reported in OI, otosclerosis, or Paget disease (20).
Camurati-Engelmann disease, also called progressive diaphyseal dysplasia, is an autosomal dominant disease with variable expression and penetrance, manifesting during childhood to early adulthood (21). In addition to the long bones, it may affect the skull and temporal bones leading to sensorineural, conductive or mixed hearing loss, facial palsy, and optic atrophy. CT commonly shows hypoattenuated areas around the cochlea and labyrinth and bone apposition in the oval and round window niches (21). It can be distinguished from OI by the specific roentgenographic findings of the long bones, which typically show a widening of the diaphysis (21).
Conclusion
The definite diagnosis of OI relies on the detection of mutations in specific genes. Despite several differential diagnoses, neuroradiologists should be aware of this entity when encountering bilateral areas of demineralization in the otic capsules of the temporal bones. It is an important differential consideration in a patient presenting with sensorineural hearing loss, who may be evaluated to rule out a mass in the cerebellopontine angle. Moreover, in previously undiagnosed patients with an only mild phenotype of OI presenting with hearing loss, CT, together with MR imaging, may be the clue that leads to a correct diagnosis. In dedicated cases, the precise knowledge about the disease in combination with accurate imaging can also assist the surgeon in the preoperative planning for cochlear implantation.
References
- 1.Nager GT. Osteogenesis imperfecta of the temporal bone and its relation to otosclerosis. Ann Otol Rhinol Laryngol 1988;97:585–593 [DOI] [PubMed] [Google Scholar]
- 2.Sillence DO, Senn A, Danks DM. Genetic heterogeneity in osteogenesis imperfecta. J Med Genet 1979;16:101–116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ablin DS. Osteogenesis imperfecta: a review. Can Assoc Radiol J 1998;49:110–123 [PubMed] [Google Scholar]
- 4.Ross UH, Laszig R, Bornemann H, Ulrich C. Osteogenesis imperfecta: clinical symptoms and update findings in computed tomography and tympano-cochlear scintigraphy. Acta Otolaryngol (Stockh) 1993;113:620–624 [DOI] [PubMed] [Google Scholar]
- 5.Van der Hoeve J, de Kleyn A. Blaue Scleren, Knochenbrüchigkeit und Schwerhörigkeit. Arch Ophthalmol 1918;95:81–93 [Google Scholar]
- 6.Tabor EK, Curtin HD, Hirsch BE, May M. Osteogenesis imperfecta tarda: appearance of the temporal bones at CT. Radiology 1990;175:181–183 [DOI] [PubMed] [Google Scholar]
- 7.Mafee MF, Valvassori GE, Deitch RL, et al. Use of CT in the evaluation of cochlear otosclerosis. Radiology 1985;156:703–708 [DOI] [PubMed] [Google Scholar]
- 8.Palacios E, Valvassori G. Osteogenesis imperfecta. Ear Nose Throat J 2000;79:232. [PubMed] [Google Scholar]
- 9.Swartz JD, Harnsberger HR. The Optic Capsule and Otodystrophies. In: Imaging of the Temporal Bone. 2nd ed. New York: Thieme;1992. :192–246
- 10.Czerny C, Temmel AF. Quiz case 7: osteogenesis imperfecta tarda with association of the inner ear also called Van Hoeve-Klein-syndrome. Eur J Radiol 1999;30:162–164 [DOI] [PubMed] [Google Scholar]
- 11.Ziyeh S, Berger R, Reisner K. MRI-visible pericochlear lesions in osteogenesis imperfecta type I. Eur Radiol 2000;10:1675–1677 [DOI] [PubMed] [Google Scholar]
- 12.Heimert TL, Lin DDM, Yousem DM. Case 48: osteogenesis imperfecta of the temporal bone. Radiology 2002;224:166–170 [DOI] [PubMed] [Google Scholar]
- 13.Shapiro JR, Pikus A, Weiss G, Rowe DW. Hearing and middle ear function in osteogenesis imperfecta: JAMA 1982;247:2120–2126 [PubMed] [Google Scholar]
- 14.Marion MS, Hinojosa R. Osteogenesis imperfecta. Am J Otolaryngol 1993;14:137–138 [DOI] [PubMed] [Google Scholar]
- 15.Sartoretti-Schefer S, Kollias S, Wichmann W, Valavanis A. T2-weighted three-dimensional fast spin-echo MR in inflammatory peripheral facial nerve palsy. AJNR Am J Neuroradiol 1998;19:491–495 [PMC free article] [PubMed] [Google Scholar]
- 16.Migirov L, Henkin Y, Hildesheimer M, Kronenberg J. Cochlear implantation in a child with osteogenesis imperfecta. Int J Pediatr Otorhinolaryngol 2003;67:677–680 [DOI] [PubMed] [Google Scholar]
- 17.Shea JJ, Postma DS. Findings and long-term surgical results in the hearing loss of osteogenesis imperfecta. Arch Otolaryngol 1982;108:467–470 [DOI] [PubMed] [Google Scholar]
- 18.d’Archambeau O, Parizel PM, Koekelkoren E, et al. CT diagnosis and differential diagnosis of otodystrophic lesions of the temporal bone. Eur J Radiol 1990;11:22–30 [DOI] [PubMed] [Google Scholar]
- 19.Fayad JN, Linthicum FH Jr. Temporal bone histopathology case of the month: otosyphilis. Am J Otol 1999;20:259–260 [PubMed] [Google Scholar]
- 20.Sonne JE, Zeifer B, Linstrom C. Manifestations of otosyphilis as visualized with computed tomography. Otol Neurotol 2002;23:806–807 [DOI] [PubMed] [Google Scholar]
- 21.Huygen PLM, Cremers CWRJ, Verhagen WIM, Joosten FBM. Camurati-Engelmann disease presenting as “juvenile otosclerosis.” Int J Pediatr Otorhinolaryngol 1996;37:129–141 [DOI] [PubMed] [Google Scholar]