Abstract
Background and aim of the work:
Every year around 275 thousand people in Europe and 420 thousand in the United States are affected by sudden cardiac arrest. Early electrical defibrillation before the arrival of emergency services can improve survival. Training the population to use the AED is essential. The training method currently in use is the BLSD course, which limits training to a population cohort and may not be enough to meet the requirements of the proposed Law no. 1839/2019. This study aims to verify the effectiveness of an online course that illustrates the practical use of the AED to a population of laypeople.
Methods:
An observational study was conducted to compare a lay population undergoing the view of a video spot and a cohort of people who had participated in BLSD Category A courses. The performances of the two groups were measured immediately after the course and 6 months later.
Results:
Overall, the video lesson reported positive results. Six months later the skills were partially retained. The cohort that followed the video lesson showed significant deterioration in the ability to correctly position the pads and in safety.
Conclusions:
Although improved through significant reinforcements, the video spot represents a valid alternative training method for spreading defibrillation with public access and could facilitate the culture of defibrillation as required by the new Italian law proposal. (www.actabiomedica.it)
Keywords: Out-of-hospital cardiac arrest, public access defibrillation (PAD), automated external defibrillator (AED), defibrillation, first responders, lay public, training, outcomes related, safety
Background
An estimated 17.9 million people died from cardiovascular diseases in 2016, representing 31% of all global deaths. Of these deaths, 85% are due to heart attack and stroke (WHO, 2020) (1). In the same year, in Italy were recorded 221,914 deaths (ISTAT, 2019) (2).
Sudden cardiac arrest affects about 420 thousand people in the United States and 275 thousand in Europe annually (3).
Gräsner et al. (4) calculated in Europe an incidence rate of 84 cardiac arrests per 100 thousand inhabitants. Analyzing the primary heart rhythms, a quarter of the victims have initial ventricular fibrillation, which tends to evolve into asystole before extra-hospital rescuers arrive. This because rescue time after 5 - 8 minutes from the event makes the heart rhythm no longer shockable. (5). The presence of an automatic external defibrillator (AED) at the time of collapse could improve the prognosis by restoring a cardiac rhythm compatible with an effective circulation up to 76% of subjects affected by ventricular fibrillation (6).
Recent studies have shown that the use of the AED by unqualified people or with minimal training is safe and effective. Therefore, if a spectator can use an automatic defibrillator, this practice is recommended (7, 8).
In the last ten years, there has been an explosion of defibrillation programs in places with public access (PAD), in fact, even in Italy, the legislator, with its decree, established by law the presence of the AED in places with large numbers of visitors (9).
Yet despite the literature, the recommendations, the regulations, and the increase in the number of AEDs in public places, the portion of patients in cardiac arrest defibrillated before the rescue vehicle arrives, remains significantly low (10). Brooks et al. (11) and Smith et al. (12) have shown that in front of a collapsed person who is not responding, only 1.7-2.1% of viewers look for and use an AED before the ambulance arrives.
Since 2001, in Italy, a precise law grants the use of the semi-automatic defibrillator by non-healthcare personnel with specific training in cardio-pulmonary resuscitation activities (13). This rule does not seem to facilitate the use of the AED, as in the countries where the law allows all citizens to use the AED, their use is about 15-20% higher (8).
However, the Italian law, having requested the presence of the defibrillator in sports centers, highlighted an important first result. In 2015, were 123 the arrests reported in sports facilities with a return to spontaneous circulation for 62% of the victims after using the AED. This shows that the norm works, even if the device used only by specially trained people is not enough to reduce incidence in the general population (14). For this reason, we have made efforts to identify potential obstacles related to the use of AEDs by the lay public. The nature of obstacles turned out to be multifactorial and, among the causes, there is certainly the legal liability (4-38%); other relevant obstacles are the lack of knowledge about how the device works, not feeling comfortable in using it and the fear of causing harm to the victim (12).
A public access defibrillation program (PAD) (15) to be successful requires three requisites: firstly, there must be enough devices in the community; secondly, their position must be known or easily identifiable in an emergency, thirdly the public must have sufficient knowledge and confidence to use them. All these requirements must be met for a bystander to provide effective defibrillation. However, generally, national systems have so far focused on the first of these requirements, therefore greater use of public AEDs will not be achieved until the population has acquired greater knowledge and confidence with them (11).
The current classroom teaching methods, to acquire enough knowledge and confidence for the use of the AED, cannot be easily disclosed to the whole community and can present significant logistical, temporal and financial barriers, especially when it is necessary to form large groups. To cope with these difficulties, the scientific community has proposed alternative training methods for non-experts. Although not yet validated, these new methods present good results in their support (16). Remarkably, the testing of structured courses through video lessons and the use of the web has proven effective even in the physical absence of the instructor (17, 20). Recent studies conducted on school-aged students between 14 and 19 years old have shown a good efficacy of video-based training. This type of population seems to be particularly receptive to training in use the AED through this teaching method (21).
In Italy, a bill proposed at the end of July 2019 called “Progetto Life” provides that it is allowed to be able to use an AED even without specific training.. However, rescuers must follow the instructions given by the 112 emergency center health professionals. (22).
Aim
Assess of level of the learning in the use of the AED, through the viewing of a video spot and the subsequent practice on a static simulator
Research questions
1. In remote training courses, does the lesson through video spots compared to traditional BLSD courses provide the necessary skills for using the defibrillator?
2. Which skills, acquired through the video lesson and the BLSD courses, remain in the learner after months from the end of the training?
Materials and Methods
Study design and participants
Prospective and retrospective observational studies were conducted in 2019. The research involved the 1st year students of the Degree Course in Nursing at the University of Bologna and a cohort of operators from some metalworking companies in northern Italy. Our convenience sample of 91 lay people, 44 students, and 47 workers never held CPR courses or early defibrillation courses and had no clinical subject knowledge. We divided the sample into two groups according to the training method. The students attended the video lesson, while the workers were trained with the BLSD course certified IRC ©.
The video spot production was carried out by medical instructors and nurses experienced in cardiopulmonary resuscitation and with IRC certification. The video creation took inspiration from three videos found on the web: “How to Use a Defibrillator (AED) - First Aid Training” by St John Ambulance, “Emergency CPR / AED Emergency Response Update” and “HeartStart Field Defibrillator (AED) Video of training “by Philips.
1ª Phase of the study
The prospective study took place in this phase. The students were divided into groups with an instructor and learner ratio of approximately 1: 6. The learners were shown twice, 5 minutes apart, the video in which the use of the AED was explained in 4 minutes. The video instructions included six essential steps: 1. the 112/118 call; 2. switching on the AED; 3. how to uncover the victim’s chest; 4. the positioning of the defibrillator pads; 5. how to comply with the rules for using the AED safely; 6. the delivery of the shock if indicated.
After watching the videos, the students were asked to immediately perform the procedure on the manikin under the supervision of the instructors, who immediately proceeded to evaluate the performance through a specific form that summarized the video steps. As regards the retrospective survey, 47 workers were randomized through the database of BLSD courses carried out in metalworking companies in a province of northern Italy and their performances were obtained from the forms. The BLSD courses had been held a few months earlier by the same instructors enrolled for the prospective study with the video lesson (Figure 1).
Figure 1.

Phase 1 of the study
2ª Phase of the study
After 6 months, 1st year nursing students were recalled. Of these, 34 responded to the invitation, 10 fewer than in the first phase. Without viewing any video or repeating the instructors’ instructions, they were asked to repeat the procedure for using the AED on the manikin.
After 6 months, the 47 randomized workers were also asked to use the AED on a manikin without any revision of the IRC © procedures.
The performance of the two groups was assessed by the same instructors, with the same tool used in the first phase.
Ethical considerations
All the sample involved in the study gave their written consent after learning the purpose and method of conducting the research. The anonymity and confidentiality of the participants were guaranteed. The research was authorized by the Bioethics Committee of Bologna University and by the Coordinator of the Degree Course in Nursing in Faenza, Italy.
Statistical analyses
The data were collected through Office Excel; the statistical analysis was conducted with SPSS software, version 26. Descriptive statistics calculations (mean, standard deviation, frequency, percentages) were performed. Significances were analyzed through Pearson’s Chi-square.
Results
Nursing students evaluated immediately after the video lesson are 90.9% (n = 40) females, with an average age of 21.32 ± 5.59 and all with a high school diploma without further degrees.
The workers who achieved the BLSD certificate are 95.7% (n = 45) male, with an average age of 38.51 ± 11.69 and all with a high school diploma. Overall, the results of the video lesson are positive. Compared to the performances provided by the BLSD course, which provides for the knowledge of all the passages (100%), the video lesson achieved an average performance percentage of 89.77% ± 15.75. As regards the 6 single performances provided by the video: 79.5% call 112 or 118, 95.5% correctly turn on the AED, 97.7% correctly discover the patient’s chest, 81.8% attacks the plates in the correct position, 88.8% follow the safety instructions and 95.5% deliver the shock if required (Graphic 1).
Graphic 1.

Distribution of students performance in the first phase
After six months, the average percentage of performance retention is significant for both training modalities (p = < .0001). The BLSD course sustains a performance of 81.21 ± 15.39, with an average difference of 18.79 respect to the certification phase. The video lesson maintains a 63.73 ± 15.05 losing a 26.04. However, both students and workers have maintained positive performances in skills 1, 2 and 3 with a range that varies from 64.7 to 94.1%. Skill 4 suffered a worsening for both groups with an average percentage value of 48.1%, while for performances 5 and 6 there were significant differences. Workers trained with the BLSD responded positively to the “follow instructions safely” ability for 63.8% (n = 30) of the sample, against 2.9% (N = 1) of the student group. In skill 6, although recording a significant difference between the video lesson and the BLSD, the performances remain above 88% (Table 1).
Table 1.
Performance evaluation after 6 months. Comparison between the two cohorts.
| BLSD Course | Video lesson | Total | ||||
| n = 47 | n = 34 | N = 81 | ||||
| Performance | n | % | n | % | N (%) | p |
| 1. Call 118 or 112 | 35 | 74.5 | 22 | 64.7 | 57 (70.4) | .342 |
| 2. Use the AED and turn it on | 47 | 100 | 32 | 94.1 | 79 (97.5) | .092 |
| 3. Uncover the victim’s chest | 46 | 97.9 | 30 | 88.2 | 76 (93.8) | .075 |
| 4. Attach the pads in the correct position | 24 | 51.1 | 15 | 44.1 | 39 (48.1) | .537 |
| 5. Follow the safety instructions | 30 | 63.8 | 1 | 2.9 | 31 (38.3) | .000** |
| 6. Dispense shock if required | 47 | 100 | 30 | 88.2 | 77 (95.1) | .016* |
* p = < .05; ** p = < .01
The difference in performance between the video lesson and the BLSD is also highlighted by a significant loss in the performance of the video lesson (activities 4 and 5) in the period immediately after viewing the videos (T0) and its subsequent verification after 6 months (T1) (Table 2).
Table 2.
Evaluation of students’ performance after 6 months from the administration of the video lesson.
| T0 | T1 | |||||
| n = 44 | n = 34 | |||||
| Performance | n | % | n | % | Δ | p |
| n. 1 | 35 | 79.5 | 22 | 64.7 | -14.8 | .143 |
| n. 2 | 42 | 95.5 | 32 | 94.1 | -1.4 | .791 |
| n. 3 | 43 | 97.7 | 30 | 88.2 | -9.5 | .090 |
| n. 4 | 36 | 81.8 | 15 | 44.1 | -37.7 | .001** |
| n. 5 | 39 | 88.6 | 1 | 2.9 | -85.7 | .000** |
| n. 6 | 42 | 95.5 | 30 | 88.2 | -7.3 | .235 |
* p = < .05; ** p = < .01
In graphic 2, after 6 months, there is a good holding of the skills acquired in the video lesson, the curve becomes significantly negative in skills 4 and 5 with a loss of 28.9% in the first and 85.7 in the second.
Graphic 2.
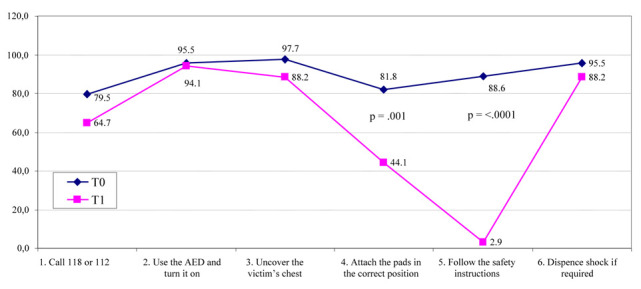
Retention of skills with the video lesson at T0 and T1.
Discussion
The study, by what has been highlighted in the literature (17-20), shows that a short video lasting some minutes, which illustrates simply the fundamental steps of the use of a semiautomatic defibrillator and which uses an easy to understand language, can be a valid training method for a “non-professional” public of health (layman).
The video allows the desired message to reach many people, especially as regards the youth population (21).
The use of the AED requires specific training and simulation is a tool highly appreciated by learners (23-25), but it is also the method that allows you to prevent accidents and promote safety (26). Simulate the use of the AED through a video lesson could be a valid strategy considering a possible future application of the legislative proposal no. 1839 (2019) (22); distance learning could guarantee the minimum skills needed to effectively use the AED (7, 8). The study, however, noted a certain difficulty for the students in maintaining their performances. After 6 months, statistically significant differences were pointed out, especially as regards the safety of the scene, significantly less guaranteed by the students compared to the BLSD sample.
However, even the workers trained through the BLSD course have shown a decrease in performance in the application of adhesive pads on the chest and in the safe execution of the procedure. The skills gaps months after defibrillation courses are confirmed in the literature. Educational reinforcements following certification are recommended to maintain the standards acquired during training (27, 28).
Conclusions
Unlike the BLSD courses that require the physical presence of the students and a certain economic and organizational commitment both in the certification courses and in the retraining, the video lesson can be carried out remotely, at low prices, easily accessible to a large population. A video spot of this kind, related to the law currently under approval, could empower the population. The statements of the video should be passionate and highly engaging on the emotional side, so the main concepts could thus be better retained in the population that receives them (29).
As exemplified by this study, videos need training reinforcement; a simple solution could be to administer them as spots of the Ministry of Health, using both traditional and social information channels; so they could represent a valid tool to spread the culture of defibrillation and encourage citizens to use it effectively, as required by the new Italian law proposal and literature.
The main limitations of the study are the size and characteristics of the sampling. The research takes into consideration a limited sample relating to two cohorts that are not entirely equivalent by age, gender and professionalism: the average age of 20 years, female prevalence, university students for video lessons; an age < 40 years, male prevalence, workers for BLSD courses. To confirm our results further studies with a larger sampling are needed, including subjects randomly assigned to cohorts with comparable age, professionalism and personal characteristics.
Acknowledgments
We would like to thank Domenico Motola, Coordinator of the Degree Course in Nursing at the UNIBO Campus in Ravenna, for having authorized the study within the course and the group of instructors at the IRC centre AUSL Romagna - Forlì.
Conflict of interest:
Each author declares that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangement etc.) that might pose a conflict of interest in connection with the submitted article
References
- 1.World Health Organization. Cardiovascular Diseases. 2020 Available from: https://www.who.int/health-topics/cardiovascular-diseases/#tab=tab_1 . (Accessed 18 April 2020) [Google Scholar]
- 2.Istat. Indagine su decessi e cause di morte. 2019 Available from: https://www.istat.it/it/archivio/4216 . (Accessed 18 April 2020) [Google Scholar]
- 3.Moya-Mitjans À, Lidón RM. Automatic External Defibrillator in Sudden Out-of-hospital Cardiac Arrest: In Search of Effective Treatment. Rev Esp Cardiol (Engl Ed) 2018;71:64–6. doi: 10.1016/j.rec.2017.09.001. [DOI] [PubMed] [Google Scholar]
- 4.Gräsner JT, Lefering R, Koster RW, et al. EuReCa ONE-27 Nations, ONE Europe. ONE Registry: A prospective one-month analysis of out-of-hospital cardiac arrest outcomes in 27 countries in Europe. Resuscitation. 2016;105:188–95. doi: 10.1016/j.resuscitation.2016.06.004. [DOI] [PubMed] [Google Scholar]
- 5.Lapucci G, Bondi B, Rubbi I, et al. A randomized comparison trial of two and four-step approaches to teaching Cardio-Pulmonary Reanimation. Acta Biomed. 2018;89(4-S):37–44. doi: 10.23750/abm.v89i4-S.7129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Perkins GD, Handley AJ, Koster RW, et al. European Resuscitation Council Guidelines for Resuscitation 2015: Section 2. Adult basic life support and automated external defibrillation. Resuscitation. 2015;95:81–99. doi: 10.1016/j.resuscitation.2015.07.015. [DOI] [PubMed] [Google Scholar]
- 7.Holmberg MJ, Vognsen M, Andersen MS, Donnino MW, Andersen LW. Bystander automated external defibrillator use and clinical outcomes after out-of-hospital cardiac arrest: A systematic review and meta-analysis. Resuscitation. 2017;120:77–87. doi: 10.1016/j.resuscitation.2017.09.003. [DOI] [PubMed] [Google Scholar]
- 8.Baldi E, Savastano S. AED use before EMS arrival: When survival becomes a matter of law and system in Italy, which can be improved. Eur Heart J. 2018;39:1664. doi: 10.1093/eurheartj/ehy196. [DOI] [PubMed] [Google Scholar]
- 9.Decreto Interministeriale 18 marzo 2011. Determinazione dei criteri e delle modalità di diffusione dei defibrillatori semiautomatici esterni di cui all’art. 2 co. 46 della legge n. 191/2009. Available from: http://www.trovanorme.salute.gov.it/norme/dettaglioAtto?id=38392 . (Accessed 18 April 2020) [Google Scholar]
- 10.Fredman D, Haas J, Ban Y, et al. Use of a geographic information system to identify differences in automated external defibrillator installation in urban areas with similar incidence of public out-of-hospital cardiac arrest: a retrospective registry-based study. BMJ Open. 2017;7:e014801. doi: 10.1136/bmjopen-2016-014801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brooks B, Chan S, Lander P, Adamson R, Hodgetts GA, Deakin CD. Public knowledge and confidence in the use of public access defibrillation. Heart. 2015;101:967–71. doi: 10.1136/heartjnl-2015-307624. [DOI] [PubMed] [Google Scholar]
- 12.Smith CM, Lim Choi Keung SN, Khan MO, et al. Barriers and facilitators to public access defibrillation in out-of-hospital cardiac arrest: a systematic review. Eur Heart J Qual Care Clin Outcomes. 2017;3:264–73. doi: 10.1093/ehjqcco/qcx023. [DOI] [PubMed] [Google Scholar]
- 13.Legge 3 aprile 2001, n. 120. Utilizzo dei defibrillatori semiautomatici in ambiente extraospedaliero. Available from: https://www.gazzettaufficiale.it/atto/serie_generale/caricaDettaglioAtto/originario?atto.dataPubblicazioneGazzetta=2001-04-14&atto.codiceRedazionale=001G0173&elenco30giorni=false . (Accessed 18 April 2020) [Google Scholar]
- 14.Zorzi A, Susana A, Spadotto V, Cacciavillani L, Corrado D. Sudden cardiac arrest in Italian sports facilities in 2015: epidemiological implications of the so-called “Balduzzi decree”. G Ital di Cardiol. 2016;17:903–907. doi: 10.1714/2498.26192. [DOI] [PubMed] [Google Scholar]
- 15.Sondergaard KB, Hansen SM, Pallisgaard JL, et al. Out-of-hospital cardiac arrest: Probability of bystander defibrillation relative to distance to nearest automated external defibrillator. Resuscitation. 2018;124:138–44. doi: 10.1016/j.resuscitation.2017.11.067. [DOI] [PubMed] [Google Scholar]
- 16.Yeung J, Okamoto D, Soar J, Perkins GD. AED training and its impact on skill acquisition, retention and performance - a systematic review of alternative training methods. Resuscitation. 2011;82:657–64. doi: 10.1016/j.resuscitation.2011.02.035. [DOI] [PubMed] [Google Scholar]
- 17.Isbye DL, Rasmussen LS, Lippert FK, Rudolph SF, Ringsted CV. Laypersons may learn basic life support in 24 min using a personal resuscitation manikin. Resuscitation. 2006;69:435–42. doi: 10.1016/j.resuscitation.2005.10.027. [DOI] [PubMed] [Google Scholar]
- 18.Lynch B, Einspruch EL, Nichol G, Becker LB, Aufderheide TP, Idris A. Effectiveness of a 30-min CPR self-instruction program for lay responders: a controlled randomized study. Resuscitation. 2005;67:31–43. doi: 10.1016/j.resuscitation.2005.04.017. [DOI] [PubMed] [Google Scholar]
- 19.Roppolo LP, Pepe PE, Campbell L, et al. Prospective, randomized trial of the effectiveness and retention of 30-min layperson training for cardiopulmonary resuscitation and automated external defibrillators: The American Airlines Study. Resuscitation. 2007;74:276–85. doi: 10.1016/j.resuscitation.2006.12.017. [DOI] [PubMed] [Google Scholar]
- 20.De Vries W, Handley AJ. A web-based micro-simulation program for self-learning BLS skills and the use of an AED. Can laypeople train themselves without a manikin? Resuscitation. 2007;75:491–98. doi: 10.1016/j.resuscitation.2007.05.014. [DOI] [PubMed] [Google Scholar]
- 21.Paglino M, Contri E, Baggiani M, et al. A video-based training to effectively teach CPR with long-term retention: the ScuolaSalvaVita.it (“SchoolSavesLives.it”) project. Intern Emerg Med. 2019;14:275–79. doi: 10.1007/s11739-018-1946-3. [DOI] [PubMed] [Google Scholar]
- 22.Proposta di legge 08 maggio 2019, n. 1836, Modifiche alla tabella A allegata al decreto del Presidente della Repubblica 26 ottobre 1972, n. 633, e alla legge 3 aprile 2001, n. 120, per la promozione della diffusione e dell’impiego dei defibrillatori semiautomatici e automatici. Available from: https://www.camera.it/leg18/126?leg=18&idDocumento=1836 . (Accessed 18 April 2020) [Google Scholar]
- 23.Cremonini V, Ferri P, Artioli G, Sarli L, Piccioni E, Rubbi I. Nursing students’ experiences of and satisfaction with the clinical learning environment: the role of educational models in the simulation laboratory and in clinical practice. Acta Biomed. 2015;86 Suppl 3:194–204. [PubMed] [Google Scholar]
- 24.Rubbi I, Ferri P, Andreina G, Cremonini V. Learning in clinical simulation: observational study on satisfaction perceived by students of nursing. Prof Inferm. 2016;69:84–94. doi: 10.7429/pi.2016.692084. [DOI] [PubMed] [Google Scholar]
- 25.Ferri P, Rovesti S, Magnani D, et al. The efficacy of interprofessional simulation in improving collaborative attitude between nursing students and residents in medicine. A study protocol for a randomised controlled trial. Acta Biomed. 2018;89(7-S):32–40. doi: 10.23750/abm.v89i7-S.7875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rubbi I, Cremonini V, Butuc A, et al. Incidence and type of health care associated injuries among nursing students: an experience in northern Italy. Acta Biomed. 2018;89(7-S):41–9. doi: 10.23750/abm.v89i7-S.7812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gonzi G, Sestigiani F, D’errico A, et al. Correlation between quality of cardiopulmonary resuscitation and self-efficacy measured during in-hospital cardiac arrest simulation; preliminary results. Acta Biomed. 2015;86 Suppl 1:40–5. [PubMed] [Google Scholar]
- 28.Jeffers J, Eppich W, Trainor J, Mobley B, Adler M. Development and Evaluation of a Learning Intervention Targeting First-Year Resident Defibrillation Skills. Pediatr Emerg Care. 2016;32:210–6. doi: 10.1097/PEC.0000000000000765. [DOI] [PubMed] [Google Scholar]
- 29.Rollero C. L’oggettivazione attraverso gli spot pubblicitari: l’influenza dei media su umore e autostima. Psicologia di comunità. 2013;2:65–72. [Google Scholar]


