Abstract
Background:
The Surprise Question (“Would I be surprised if this patient were to die within the next 12 months?”) is widely used to identify palliative patients, though with low predictive value. To improve timely identification of palliative care needs, we propose an additional Surprise Question (“Would I be surprised if this patient is still alive after 12 months?”) if the original Surprise Question is answered with “no.” The combination of the two questions is called the Double Surprise Question.
Aim:
To examine the prognostic accuracy of the Double Surprise Question in outpatients with cancer.
Design:
A prospective study.
Participants:
Twelve medical oncologists completed the Double Surprise Question for 379 patients.
Results:
In group 1 (original Surprise Question “yes”: surprised if dead) 92.1% (176/191) of the patients were still alive after 1 year, in group 2a (original and additional Surprise Question “no”: not surprised if dead and not surprised if alive) 60.0% (63/105), and in group 2b (original Surprise Question “no,” additional Surprise Question “yes”: surprised if alive) 26.5% (22/83) (p < 0.0001). The positive predictive value increased by using the Double Surprise Question; 74% (61/83) vs 55% (103/188). Anticipatory palliative care provision and Advance Care Planning items were most often documented in group 2b.
Conclusions:
The Double Surprise Question is a promising tool to more accurately identify outpatients with cancer at risk of dying within 1 year, and therefore, those in need of palliative care. Studies should reveal whether the implementation of the Double Surprise Question leads to more timely palliative care.
Keywords: Palliative care, advance care planning, medical oncology, surprise question, timely identification, predictive value
What is already known about the topic?
The original Surprise Question (“Would I be surprised if this patient were to die within the next 12 months?”) is widely used to identify palliative patients, however, it also identifies a substantial number of patients who are not necessarily in the last year of their lives, which may have resource implications.
To improve the predictive value of the original Surprise Question an additional Surprise Question (“Would I be surprised if this patient is still alive after 12 months?”) has been added to the original Surprise Question in cases where the original Surprise Question is answered with “no” (the Double Surprise Question).
The Double Surprise Question appeared promising in elderly patients (⩾75 years) listed in general practice, but its prognostic accuracy for (out)patients with cancer is unknown.
What this paper adds?
The Double Surprise Question is a promising tool to more accurately identify outpatients with cancer at risk of dying within 1 year, and therefore, those in need of palliative care.
Using the Double Surprise Question instead of the original Surprise Question alone prevents the identification of a substantial number of patients who are not in the last year of their lives.
Implications for practice, theory, or policy
The Double Surprise Question seems promising in assisting professionals to identify patients with cancer who have unmet palliative care needs more accurately.
Implementation studies should reveal whether the Double Surprise Question can contribute to more timely palliative care.
Background
Timely palliative care has shown beneficial effects; it improves quality of life1–3 and patient autonomy,4 it decreases futile interventions,5,6 and it lowers costs.7 Despite these beneficial effects, palliative care is often still restricted to terminal care in patients with advanced cancer.3,8,9 One of the main reasons for this is the challenge of timely identifying palliative care needs in patients with cancer.10
Several tools have been developed to timely identify patients’ palliative care needs.11,12 Nonetheless, these tools seem to be little suited for daily practice, as they consist of many items and applying them is time-consuming. An easy and practical tool is the original Surprise Question.13 Professional caregivers asks themselves: “Would I be surprised if this patient were to die within the next 12 months?” to determine whether “the person is in a fragile enough condition that relatively minor worsening or intercurrent illnesses could spell the end of life.”13 However, the original Surprise Question performs poorly to modestly as a predictive tool for death within 6–18 months.14,15 Consequently, the use of the original Surprise Question alone may lead to identifying a substantial number of patients who may not necessarily be in the last year of their lives, and this may have resource implications.15 Therefore, there is an urgent need to further develop accurate and practical screening tools to identify patients with palliative care needs.14,15 For that reason, an additional Surprise Question was introduced: “Would I be surprised if this patient is still alive after 12 months?”. The additional Surprise Question is only asked in cases where the original Surprise Question is answered with “no.” The combination of these two questions is called “the Double Surprise Question.” The Double Surprise Question may be valuable as an easy identification method to identify patients who need palliative care, as these needs are usually most prominent in their last year of life.16 To date, the Double Surprise Question has been studied in primary care and has shown promising results. Case vignette studies showed that general practitioners are willing to use the Double Surprise Question.17,18 In an explorative study, the prognostic accuracy of the Double Surprise Question for patients aged ⩾75 years in general practice was examined. It was shown that the Double Surprise Question is able to discriminate between patients with different life expectancies and palliative care needs.19 However, the prognostic accuracy of the Double Surprise Question is unknown for patients with cancer.
The aim of this study was to examine the prognostic accuracy of the Double Surprise Question in outpatients with cancer. We hypothesized that the Double Surprise Question more accurately identifies palliative care needs than the original Surprise Question, by stratifying patients in three risk groups with different survival rates.
Methods
Study design and setting
We performed a prospective study at the Medical Oncology Outpatient clinic of the Radboud university medical center (Radboudumc), Nijmegen, The Netherlands.
Participants and recruitment
In 2017, medical oncologists completed the Double Surprise Question for their patients, so the patients were not directly involved in this study. We retrieved data from patient records; no further consent was needed in addition to the standard opt-out procedure in the Radboudumc (see section “Ethical considerations”). Medical oncologists gave verbal consent when the researcher (DE) asked them if they were willing to answer the Double Surprise Question for those patients consulting them. Patients were eligible when aged ⩾18 years. There were no exclusion criteria. Due to the novelty of the Double Surprise Question in outpatients with cancer, we decided not to perform a power calculation.
Study procedure and data collection
We asked all medical oncologists who completed consultations at the outpatient clinic to answer the Double Surprise Question individually for every patient who had been scheduled that day. Consequently, we did not make a preselection of patients for whom the surprise questions were answered. Answers were not documented in the medical records but stored separately. One year later, the hospital patients’ medical records were reviewed retrospectively. We collected (demographic) patient characteristics, death within 1 year, documentation of palliative care provision (as described by the WHO20), Advance Care Planning (based on to the definition defined by Rietjens et al.21), and healthcare use during the year following Double Surprise Question completion. We used those secondary outcomes as a proxy for palliative care needs. Table 1 and Supplemental Appendix Table A1 give a complete overview of all outcome measures and their operationalization.
Table 1.
Outcome measurements and descriptions used for the case report form.
| Double Surprise Question outcome | Answers on the original Surprise Question (yes/no). If “no,” answers on the additional Surprise Question (yes/no). |
| Medical oncologists’ characteristics | Age, gender, years of experience. |
| Data regarding death*a | Date, place (home/hospital/hospice/nursing home/other/unknown) and cause of death (cancer/respiratory/cardiovascular/other cause/unknown). |
| (Demographic) patient characteristics | Age, gender, living situation (at home with partner/at home alone/living in house of family member/residential home/other/unknown), care provider (partner/child/other family member/friend/neighbor/unknown relationship/other/unknown, none) and home care (yes/no/unknown) provided during study period. Type of cancer*b (blood/bone marrow and lymph nodes/bone and soft tissue/breast/central nervous system/endocrine glands/head and neck/skin/male genital organs/lower respiratory system/urinary tract/digestive organs/female genital organs/unknown primary site/more than one type of cancer). Performance status*c: Eastern Cooperative Oncology Group score (0–5) ± 7 days at date the Double Surprise Question was answered. |
| Palliative care20 and Advance Care Planning21 | Advance Care Planning directives (yes/no): cardiopulmonary resuscitation and intensive care policy, and other limitations regarding treatment, and hospital admission policy. Advance Care Planning aspects (yes/no): preference place of treatment or death, whether prognosis/disease or dying scenarios, euthanasia, palliative sedation was discussed, or whether there was an advance directive (e.g. representative and euthanasia directive). Dimensions of palliative care*d (yes/no): Somatic: symptoms, complaints, general health. Non-somatic (psychological, social or spiritual): fear, depressed mood, emotions, anger, denial, anxiety, worries, social contacts, holidays, tension between patient and loved ones or care providers, financial worries, leaving loved ones when dying, saying goodbyes, things that occupy someone, balance of life, questions regarding life and death, preparing for dying, a wish to die, feeling powerless or dependent, hope, faith. Anticipation regarding the somatic and non-somatic dimension of palliative care: whether there was anticipated on the dimensions of palliative care, for example when a patient wanted to attend a wedding the therapy was paused, or prophylactic antibiotics were prescribed. Others (yes/no): personal aspect regarding quality of life and personal goals, for example attending a wedding. |
| Healthcare use | Involvement of (yes/no): palliative care team, pain team, psychologist, and chaplain. Number of consultations with: medical oncologist, other specialists, oncology nurses (including clinical nurse specialists and case managers at the medical oncology department), other nurses, palliative care team, pain team, psychologists, chaplains and other paramedical caregivers. Treatment during the follow up period, the first 3 months and last 3 months of life*e (yes/no): antibiotics, infusion therapy (hydration fluids or transfusion), surgery, artificial feeding, chemo-, radio-, immuno-, targeted and hormone-therapy and other treatment. Hospitalizations: number and duration (in days) of hospitalizations during the study period. Emergency department visits: number of visits during the study period. |
A patient was considered death when: (1) death was stated in the electronic medical record; (2) when the patient could be found at www.Mensenlinq.nl (a website for death registration in The Netherlands); (3) the general practitioner, contacted by EK (part of the treatment team), confirmed the patient’s death (when 1 and 2 did not provide information on death).
Based on the tumor classification of the Dutch quality institute for oncological and palliative research and practice.22
For the patients’ performance status, we used the Eastern Cooperative Oncology Group score.23 In case the Karnofsky Performance Status24 was reported, we transcribed this into an Eastern Cooperative Oncology Group score according to the transcription table.23
Initially, we reviewed whether the medical records contained information on each of the four different domains of palliative care. However, it appeared that a proper distinction between the domains could not be made. Therefore, the somatic domain was called “somatic” and the psychological, social and existential domain where combined and together called “non-somatic.”
Treatment during the last 3 months was reviewed only when a patient had died during the study period.
One researcher (DE) reviewed the medical records and extracted the data. A second researcher (GvdL) independently reviewed 20 selected medical records that contained most Advance Care Planning items to warrant inter-observer reliability of the extracted data. To check intra-observer reliability, 20 medical records were reviewed twice (by DE); the first 10, and 10 which contained most Advance Care Planning documentation. In case of doubt, issues were discussed with YE and EK. Supplemental Appendix Table A1 shows Cohen’s kappa for inter-observer and intra-observer reliability.
To effectively blind the researcher for the Double Surprise Question outcomes, the extracted data and Double Surprise Question results were not electronically merged until all medical records had been reviewed. Data were stored in Castor (a validated database that meets the Good Clinical Practice criteria), and the database was locked after extraction of all data.
Test methods
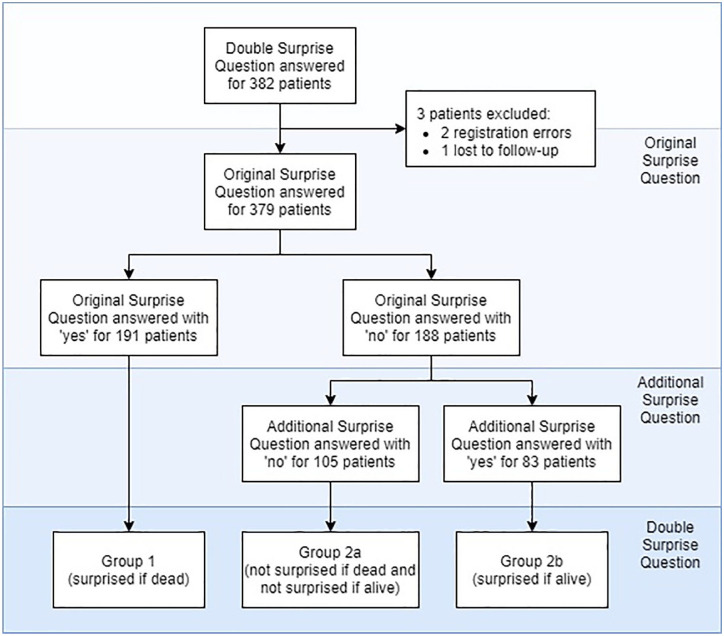
The study population was divided into three groups following the answers to the Double Surprise Question (Figure 1): group 1 the medical oncologist stated that he/she would be surprised if the patient were to die in the next 12 months (surprised if dead); group 2a the medical oncologist stated that he/she would not be surprised if the patient were to die in the next 12 months, and would not be surprised if the patient would still be alive after 12 months (not surprised if dead and not if alive); and group 2b the medical oncologist stated that he/she would not be surprised if the patient were to die in the next 12 months and would be surprised if the patient would still be alive after 12 months (surprised if alive).
Figure 1.
Outpatients with cancer for whom the Double Surprise Question was answered by medical oncologists; the Double Surprise Question divided the study population into three groups.
Using the original Surprise Question, the study population was divided into two groups: group 1 corresponding with group 1 of the Double Surprise Question (surprised if dead), and group 2 corresponding with group 2a and 2b of the Double Surprise Question combined (not surprised if dead).
Data analyses
To determine the prognostic accuracy of the Double Surprise Question we evaluated its ability to accurately predict death. We plotted Kaplan-Meier estimates stratified by the original Surprise Question and Double Surprise Question groups, and analyzed the differences using the log-rank test. We determined 1-year survival probabilities per group.
We then compared the prognostic accuracy of the original Surprise Question (two groups) with the Double Surprise Question (three groups). To account for the difference in the number of groups, we combined group 2a (not surprised if dead and not if alive) and group 1 (surprised if dead) of the Double Surprise Question. This group then consisted of patients who were not and those who were less expected to die within 1 year. We compared this dichotomous version of the Double Surprise Question to the original Surprise Question; we compared sensitivity, specificity, positive and negative predictive value for the Double Surprise Question to the original Surprise Question.
Moreover, we used descriptive statistics for all secondary outcomes. To describe differences between the Double Surprise Question and the original Surprise Question, we compared group 1 (surprised if dead) with group 2 (not surprised if dead), and group 2a (not surprised if dead and not if alive) with group 2b (surprised if alive). For dichotomous outcomes, logistic regression models were used, and we only analyzed those variables with more than 10 observations in both the groups with a positive and a negative outcome. A generalized estimating equation was applied to allow for data clustering within medical oncologists. For counts data, we applied a negative binomial regression analysis with bootstrapping. In both cases, 95% confidence intervals for Odds Ratios and Incidence Rate Ratios were calculated.
Statistical analyses were performed with IBM SPSS software version 25 and R version 3.6.1.
Ethical considerations
The research ethics committee of Radboudumc approved this study, case number 2017-3403. All Radboudumc patients are informed that anonymized route registration data can be used for scientific research and are given the possibility to opt-out. Therefore, according to Dutch law (Medical Treatment Contracts Act25 and Medical Research Involving Human Subjects Act10), written informed consent for reviewing medical records was not required.
Results
Participants
Twelve oncologists answered the Double Surprise Question for a total of 382 patients, with a variation between 5 and 85 patients per medical oncologist. Of the medical oncologists, 75% (9/12) was female, with a mean age of 46 years (range 32-64), and the median years of expertise was 9 (mean 12, range 1-27).
Three patients were removed from analysis; two of them due to registration errors, and one was lost to follow-up. Subsequently, data used to study the Double Surprise Question were based on 379 patients (Figure 1). Group 1, group 2a, and group 2b consisted of 191, 105, and 83 patients respectively.
The mean age of patients was 59.4 years (Table 2); 44.3% were female. Patients had different types of cancer, of which skin, digestive organs, breast, and urinary tract cancer were most frequent. Supplemental Appendix Table A2 provides a complete overview of all demographic patient characteristics and their health status.
Table 2.
Demographic, functional and social patient characteristics obtained from the medical records.
| Group 1 (surprised if dead), n = 191 | Group 2a (not surprised if dead and not if alive), n = 105 | Group 2b (surprised if alive), n = 83 | All patients, n = 379 | |
|---|---|---|---|---|
| Age; mean (SD) | 56 (15) | 65 (13) | 61 (13) | 59 (15) |
| Gender | ||||
| Female; N (%) | 81 (42.4) | 46 (43.8) | 41 (49.4) | 168 (44.3) |
| Type of cancer; N (%) | ||||
| Skin | 37 (19.4) | 23 (21.9) | 16 (19.3) | 76 (20.1) |
| Digestive organs | 18 (9.4) | 18 (17.1) | 22 (26.5) | 58 (15.3) |
| Breast | 29 (15.2) | 10 (9.5) | 11 (13.3) | 50 (13.2) |
| Urinary tract | 18 (9.4) | 22 (21.0) | 10 (12.0) | 50 (13.2) |
| Male genital organs | 36 (18.8) | 6 (5.7) | 3 (3.6) | 45 (11.9) |
| Bone and soft tissue | 13 (6.8) | 2 (1.9) | 9 (10.8) | 24 (6.3) |
| Female genital organs | 9 (4.7) | 5 (4.8) | 5 (6.0) | 19 (5.0) |
| Central nervous system | 6 (3.1) | 8 (7.6) | 4 (4.8) | 18 (4.7) |
| More than one cancer | 10 (5.2) | 8 (7.6) | 0 (0.0) | 18 (4.7) |
| Head and neck | 11 (5.8) | 2 (1.9) | 3 (3.6) | 16 (4.2) |
| Endocrine glands | 3 (1.6) | 0 (0.0) | 0 (0.0) | 3 (0.8) |
| Blood, bone marrow and lymph nodes | 1 (0.5) | 0 (0.0) | 0 (0.0) | 1 (0.3) |
| Unknown primary site | 0 (0.0) | 1 (1.0) | 0 (0.0) | 1 (0.3) |
| Lower respiratory system | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
SD: standard deviation; N: number.
Prognostic accuracy
After 1 year, in group 1 (surprised if dead), 92.1% (176/191) of the patients were still alive; in group 2 (not surprised if dead) this was 45.2% (85/188); in group 2a (not surprised if dead and not if alive) this was 60.0% (63/105); and in group 2b (surprised if alive) 26.5% (22/83) (Figure 2). One-year survival probabilities differed significantly between groups stratified by the original Surprise Question and by the Double Surprise Question; both for group 1 vs group 2 and for group 1 vs group 2a vs group 2b: p < 0.0001.
Figure 2.
Kaplan-Meier curve with 95% CI (in colour) of the different groups divided by the original Surprise Question (group 1 [surprised if dead] and group 2 [not surprised if dead]) and the Double Surprise Question (group 1 [surprised if dead], group 2a [not surprised if dead and not if alive], and group 2b [surprised if alive]).
For 188 patients, the medical oncologist would not be surprised if the patient were to die within 1 year (original Surprise Question “no”). After 1 year, 103 patients of them had died (PPV: 54.8%). From the remaining 191 patients of whom the medical oncologist would be surprised if the patient would die within 1 year (original Surprise Question “yes”), 176 patients were still alive after 1 year (NPV:92.1%). For the 188 patients identified by the original Surprise Question, an additional surprise Question was asked. The medical oncologist would be surprised if the patient would be still alive after 1 year (additional Surprise Question “yes”) for 83 of the 188 patients. After 1 year, 61 of them had died (PPV: 73.5%). For 105 patients the medical oncologist would not be surprised if the patient would be still alive after 1 year (additional Surprise Question “no”) of whom 63 were still alive after 1 year (NPV: 60%).
In comparison with the original Surprise Question, the specificity and positive predictive value (PPV) of the Double Surprise Question was better (67.7% [95% CI 61.6%-73.3%] to 91.6% [87.5%-94.6%], and 54.8% [47.4%-62.0%] to 73.5% [62.7%-82.6%], respectively), see Table 3. The sensitivity and negative predictive value (NPV) decreased significantly (87.3% [79.9%-92.7%] to 51.7% [42.3%-61.0%] and 92.1% [87.4%-95.5%] to 80.7% [75.8%-85.1%], respectively).
Table 3.
The accuracy of the Surprise Question and the additional Surprise Question, and a comparison between them.
| Deceased N | Alive N | Total N | Sensitivity,a % (95% CI) | Specificity,b % (95% CI) | PPV,c % (95% CI) | NPV,d % (95% CI) | ||
|---|---|---|---|---|---|---|---|---|
| SQ1 | No | 103 | 85 | 188 | 87.3 (79.9–92.7) | 67.7 (61.6–73.3) | 54.8 (47.4–62.0) | 92.1 (87.4–95.5) |
| Yes | 15 | 176 | 191 | |||||
| Total | 118 | 261 | 379 | |||||
| SQ2e | Yes | 61 | 22 | 83 | 59.2 (49.1–68.8) | 74.1 (63.5–83.0) | 73.5 (62.7–82.6) | 60.0 (50.0–69.4) |
| No | 42 | 63 | 105 | |||||
| Total | 103 | 85 | 188 | |||||
| DSQ | Predicted death | 61 | 22 | 83 | 51.7 (42.3–61.0) | 91.6 (87.5–94.6) | 73.5 (62.7–82.6) | 80.7 (75.8–85.1) |
| Predicted alive | 57 | 239 | 296 | |||||
| Total | 118 | 261 | 379 |
N: number; CI: confidence interval; PPV: positive predictive value; NPV: negative predictive value.
Sensitivity: ability to correctly identify patients who will die.
Specificity: ability to correctly identify patients who will not die.
PPV: ability to predict death.
NPV: ability to predict survival.
The additional Surprise Question was only asked when the original Surprise Question was answered with “no,” therefore the N does not equal the entire study population.
Secondary outcomes
Palliative care provision and Advance Care Planning
Aspects of the somatic and non-somatic (psychological, social or spiritual) dimensions of palliative care were documented in 99.5% and 81.5% of medical records respectively (Table 4). Documentation of neither the somatic nor the non-somatic dimensions of palliative care differed between groups (Supplemental Appendix Table A3). In group 2b (surprised if alive), anticipation regarding the somatic and non-somatic dimensions of palliative care was more often documented than in group 2a (not surprised if dead and not if alive) (21.7% vs 8.6%). In 36.1% of the medical records of group 1 patients (surprised if dead), at least one Advance Care Planning aspect or directives was documented; these figures were 55.2% for group 2a, and 75.9% for group 2b. In 13.1% of the medical records of group 1 patients, three or more Advance Care Planning aspects or directives were documented; these figures were 26.7% for group 2a, and 37.3% for group 2b (Table 4 and Supplemental Appendix Table A3).
Table 4.
Palliative care provision, advance care planning and healthcare use during the year following Double Surprise Question completion.
| Group 1 (surprised if dead), N = 191 | Group 2a (not surprised if dead and not if alive), N = 105 | Group 2b (surprised if alive), N = 83 | All patients, N = 379 | ||
|---|---|---|---|---|---|
| Palliative care provision | |||||
| Dimensions of palliative care; N (%) | |||||
| Somatic | 190 (99.5) | 104 (99) | 83 (100) | 377 (99.5) | |
| Non-somatic*a | 156 (81.7) | 87 (82.9) | 66 (79.5) | 309 (81.5) | |
| Anticipation | 19 (9.9) | 9 (8.6) | 18 (21.7) | 46 (12.1) | |
| Other palliative care aspects; N (%) | |||||
| Personal aspects regarding quality of life | 14 (7.3) | 27 (25.7) | 23 (27.7) | 64 (16.9) | |
| Personal goals | 2 (1.0) | 8 (7.6) | 7 (8.4) | 17 (4.5) | |
| Other preferences for treatment | 16 (8.4) | 24 (22.9) | 30 (36.1) | 70 (18.5) | |
| Advance care planning aspect(s) or directive(s) | |||||
| At least one | 69 (36.1) | 58 (55.2) | 63 (75.9) | 190 (50.1) | |
| At least three | 25 (13.1) | 28 (26.7) | 31 (37.3) | 84 (22.2) | |
| Healthcare use | |||||
| Number of consultations with; median [IQR] | |||||
| Medical oncologists | 9 [11] | 12 [11] | 5 [12] | 9 [12] | |
| Other specialists | 4 [9] | 6 [9] | 2 [9] | 4 [9] | |
| Oncology nurses | 5 [15] | 7 [14] | 3 [10] | 5 [14] | |
| Involvement of; N (%) | |||||
| Palliative care team | 14 (7.3) | 19 (18.1) | 17 (20.5) | 50 (13.2) | |
| Pain team | 19 (9.9) | 12 (11.4) | 13 (15.7) | 44 (11.6) | |
| Psychologist | 8 (4.2) | 1 (1.0) | 2 (2.4) | 11 (2.9) | |
| Chaplain | 5 (2.6) | 4 (3.8) | 7 (8.4) | 16 (4.2) | |
| Number emergency department visits; N (%) | |||||
| 0 | 142 (74.3) | 60 (57.1) | 49 (59.0) | 251 (66.2) | |
| 1 | 29 (15.2) | 24 (22.9) | 17 (20.5) | 70 (18.5) | |
| 2 | 14 (7.3) | 9 (8.6) | 10 (12.0) | 33 (8.7) | |
| ⩾3 | 6 (3.1) | 12 (11.4) | 7 (8.4) | 25 (6.6) | |
| Number of hospitalizations; N (%) | |||||
| 0 | 118 (61.8) | 59 (56.2) | 45 (54.2) | 222 (58.6) | |
| 1 | 32 (16.8) | 25 (23.8) | 21 (25.3) | 78 (20.6) | |
| 2 | 18 (9.4) | 12 (11.4) | 11 (13.3) | 41 (10.8) | |
| ⩾3 | 23 (12.0) | 9 (8.6) | 6 (7.2) | 38 (10.0) | |
N: number; IQR: inter quartile range.
Initially, we reviewed whether the medical records contained information on each of the four different domains of palliative care. However, it appeared that a proper distinction between the domains could not be made. Therefore, the somatic domain was called “somatic” and the psychological, social and existential domain where combined and together called “non-somatic.”
Healthcare use
The median number of consultations with medical oncologists, other specialists, and oncological nurses was lowest in group 2b (Table 4). The palliative care team, the pain team, psychologist, and chaplain were most frequently involved in patients in group 2b but did not differ significantly (Supplemental Appendix Table A4). Patients in group 1 more frequently visited the emergency department than patients in group 2 (Table 4). For this outcome, no differences were found between groups 2a and 2b. No differences between the number of hospitalizations were found between the groups. During follow-up, patients in group 2b received tumor targeted therapy (e.g., radio, immune, and hormone therapy) less frequently, Supplemental Appendix Table A4.
Discussion
Main findings
The Double Surprise Question appeared a promising tool to more accurately identify patients with cancer at the Medical Oncology Outpatient clinic who are at risk of dying, and therefore, in need of palliative care. The Double Surprise Question correctly identified 74% of the patients to be in their last year of life, while this figure was 55% for the original Surprise Question; the positive predictive value of the Double Surprise Question performed better than the original Surprise Question alone (74% [95% CI 63%-83%] vs. 55% [47%-62%]). Using the Double Surprise Question prevents the identification of a substantial number of patients who are not in the last year of their lives, and may avoid unnecessarily burdening palliative care resources. This result can easily be explained as the dichotomous Double Surprise Question by definition is more conservative in estimating which patients are more at risk of dying within 1 year. To account for the difference in the number of groups distinguished by the original Surprise Question (two groups) and the Double Surprise Question (three groups) we combined group 2a (not surprised if dead and not if alive) and group 1 (surprised if dead) of the Double Surprise Question. As a result, a substantial number of patients identified by the original Surprise Question (group 2: not surprised if dead) is combined with group 1 (surprised if dead). Consequently, the specificity/positive predictive value increases and the sensitivity/negative predictive value decreases.
However, using the dichotomous version of the Double Surprise Question has implications; 48.3% (57/118) of the patients that died within the next 12 months had not been identified as such. Therefore, we recommend not to use the dichotomous version of the Double Surprise Question; the strength of the Double Surprise Question is its ability to distinguish three groups of patients with an increasing risk of dying within 1 year, and therefore, with increasing palliative care needs.
Proactive care provision and Advance Care Planning documented in hospital patients’ medical records significantly differed between the groups with the lowest life expectancy. In group 2b anticipation regarding the somatic and non-somatic dimensions of palliative care and ⩾1 Advance Care Planning aspects or directives were documented more often than in group 2a. However, documentation of three or more Advance Care Planning aspects or directives appeared to be limited (13.1% of the medical records). No differences were found for the documentation of the somatic and non-somatic dimensions of palliative care, the involvement of the palliative care team, the pain team, psychologist, and chaplain, and the number of emergency department visits and hospitalizations.
Strengths and limitations of the study
This is the first study to examine the prognostic accuracy of the Double Surprise Question at a medical oncology outpatient clinic in secondary care. In our study, we asked medical oncologists to answer the Double Surprise Question for every patient who had had a consultation at the outpatient clinic that day without making a preselection, opposed to many other studies.15 Moreover, some concerns have been expressed regarding the use of the original Surprise Question in extensive identification tools for palliative needs and in palliative care guidelines.26–28 Concerns involve the moderate predictive values for death and the lack of evidence that a negative answer to the original Surprise Question correlates with palliative care needs. Therefore, we did not focus on death alone. We also provided information about documentation on palliative care provision as proxy of palliative care needs, for which the original Surprise Question was initially intended.13 Our results showed that the three groups of the Double Surprise Question correlated with increasing palliative care provision and Advance Care Planning.
Our study has some limitations. First, there is a lack of evidence that palliative care provision correlates with palliative care needs. Second, not all types of cancer were presented in this study, as some patients with certain types of cancer are treated at other departments than the medical oncology department. In the Netherlands, for example, patients with lung cancer are treated at the department of Pulmonology. Consequently, we are cautious to generalize our results to all outpatients with cancer. Third, we only retrieved data from the hospital medical records and not from primary care medical records, and it is known that general practitioners play a key role in providing end-of-life care. This may have led to an underestimation of our secondary outcomes. Moreover, we did not correct healthcare use for the length of follow-up, which may also have led to an underestimation; in groups 2a and 2b more patients died during the year, consequently they had a shorter length of follow-up which may have led to an underestimation of the quantity and quality of care. Finally, medical oncologists may have been affected by the Double Surprise Question answers while planning and providing care, as the use of the Double Surprise Question may have raised awareness with regard to the palliative care needs of their patients. However, the answers on the Double Surprise Question were not documented in the medical record. Additionally, even in the group with the lowest life-expectancy, we still found limited palliative care provision.
What this study adds
Comparison with existing literature
We showed that the Double Surprise Question is able to classify (out)patients with cancer into three groups with different life expectancies and palliative care needs. Veldhoven et al.19 found similar results in elderly patients (⩾75 years) listed in general practices in the Netherlands. Our results regarding the accuracy of the original Surprise Questions matches those from a systematic review performed by White et al.15 showing that the original Surprise Question detects at least as many false positives as true positives. However, the accuracy of the original Surprise Question in our study is higher than in the systematic review performed by Downar et al.14 A possible explanation is that the number of patients with cancer differs between the studies (43% vs. 58% respectively), and patients with cancer are known to have relatively predictable disease trajectories.10
Implications for research and practice
The Double Surprise Question performs better than the original Surprise Question alone when identifying patients with cancer at risk of dying during the next year. Adding the second Surprise Question makes it possible to divide the patients for whom the original Surprise Question is answered with “no” into two groups: a small group to focus proactive palliative care on, and a larger group to monitor less intensively. Thus, the Double Surprise Question can help professionals to carefully balance between the timely identification of more patients with cancer who have unmet palliative care needs, without over-burdening limited professional resources. However, more scientific evidence is needed to support this hypothesis. Further research should examine whether the application of the Double Surprise Question contributes to more timely palliative care. Additionally, future studies should validate the Double Surprise Question in different settings and different patient groups. Moreover, to minimize the risk of missing patients in need of palliative care, studies need to reveal how often the Double Surprise Question should be used as an identification tool. Finally, we recommend studying whether the Double Surprise Question is a cost-effective way to identify patients in need of palliative care.
Conclusion
In daily practice, it is not feasible to provide proactive palliative care to all patients identified with the original Surprise Question due to time constraints. Therefore, we recommend starting palliative care for patients classified in group 2b when identified by the Double Surprise Question in an oncological hospital setting, as more than 50% will pass away within 6 months. Although 26.5% of the patients in this group are not actually in their last year of life, it is unlikely that a palliative care approach would adversely affect their care; it may even result in better provision of holistic care.15 For patients classified in group 2a (not surprised if dead and not surprised if alive), we recommend to actively monitor these patient to minimize the risk of missing patients in need of palliative care.
Supplemental Material
Supplemental material, sj-pdf-1-docx-10.1177_0269216320986720 for Timely identification of patients in need of palliative care using the Double Surprise Question: A prospective study on outpatients with cancer by Daisy JM Ermers, Evelien JM Kuip, CMM Veldhoven, Henk J Schers, Marieke Perry, Ewald M Bronkhorst, Kris CP Vissers and Yvonne Engels in Palliative Medicine
Acknowledgments
We are grateful to the medical oncologists who answered the Double Surprise Question for the patients included in our study. We would also like to thank Dr. Stans Verhagen who had an essential role in the design of our study. Many thanks as well to Guus van der Linden for acting as a second reviewer to guarantee inter-observer reliability.
Footnotes
Author contributions: Conception and design: DE, YE, SV. Provision of study materials or patients: DE. Collecting and assembly of data: DE. Data analysis and interpretation, manuscript writing, final approval of manuscript, and accountable for all aspects of the work: all authors.
Data management and sharing: Data are available upon reasonable request via the corresponding author.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval and informed consent: This study was approved by the research ethics committee of the Radboudumc, case number 2017-3043. All patients are informed that data from their medical record may be used for research and are given the possibility to opt-out. Therefore, according to Dutch law (Medical Treatment Contracts Act and Medical Research Involving Human Subjects Act), written informed consent for reviewing medical records was not required.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Daisy JM Ermers  https://orcid.org/0000-0003-1985-2839
https://orcid.org/0000-0003-1985-2839
Yvonne Engels  https://orcid.org/0000-0002-7669-1018
https://orcid.org/0000-0002-7669-1018
Supplemental material: Supplemental material for this article is available online.
References
- 1. Bakitas M, Lyons KD, Hegel MT, et al. Effects of a palliative care intervention on clinical outcomes in patients with advanced cancer: the Project ENABLE II randomized controlled trial. JAMA 2009; 302(7): 741–749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Temel JS, Greer JA, Muzikansky A, et al. Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med 2010; 363(8): 733–742. [DOI] [PubMed] [Google Scholar]
- 3. Zimmermann C, Swami N, Krzyzanowska M, et al. Early palliative care for patients with advanced cancer: a cluster-randomised controlled trial. Lancet 2014; 383(9930): 1721–1730. [DOI] [PubMed] [Google Scholar]
- 4. Weathers E, O’Caoimh R, Cornally N, et al. Advance care planning: a systematic review of randomised controlled trials conducted with older adults. Maturitas 2016; 91: 101–109. [DOI] [PubMed] [Google Scholar]
- 5. Mack JW, Cronin A, Keating NL, et al. Associations between end-of-life discussion characteristics and care received near death: a prospective cohort study. J Clin Oncol 2012; 30(35): 4387–4395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wright AA, Zhang B, Ray A, et al. Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. JAMA 2008; 300(14): 1665–1673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Molloy DW, Guyatt GH, Russo R, et al. Systematic implementation of an advance directive program in nursing homes: a randomized controlled trial. JAMA 2000; 283(11): 1437–1444. [DOI] [PubMed] [Google Scholar]
- 8. Hackett J, Bekker H, Bennett MI, et al. Developing a complex intervention to support timely engagement with palliative care for patients with advanced cancer in primary and secondary care in the UK: a study protocol. BMJ Open 2018; 8(5): e022835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Abarshi EA, Echteld MA, Van den Block L, et al. Recognising patients who will die in the near future: a nationwide study via the Dutch Sentinel Network of GPs. Br J Gen Pract 2011; 61(587): e371–e378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Murray SA, Kendall M, Boyd K, et al. Illness trajectories and palliative care. BMJ 2005; 330(7498): 1007–1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Maas EA, Murray SA, Engels Y, et al. What tools are available to identify patients with palliative care needs in primary care: a systematic literature review and survey of European practice. BMJ Support Palliat Care 2013; 3(4): 444–451. [DOI] [PubMed] [Google Scholar]
- 12. Walsh RI, Mitchell G, Francis L, et al. What diagnostic tools exist for the early identification of palliative care patients in general practice? A systematic review. J Palliat Care 2015; 31(2): 118–123. [DOI] [PubMed] [Google Scholar]
- 13. Lynn J. Living long in fragile health: the new demographics shape end of life care. Hastings Cent Rep 2005; 34: 14–18. [DOI] [PubMed] [Google Scholar]
- 14. Downar J, Goldman R, Pinto R, et al. The ‘surprise question’ for predicting death in seriously ill patients: a systematic review and meta-analysis. CMAJ 2017; 189(13): E484–E493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. White N, Kupeli N, Vickerstaff V, et al. How accurate is the ‘Surprise Question’ at identifying patients at the end of life? A systematic review and meta-analysis. BMC Med 2017; 15(1): 139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Teunissen SC, Wesker W, Kruitwagen C, et al. Symptom prevalence in patients with incurable cancer: a systematic review. J Pain Symptom Manage 2007; 34(1): 94–104. [DOI] [PubMed] [Google Scholar]
- 17. Klok L, Engels Y, Veldhoven C, et al. Early identification of patients in need of palliative care in Slovenian general practice. Zdr Varst 2018; 57(2): 55–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Weijers F, Veldhoven C, Verhagen C, et al. Adding a second surprise question triggers general practitioners to increase the thoroughness of palliative care planning: results of a pilot RCT with cage vignettes. BMC Palliat Care 2018; 17(1): 64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Veldhoven CMM, Nutma N, De Graaf W, et al. Screening with the double surprise question to predict deterioration and death: an explorative study. BMC Palliat Care 2019; 18(1): 118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Stewart S, McMurray JJ. Palliative care for heart failure. BMJ 2002; 325(7370): 915–916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Rietjens JAC, Sudore RL, Connolly M, et al. Definition and recommendations for advance care planning: an international consensus supported by the European Association for Palliative Care. Lancet Oncol 2017; 18(9): e543–e551. [DOI] [PubMed] [Google Scholar]
- 22. Tumorindeling, https://www.cijfersoverkanker.nl/tumorindeling-34.html (2019, accessed 31 July 2019).
- 23. Oken MM, Creech RH, Tormey DC, et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol 1982; 5(6): 649–655. [PubMed] [Google Scholar]
- 24. Mor V, Laliberte L, Morris JN, et al. The Karnofsky Performance Status Scale. An examination of its reliability and validity in a research setting. Cancer 1984; 53(9): 2002–2007. [DOI] [PubMed] [Google Scholar]
- 25. Elliott M, Nicholson C. A qualitative study exploring use of the surprise question in the care of older people: perceptions of general practitioners and challenges for practice. BMJ Support Palliat Care 2017; 7(1): 32–38. [DOI] [PubMed] [Google Scholar]
- 26. Bodkin H. ‘Surprise question’ sees thousands wrongly told they will die under faulty NHS system. The Telegraph, 2 August 2017. [Google Scholar]
- 27. Janssen DJA, Beuken-van Everdingen vd MHJ, Schols JMGA. Verrast door de ‘surprise question’. Ned Tijdschr Geneeskd 2015; 159: A8427. [Google Scholar]
- 28. Small N, Gardiner C, Barnes S, et al. Using a prediction of death in the next 12 months as a prompt for referral to palliative care acts to the detriment of patients with heart failure and chronic obstructive pulmonary disease. Palliat Med 2010; 24(7): 740–741. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-docx-10.1177_0269216320986720 for Timely identification of patients in need of palliative care using the Double Surprise Question: A prospective study on outpatients with cancer by Daisy JM Ermers, Evelien JM Kuip, CMM Veldhoven, Henk J Schers, Marieke Perry, Ewald M Bronkhorst, Kris CP Vissers and Yvonne Engels in Palliative Medicine