Abstract
Background and aim of the work:
Even though vaccination is easy to access in Europe, it has been facing several outbreaks caused by vaccine preventable diseases. Trying to balance the right to health of the community with individual self-determination, in Italy was mandate vaccination for ten vaccine preventable diseases in 2017. The project “Sportello Vaccinale” provided a counseling service to parents in kindergarten of Palermo. The main objective of the study was to investigate knowledge and compliance on vaccination by children’s parents after the implementation of mandatory vaccination.
Methods:
A cross sectional study was conducted among parents accessing to the “Sportello Vaccinale” using a questionnaire. The questionnaire consisted of 34 items divided into three sections: socio-demographic data; knowledge and attitude on mandatory vaccination using Health Belief Model (HBM); Health Literacy (HL) level.
Results:
A total of 95 questionnaires were garnered in the kindergartens from respondents with a mean age of 36 (±SD=6) years. The respondents who delayed hexavalent or Measles, Mumps, Rubella and Varicella (MMRV) vaccinations were 8 (8%) and the more frequent cause was fear of adverse reaction (87%). The sample had more often high level of health literacy (37%), and 55% had higher HBM score. The factor significantly associated with higher HBM score was the age of respondents (OR= 1.14, p=0.006) after controlling for other variables.
Conclusions:
Consent to vaccination practice was widely represented, but the results of the study highlighted the need for parents to have more information and more time devoted to the practice of vaccination counseling. Implementing counseling activities at school or at the vaccination service, could support an aware decision process of the parents on vaccination topic.
Keywords: mandatory vaccination, vaccine adherence, parent age, MMRV vaccine, hexavalent vaccine, Health Belief Model, Health Literacy, Safety, Accessibility, Sicily
Background
The Strategic Advisory Group of Experts on Immunization (SAGE) of the World Health Organization (WHO) defined with the term “vaccine hesitancy” the delay in the acceptance or the refusal of the vaccine despite the availability of vaccination services (1). Vaccine hesitancy represents a complex topic, context-specific and very variable depending on the country, the age of the subject and the type of vaccine. It is influenced by factors such as information on vaccine-preventable diseases, efficacy and safety (1). Indeed, the lack of right information on the risk of contracting the disease, the mistaken belief that vaccines are unsafe or the lack of confidence in the efficacy of the vaccine can be obstacles to vaccination adherence (2).
Even though vaccination is easy to access in more developed countries, Europe has been facing several outbreaks caused by vaccine preventable diseases such as measles (3). This can be due by different measles vaccination coverage rates observed in countries, ranging from 85% in Italy to 99% in Luxembourg, with an average coverage for the EU of 93.6% in 2016 for the first dose (4).
Nowadays, the Italian vaccination schedule offer, as reported in the National Vaccine Immunization Plan (PNPV) 2017-2019, provides universal mass vaccination for 18 vaccine preventable diseases (5).
Notwithstanding, in Italy, 4,991 measles cases were reported in 2017 (including over 300 healthcare workers), with 4 deaths and 95% of the cases that were unvaccinated or vaccinated with a single dose (6). Other 2,526 cases of measles were reported in 2018. During this period, the highest incidence was recorded in children under one year of age. Furthermore, 47% of cases reported at least one complication and 8 deaths occurred (7). In Sicily, one of the four most populous Italian administrative region, before 2017 was showed vaccination coverage rates against measles far below 95%, the minimum level reccomended to eliminate virus circulation (8).
Trying to balance the right to health of the community with individual self-determination, the Italian Ministry of Health has decided to mandate vaccination for ten vaccine preventable diseases, adopting the law 119/2017 (9). Furthermore, the Italian government considered essential to focus on a better communication strategy aimed at the active and informed participation of the citizen in the public health program (9).
The new Italian mandatory law has showed an increase of vaccination coverage for the hexavalent and Measles, Mumps and Rubella (MMR) vaccines, but also for those vaccines which has been only recommended, such as the anti-pneumococcal and the antimeningococcal C vaccine (10). Although other factors on this phenomeon cannot be quantified and remain undefined, they may have a role as: the better information of healthcare workers, the judgment announcement of lack of causation between vaccination and suspected adverse reactions and the increase of web scientific information and social media debate by vaccinology experts (11).
A project called “Sportello Vaccinale” was conducted from March to April 2018 in 19 kindergarten of Palermo. The main aim of the project consisting in providing a counseling service to parents, giving information about vaccines of the Sicilian Immunization Schedule and the new regulations on vaccination in Italy after the introduction of the law 119/2017.
The main objective of the study was to investigate knowledge and compliance on vaccination by children’s parents attending kindergarten in Palermo after the implementation of mandatory vaccination.
Materials and methods
A cross sectional study was conducted among parents accessing to the “Sportello Vaccinale” using a questionnaire. It was filled in after collecting the written consent form by the children’s parents. The anonymity of the questionnaire was guaranteed by assigning an alphanumeric code, and after filling in the questionnaire an individual counselling with a Public Health physisician was held, to clarify any doubt and give information on mandatory vaccination law and Regional Vaccination schedule.
The questionnaire consisted of 34 items divided into three sections: socio-demographic data; knowledge and attitude on mandatory vaccination using Health Belief Model (HBM); Health Literacy (HL) level.
The second section of the questionnaire used one of the most validated and widely implemented model to explain vaccination adherence, the HBM. HBM was developed in the 1950s to explain and predict behavior in a population that adhere to preventive practices (12). It is structured in 4 main domains: susceptibility and perceived seriousness of disease, perceived advantages of preventive strategy and barriers to reach preventive services (12). The questionnaire contained 21 questions using a five points Likert scale (1 = not at all, 2 = little, 3 = enough, 4 = very and 5 = very much), that investigated the following items: perceived advantages on vaccinations; perceived advantages on hexavalent and Measles, Mump, Rubella and Varicella (MMRV) vaccinations; perceived barriers on vaccinations; perceived obstacles on hexavalent and MMRV vaccinations; perceived susceptibility to diseases prevented by vaccines; perceived severity of vaccine preventable disease.
A score was assigned to each answer, assigning 0 to the replies considered negative and 1 to the positive ones. High scores reflect a greater awareness of vaccination issue, its importance and the need to carry out available vaccinations. On the other hand, the lower scores were indicators of a lower awareness of vaccination and adherence to the vaccination programs.
HL allows to assess the ability to obtain, understand and manage health information and make appropriate health decisions using the offered services (13). For the evaluation of the HL, an examination based on the Medical Term Recognition Test (METER), adapted to the Italian language, was used (14) (15). The proposed test provides a list of 70 terms, 40 of medical use and 30 non-words or words not referable to medical use, requiring to mark only the words recognized as medical terms. The score is established by calculating the number of correctly recognized words and the results are then classified according to the scale: 0-20 = low level, 21-34 = medium level, 35-40 = high level.
Finally, to assess the reasons that led the parents to delay or refuse mandatory vaccinations, an open-ended questions was included “What was main reason of vaccine delay?”. The ethical committee Palermo 1 approved the study during the session 06/2017.
Statistic analysis
The normality of the distribution of quantitative variables was assessed with the Skewness and Kurtosis test. The quantitative variables distributed normally have been summarized as mean (standard deviation) and those distributed not normally as median (interquartile range). For the qualitative variables the absolute and relative frequencies have been calculated. Subsequently the whole population was divided in higher and lower HBM level according to median HBM score. The association of the quantitative variables normally and not normally distributed with higher scores achieved at the HBM was evaluated with the student’s T and with the Wilcoxon and Mann Withney test respectively; while for the qualitative variables the Chi2 test was used. All the variables associated with a p-value<0.5 with higher HBM scores were included in a multivariate logistic analysis model to analyze their effect. All the data collected were analyzed using the Stata MP 14.2 statistical software. For all analyses, a P-value of 0.05 was assumed to indicate significance (two-tailed).
Results
A total of 95 questionnaires were garnered in the kindergartens. Table 1 shows characteristics of interviewed parents, univariate and multivariate analysis. The questionnaire was filled in more frequently by mothers (89%), followed by fathers (7%), and by both parents (3%). The respondents had a mean age of 36 (±SD=6) years, their families were composed by 4 (±SD=1) members and they were more frequently Italian (93%). The most frequent civil status was married (81%) followed by cohabiting parents (14%) and the most prevalent education level was middle school (49%), followed by high school (35%) and university (11%). Only 5% of the sample worked in the health sector (social health assistant, pharmaceutical salesman and nurse). The main source of information regarding vaccinations was more frequently pediatrician (94%) followed by Local Health Unit vaccinating physician and book/newspaper (2% each). The sample had more often high level of health literacy (37%), followed by low (35%) and medium level (28%). The median score for HBM answer was 16 and according to this cut-off 52 (55%) respondents had higher and 43 (45%) lower HBM score. The respondents who delayed hexavalent or MMRV vaccination were 8 (8%).
Table 1.
Characteristics of sample and difference between Low and High HBM score.
| Total n=95 | Low HBM n=43 | High HBM n=52 | p | Crude OR | p | Adjusted OR | p | ||
| 1) Questionnaire compiler, n (%) | Mother | 80 (89%) | 37 (91%) | 43 (88%) | 0.782 | ref | |||
| Father | 6 (7%) | 3 (7%) | 3 (6%) | 0.86 | 0.859 | ||||
| Both Parents | 3 (3%) | 1 (2%) | 2 (4%) | 1.72 | 0.663 | ||||
| Grandparents | 1 (1%) | 0 (0%) | 1 (2%) | 1 | |||||
| 2) Civil state, n (%) | Married | 66 (81%) | 30 (79%) | 36 (84%) | 0.644 | ref | |||
| Cohabiting | 11 (14%) | 6 (16%) | 5 (12%) | 0.69 | 0.577 | ||||
| Divorced | 1 (1%) | 1 (2%) | 0 (0%) | 1 | |||||
| Single | 3 (4%) | 1 (2%) | 2 (4%) | 1.67 | 0.683 | ||||
| 3) Respondent age, mean (±SD) | 36 (6) | 34 (6) | 38 (6) | 0.002 | 1.12 | 0.004 | 1.14 | 0.006 | |
| 4) Education level, n (%) | Nothing | 1 (1%) | 0 (0%) | 1 (2%) | 0.896 | ref | |||
| Primary school | 4 (4%) | 2 (5%) | 2 (4%) | 1 | |||||
| Middle school | 43 (49%) | 18 (46%) | 25 (50%) | 1.39 | 0.641 | ||||
| High school | 31 (35%) | 14 (36%) | 17 (34%) | 1.21 | 0.79 | ||||
| University | 10 (11%) | 5 (13%) | 5 (10%) | 1 | |||||
| 5) Healthcare worker, n (%) | Yes | 5 (5%) | 3 (7%) | 2 (4%) | 0.479 | ref | |||
| 6) Country, n (%) | Other | 6 (7%) | 1 (2%) | 5 (10%) | 0.148 | 0.52 | 0.485 | 0.57 | 0.595 |
| Italian | 85 (93%) | 40 (98%) | 45 (90%) | ref | |||||
| 7) Number of family members, mean (±SD) | 4 (1) | 4 (1) | 4 (1) | 0.115 | 0.22 | 0.182 | 0.26 | 0.261 | |
| 8) Information source, n (%) | Pediatrician | 88 (93%) | 40 (95%) | 48 (92%) | 0.220 | 1.51 | 0.12 | 0.96 | 0.900 |
| Local Health Unit Vaccination Service | 2 (2%) | 0 (0%) | 2 (4%) | ref | |||||
| Book/newspaper | 1 (1%) | 0 (%) | 1 (2%) | 1 | |||||
| Other physician | 2 (2%) | 2 (5) | 0 (0%) | 1 | |||||
| Social network | 1 (1%) | 0 (0%) | 1 (2%) | 1 | |||||
| 9) Health Literacy level, n (%) | Low | 33 (35%) | 11 (26%) | 22 (42%) | 0.133 | 1 | |||
| Medium | 27 (28%) | 16 (37%) | 11 (21%) | ref | ref | ||||
| High | 35 (37%) | 16 (37%) | 19 (37%) | 0.34 | 0.047 | 0.31 | 0.067 | ||
| 10) Did you delay in exavalent/MMRV vaccination uptake? | Yes | 8 (8%) | 4 (9%) | 4 (8%) | 0.540 | 0.59 | 0.30 | 0.50 | 0.245 |
| Missing answer: question 1=5 , question 2= 14, question 4=6, question 6=4, question 8=1 | |||||||||
The age of respondents was the only characteristics that significantly differ between respondents with higher and lower HBM scores (38 vs 34 years old, p=0.002).
A multivariate analysis was performed in order to assess the association of demographic characteristics and HL level with the HBM scores. The age of respondents was significantly associated with higher score of HBM (OR= 1.14, p=0.006) after controlling for variables with p-level < 0.5 at univariate analysis (working as healthcare worker; country; number of family members; vaccination information source; HL level).
The reason for delay hexavalent or MMRV vaccination by parents were reported in Figure 1. The more frequent cause declared was fear of adverse reaction (87%), while only one parent expressed difficulties in vaccination services access (13%).
Figure 1.
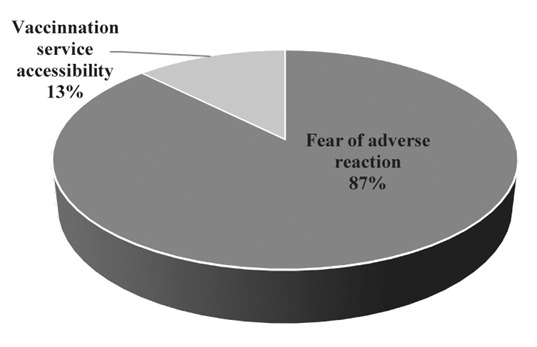
Reason of parents who delayed hexavalent and MMRV vaccination in kindergarten of Palermo.
Discussion
The “Sportello vaccinale” project demonstrated that vaccination is a widely accepted and a shared practice among parents with children attending kindergarten in the city of Palermo. Indeed, the majority of parents did not express doubts about the need to carry out all the available vaccinations.
Notwithstanding, the parents’ concerns, in our sample, were largely aimed at the possible adverse reactions that could arise: the doubt on vaccines was induced from uncertainty about its safety, rather than doubts about its efficacy. A recent American review on the vaccine beliefs of parents had similarly demonstrated that concerns about vaccines safety were the most commonly reported by parents (16). In another study conducted in 67 countries, although the opinion on vaccination is generally positive, confidence in them is very fragile. The highest levels of mistrust have been recorded in Europe, specifically in France, where 41% of respondents said they did not consider vaccines a safe medical device (17). In the sample of parents enrollend in the study, there was the opinion that vaccination is often performed following the advice of the pediatrician, or to fulfill the obligation, but without a real awareness of the benefits deriving from it. As evidenced by an American study (18) on the “vaccine hesitancy” and by a Cochrane review (19) about the importance of vaccination counselling for parents, the interventions in this area should not only be aimed at parents who totally postpone or reject vaccinations, but must also they aim to reassure and resolve the concerns of those families who, although they have decided to carry out all the vaccines, they have doubts about it. This category of subjects is susceptible to misinformation often conveyed by the media and social networks which, by giving partial or incorrect information, lead to a lack of confidence in vaccinations and institutions (20-22).
Among the safety doubt that led to delay vaccination, the false association between vaccines and autism insurgence, despite the study by Wakefield has already been withdrawn and widely denied for years, was reported in our sample (23). Moreover, also precautionary measures adopted by the Italian Health Ministry were often misunderstood by general population, as observed with the “Fluad” case. It occurred during the influenza season 2014-2015, when two batches of influenza vaccine were withdrawn following the report of three death of elderly a few days after vaccination. Although the withdrawal was just a preventive measure, and then the batches proved to be perfectly compliant, the vaccination campaign marked a dramatic drop in adherence (24, 25). In that case, the refusal of influenza vaccination was independent of the Health Literacy profile, the level of schooling or medical knowledge, but mainly due to the incorrect information given by Public Health Authorities following the withdrawal of the vaccine and the media coverage attention reserved for the event (24).
The main result of the study was the strong correlation between a high degree of HBM and older people. This is a topic widely reflected in the literature with preventive strategies or medications adherence, as a study carried out on antiretroviral therapy compliance in HIV + subjects, where the rate of low treatment adherence in the sample of the youngest people was almost double than recorded in the older patients (26). In a recent Chinese study, older parents performed significantly better on knowledge (p < 0.001) and awareness (p < 0.001) about papillomavirus vaccination than younger (27). It is likely that a greater age is related to higher responsibility and awareness of what the diseases covered by the vaccine have involved in the past. Today, that the relationship with the doctor has often become conflicting and the trust towards healthcare is always lower, it is necessary to find a meeting point with families, to provide clear and complete information to anyone who is hesitant and, above all, to demonstrate how vaccination represents a safe practice (28, 29).
Despite the fact that usually population with a high level of HL correlates better with adherence to preventive strategies, considering vaccination topic it was often observed a paradox with parents with higher HL levels that not vaccinate their children (30, 31). Also, in our study there is no evidence of a correlation between HL levels and a higher propensity towards preventive strategies, probably because there are many factors to consider and the HL alone does not guarantee reassurance for the numerous questions presented by families (32). A review of 2018 shows that HL in vaccination choices seems to be influenced by various factors such as the country of origin, age and type of vaccine (33). Therefore, it seems appropriate to support parents in making vaccination a voluntary and conscious choice with deepening counselling activities conducted with the first time younger parents (34).
The main limitations of the study is the low sample of people recruited in the project and missing answer in the questionnaire. Notwithstanding, the study threats knowledge and attitude of people about vaccination a year after the introduction of mandatory vaccination introduction in Italy, that is a topic rarely treated in the literature.
This study gave the opportunity to explore parents’ beliefs about vaccinations using the HBM methodology. Consent to vaccination practice was widely represented, but at the same time the results highlighted the need for parents to have more information and more time devoted to the practice of vaccination counseling. Moreover, significantly positive association emerged between the age of the parents and a higher grade of HBM. While no correspondence was found between the level of Health Literacy and the propensity towards vaccination.
The project carried out in the kindergartens, which also included a large part of counseling activities, was pleasantly received by the parents. Implementing counselling activities at school or at the vaccination service, could support an aware decision process of the parents on vaccination topic.
Conflict of interest:
Each author declares that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangement etc.) that might pose a conflict of interest in connection with the submitted article
References
- 1.World Healh Organization. Report of the SAGE Working Group on Vaccine Hesitancy. 2014 Available online: https://www.who.int/immunization/sage/meetings/2014/october/1_Report_WORKING_GROUP_vaccine_hesitancy_final.pdf. (accessed 12 January 2019) [Google Scholar]
- 2.MacDonald NE, Desai S, Gerstein B. Working with vaccine-hesitant parents: An update. Paediatr Child Health. 2018;23(8):561–562. doi: 10.1093/pch/pxy144. doi: 10.1093/pch/pxy144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.WHO. Measles – European Region Disease outbreak news - update 6 May 2019. Available online: https://www.who.int/csr/don/06-may-2019-measles-euro/en. / (accessed 13th of January 2020. [Google Scholar]
- 4.Rechel B, Richardson E, McKee M. The organization and delivery of vaccination services in the European Union. European Observatory on Health Systems and Policies. 2018 Available online: http://www.euro.who.int/__data/assets/pdf_file/0008/386684/vaccination-report-eng.pdf?ua=1. (accessed. [Google Scholar]
- 5.Ministero della Salute. Piano Nazionale Prevenzione Vaccinale PNPV 2017-2019. 2017 Available online: http://www.salute.gov.it/imgs/C_17_pubblicazioni_2571_allegato.pdf( accessed 12 January 2020) [Google Scholar]
- 6.Istituto Superiore di Sanità. Morbillo & Rosolia News. Rapporto N°37 - Gennaio. 2018 Available online: http://www.salute.gov.it/portale/temi/documenti/morbillo/Bollettino_morbillo_37-2018.pdf. (accessed 12 Jan 2020) [Google Scholar]
- 7.Istituto Superiore di Sanità. Morbillo & Rosolia News. Rapporto N°48 - Gennaio. 2019 Available online: https://www.epicentro.iss.it/morbillo/bollettino/RM_News_2018_48%20def.pdf. (accessed 12 Jan 2020) [Google Scholar]
- 8.Ministero della Salute. Vaccinali dell’età pediatrica e dell’adolescente - Coperture vaccinali. 2019 Available online: http://www.salute.gov.it/imgs/C_17_tavole_20_allegati_iitemAllegati_0_fileAllegati_itemFile_7_file.pdf. (accessed 12 Jan 2020) [Google Scholar]
- 9.Presidente della Repubblica. Legge 31 luglio 2017, n. 119, 2017. Available online: http://www.trovanorme.salute.gov.it/norme/dettaglioAtto?id=60201. (accessed 12 Jan 2020) [Google Scholar]
- 10.Rezza G. Mandatory vaccination for infants and children: the Italian experience. Pathog Glob Health. 2019:1–6. doi: 10.1080/20477724.2019.1705021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Signorelli C. Forty years (1978-2018) of vaccination policies in Italy. Acta Biomed. 2019;90(1):127–133. doi: 10.23750/abm.v90i1.7900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Janz NK, Becker MH. The Health Belief Model: a decade later. Health Educ Q. 1984 Spring;11(1):1–47. doi: 10.1177/109019818401100101. [DOI] [PubMed] [Google Scholar]
- 13.Rudd RE. Health Literacy: Insights and Issues. Stud Health Technol Inform. 2017;240:60–78. [PubMed] [Google Scholar]
- 14.Rawson KA, Gunstad J, Hughes J, et al. The METER: a brief, self-administered measure of health literacy. J Gen Intern Med. 2010;25(1):67–71. doi: 10.1007/s11606-009-1158-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Biasio LR, Corbellini G, D’Alessandro D. An Italian validation of “meter”, an easy-to-use Health Literacy (hl) screener. Ann Ig. 2017;29(3):171–178. doi: 10.7416/ai.2017.2144. [DOI] [PubMed] [Google Scholar]
- 16.Gidengil C, Chen C, Parker AM, Nowak S, Matthews L. Beliefs around childhood vaccines in the United States: A systematic review. Vaccine. 2019;37(45):6793–6802. doi: 10.1016/j.vaccine.2019.08.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Larson HJ, de Figueiredo A, Xiahong Z, et al. The State of Vaccine Confidence 2016: Global Insights Through a 67-Country Survey. EBioMedicine. 2016;12:295–301. doi: 10.1016/j.ebiom.2016.08.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Salmon DA, Dudley MZ, Glanz JM, Omer SB. Vaccine hesitancy: Causes, consequences, and a call to action. Vaccine. 2015;33 Suppl 4:D66–71. doi: 10.1016/j.vaccine.2015.09.035. [DOI] [PubMed] [Google Scholar]
- 19.Kaufman J, Ryan R, Walsh L, et al. Face-to-face interventions for informing or educating parents about early childhood vaccination. Cochrane Database Syst Rev. 2018;5:CD010038. doi: 10.1002/14651858.CD010038.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tabacchi G, Costantino C, Cracchiolo M, et al. Information sources and knowledge on vaccination in a population from southern Italy: The ESCULAPIO project. Hum Vaccin Immunother. 2017;13(2):339–345. doi: 10.1080/21645515.2017.1264733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Restivo V, Napoli G, Marsala MG, et al. Factors associated with poor adherence to MMR vaccination in parents who follow vaccination schedule. Hum Vaccin Immunother. 2015;11(1):140–5. doi: 10.4161/hv.34416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Restivo V, Vizzini G, Mularoni A, Di Benedetto C, Gioè SM, Vitale F. Determinants of influenza vaccination among solid organ transplant recipients attending Sicilian reference center. Hum Vaccin Immunother. 2017;13(2):346–350. doi: 10.1080/21645515.2017.1264792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Crenna S, Osculati A, Visonà SD. Vaccination policy in Italy: An update. J Public Health Res. 2018;7(3):1523. doi: 10.4081/jphr.2018.1523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Signorelli C, Odone A, Conversano M, Bonanni P. Deaths after Fluad flu vaccine and the epidemic of panic in Italy. BMJ. 2015;350:h116. doi: 10.1136/bmj.h116. [DOI] [PubMed] [Google Scholar]
- 25.Restivo V, Cernigliaro A, Palmeri S, Sinatra I, Costantino C, Casuccio A. The Socio-Economic Health Deprivation Index and its association with mortality and attitudes towards influenza vaccination among the elderly in Palermo, Sicily. J Prev Med Hyg. 2019 doi: 10.15167/2421-4248/jpmh2018.59.4s2.1074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Barclay TR, Hinkin CH, Castellon SA. Age-associated predictors of medication adherence in HIV-positive adults: health beliefs, self-efficacy, and neurocognitive status. Health Psychol. 2007;26(1):40–9. doi: 10.1037/0278-6133.26.1.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhou M, Qu S, Zhao L, Campy KS, Wang S. Parental perceptions of human papillomavirus vaccination in central China: the moderating role of socioeconomic factors. Hum Vaccin Immunother. 2019;15(7-8):1688–1696. doi: 10.1080/21645515.2018.1547605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Restivo V, Orsi A, Ciampini S, et al. How should vaccination services be planned, organized, and managed? Results from a survey on the Italian vaccination services. Ann Ig. 2019;31(2 Supple 1):45–53. doi: 10.7416/ai.2019.2276. [DOI] [PubMed] [Google Scholar]
- 29.Restivo V, Costantino C, Mammina C, Vitale F. Influenza like Illness among Medical Residents Anticipates Influenza Diffusion in General Population: Data from a National Survey among Italian Medical Residents. PLoS One. 2016;11(12):e0168546. doi: 10.1371/journal.pone.0168546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Amit Aharon A, Nehama H, Rishpon S, Baron-Epel O. Parents with high levels of communicative and critical health literacy are less likely to vaccinate their children. Patient Educ Couns. 2017;100(4):768–775. doi: 10.1016/j.pec.2016.11.016. [DOI] [PubMed] [Google Scholar]
- 31.Biasio LR. Vaccine hesitancy and health literacy. Hum Vaccin Immunother. 2017;13(3):701–702. doi: 10.1080/21645515.2016.1243633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cernigliaro A, Palmeri S, Casuccio A, Scondotto S, Restivo V In Primis Working Group. Association of the Individual and Context Inequalities on the Breastfeeding: A Study from the Sicily Region. Int J Environ Res Public Health. 2019;16(19) doi: 10.3390/ijerph16193514. pii: E3514. d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lorini C, Santomauro F, Donzellini M. Health literacy and vaccination: A systematic review. Hum Vaccin Immunother. 2018;14(2):478–488. doi: 10.1080/21645515.2017.1392423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Restivo V, Costantino C, Giorgianni G, et al. Case-control study on intestinal intussusception: implications for anti-rotavirus vaccination. Expert Rev Vaccines. 2018;17(12):1135–1141. doi: 10.1080/14760584.2018.1546122. [DOI] [PubMed] [Google Scholar]


