To the Editor,
the diagnosis of intraductal papillary mucinous neoplasms (IPMNs) is a field of great interest for researchers, since several innovative techniques have been arised in the last decade to detect such lesions.
We read with great pleasure the review “Diagnosis and management of intraductal papillary mucinous neoplasms of the pancreas” published on Your journal by Cortegoso Valdivia P. et al, highlightening the most recent evidences about the diagnosis and management of IPMNs (Acta Biomed. 2018 Dec 17;89(9-S):147-152) (1).
First of all, we would like to thank with the authors for this well organized review. In the Results section, the authors take into consideration different strategies for the diagnosis of IPMNs1. In particular, in the current era, pancreatoscopy with the innovative digital single-operator system cholangioscopes (such as SpyGlass™, Boston Scientific Corp, Marlborough, USA) represents a landmark for the detection of IPMNs (2,3). Nevertheless, direct peroral pancreatoscopy (DPOP) through ultra-slim endoscope continues representing a good alternative, thanks to higher-resolution images, a less fragility of the endoscope, the availability to perform high-intensity contrast imaging (e.g, Narrow-Banding Imaging or Blu-Light Imaging) and, finally, the possibility to use an larger size working channel (thus allowing adequate tissue samples)(2-4).
However, the usefulness of DPOP is critically related to the ability of the operator in keeping a stable position of ultraslim endoscope, due to its lack of stiffness. These inherent limitation has led endoscopists to adopt ancillary accessories in order to achieve an optimal insertion of the ultra-slim endoscope within the main pancreatic duct (MPD): guidewires, duodenal balloons, overtube balloons, intraductal balloon and the recently described Huang YH et al’ snare-assisted method (3,4).
Recently, in our referral center for biliopancreatic disease treatment, a novel “self-made” technique was adopted in order to introduce an ultraslim endoscope within the MPD. Since an intraductal papillary mucinous neoplasm (IPMN) was suspected after performing an endoscopic ultra-sound, we decided to perform some biopsies of this pancreatic mass, but, unfortunately, no digital single-operator system cholangioscope was available in our center, yet (Fig. a1). After performing an large-size endoscopic sphincterotomy, a thin endoscope was used to obtain a direct visualization of the pancreatic lumen (Fig. 1b). After several attempts to introduce the tip of the endoscope inside the pancreatic orifice, we realized that the main difficulties were related to the following two aspects: first, the acute angle between the second part of the duodenum and the MPD access; second, the formation of a large loop inside the gastric lumen (due to the lack of stiffness of the instrument). We overcame both these limitations through a disposable endoscopic-biopsy forcep running inside the working channel, thus playing a double role: first, stiffening the instrument, (providing an optimal stable position of the endoscope within the pancreatic duct) and, second, allowing to obtain good quality biopsies of an endoluminal pancreatic mass (suspected for IPMN) (Fig. 1c, 1d).
Figure 1.
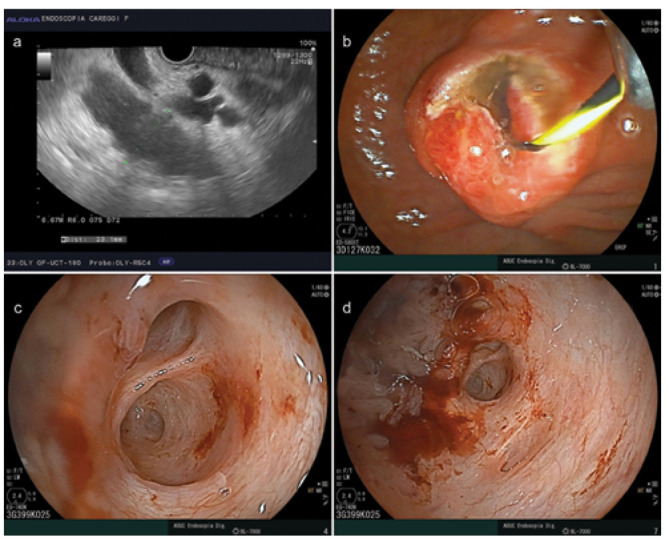
1a) Endoscopic ultra-sound (EUS) finding suspected for a pancreatic intraductal papillary mucinous neoplasm; 1b) Large-size endoscopic sphincterotomy, with the guide-wire inside the pancreatic duct; 1c, 1d) Peroral direct visualization of the pancreatic lumen with the thin endoscope, revealing the pancreatic mass.
To our knowledge, this is the first report in literature concerning the use of a disposable grasping forcep as an ancillary-tool to assist DPOP (2-5). We think this stretegy, beyond the ones described by Cortegoso Valdivia P. et al, might represent a further diagnostic methods in case of IPMNs (1). We hope our idea could be adopted by other endoscopists, whenever an easy and cheap technique is required to perform direct MPD exploration with an ultra-slim endoscope.
Conflict of interest:
Each author declares that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangement etc.) that might pose a conflict of interest in connection with the submitted article.
Informed consent:
A written informed consent form was obtained before performing the surgical operation.
Authors’ contributions:
Damiano Bisogni, Michele Rossi, Fabio Staderini: substantial contributions to conception and design, writing the study, drafting the article, final approval of the version to be published. Giancarlo Freschi, Roberto Manetti, Luca Talamucci: study design, drafting the article, final approval of the version to be published.
References
- 1.Cortegoso Valdivia P, Chialà C, Venezia L, et al. Diagnosis and management of intraductal papillary mucinous neoplasms of the pancreas. Acta Biomed. 2018 Dec 17;89(9-S):147–152. doi: 10.23750/abm.v89i9-S.7958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ayoub F, Yang D, Draganov PV. Cholangioscopy in the digital era. Transl Gastroenterol Hepatol. 2018 Oct 29;3:82. doi: 10.21037/tgh.2018.10.08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Huang YH, Chang H, Yao W, Zhang YP, Li K, Wang Y. A snare-assisted peroral direct choledochoscopy and pancreatoscopy using an ultra-slim upper endoscope: A case series study. Dig Liver Dis. 2017 Jun;49(6):657–663. doi: 10.1016/j.dld.2017.01.150. [DOI] [PubMed] [Google Scholar]
- 4.Zou XP, Zhang M, Li W, Wu YL. Biliary intraductal papillary-mucinous neoplasm diagnosed by peroral direct cholangioscopy using a slim upper endoscope (with video) Surg Laparosc Endosc Percutan Tech. 2011 Oct;21(5):e263–5. doi: 10.1097/SLE.0b013e318225d145. [DOI] [PubMed] [Google Scholar]
- 5.Cheon YK, Moon JH, Choi HJ, Lee JE, Lee YN, Cho YD, et al. Direct peroral pancreatoscopy with an ultraslim endoscope for the evaluation of intraductal papillary mucinous neoplasms. Endoscopy. 2011;43(Suppl 2 UCTN):E390–1. doi: 10.1055/s-0030-1256933. [DOI] [PubMed] [Google Scholar]


