Abstract
Background:
Because of invasive nature of catheterization, using other noninvasive tools is more preferred to assess pulmonary arterial hypertension (PAH). The present study assessed the value of chest spiral CT scan and Doppler echocardiography compared to right heart catheterization (RHC) to predict PAH in patients with scleroderma.
Methods:
This cross-sectional study was performed on 15 patients with limited scleroderma. All subjects underwent Doppler echocardiography (to assess PAP) and chest spiral CT scan without injection (to assess pulmonary trunk length or PUL), followed by RHC to assess PAH.
Results:
Comparing PUL in spiral CT scan with PAP in RHC yielded a sensitivity of 75.0% and a specificity of 100% for predicting PAH. Similarly, comparing PAP value in echocardiography with PAP in RHC achieved a sensitivity of 100% and a specificity of 63.6% to discriminate PAH from normal PAP condition. Analysis of the area under the ROC curve showed high power of CT scan to predict PAH (AUC = 1.000). The best cutoff point for PUL to predict PAH was 29.95 yielding a sensitivity of 100% and a specificity of 100%. Also, ROC curve analysis showed high value of echocardiography to discriminate PAH from normal PAP status (AUC = 0.841) that considering a cutoff value of 22.88 for PAP assessed by echocardiography reached to a sensitivity of 72.7% and a specificity of 100%.
Conclusion:
Both chest spiral CT scan and Doppler echocardiography are very useful to diagnose PAH and its severity in patients with scleroderma. (www.actabiomedica.it)
Keywords: Catheterization, Spiral CT scan, Doppler echocardiography, Pulmonary arterial hypertension
Introduction
Pulmonary arterial hypertension (PAH) is mainly caused by the increase in pulmonary vascular resistance (PVR) due to proliferation and contraction of vascular smooth muscle cells. This event not only can be revealed in cardiovascular and pulmonary disorders, but also it is a dominant complication in scleroderma. Based on the diagnostic criteria in right heart catheterization (RHC), the overall prevalence of PAH in scleroderma ranged 8 to 12 percent (1-4). Although PAH is a common finding in various types of scleroderma, some potential risk factors have been also identified for PAH including the number of telangiectasias (5-7), reduced capillary nailfold density (8), anticentromere antibodies, antitopoisomerase antibodies, male sex, underlying pulmonary fibrosis and Raynaud’s phenomenon of greater than 3 years’ duration. To early diagnose PAH in patients with systemic sclerosis, not only pulmonary artery pressure (PAP), pulmonary capillary wedge pressure, and left-ventricular end-diastolic pressure should be estimated, but also all cardiopulmonary hemodynamics such as systolic and diastolic functional parameters should be properly assessed (9). Applying an accurate tool for diagnosis of PAH especially in scleroderma is necessary and vital because it has an aggressive pattern with an extremely poor prognosis in these patients. In fact, PAH in scleroderma patients is accounted for 30% of deaths leading a median survival time of 1 year following diagnosis (10-12). RHC is now the specific available method for diagnosis of PAH and its severity. The importance of this tool is related to the simultaneous assessment of cardiac and pulmonary functional status. In fact, along with the estimation of PAP, right atrial–right ventricle gradient, however, other tools that have been recently considered to be valuable including pulmonary function testing, including measurement of DLCO, chest radiograph, CT pulmonary angiography or ventilation/perfusion lung scan, and HRCT scan (13). However, because of invasive nature of catheterization, the use of other noninvasive tools is more preferred by both patient and physician. However, it must not sacrifice accuracy for simplicity and thus determining the value of noninvasive methods such as CT scan or echocardiography for assessment of PAH in scleroderma patients is necessary. The present study thus assessed the value of chest spiral CT scan and Doppler echocardiography compared to RHC to predict PAH in patients with scleroderma.
Materials and Methods
This cross-sectional study was performed on 15 patients with limited scleroderma that referred for ruling out of PAH to a hospital in Tehran between 2013 and 2014. Informed consent form was obtained from all patients and the rights of the patients were protected.
Scleroderma was diagnosed according to the preliminary criteria of the American Rheumatology Association (14). The exclusion criteria were history of known cardiopulmonary disorders, or any history of cigarette or opium smoking. On admission, baseline characteristics including demographics, medical history, findings of physical examination, and laboratory parameters were collected from the recorded files or by examining the patients. All subjects underwent Doppler echocardiography to determine the following criteria: left ventricular ejection fraction (LVEF), left and right ventricular size, systolic and mean PAP as well as heart valves status. Then, chest spiral CT scan without injection was requested for all to measure the size of main pulmonary artery and also left and right branches of this artery as well as any abnormal changes in pulmonary parenchyma. The patients finally underwent RHC to assess the following indices: systolic PAP, diastolic PAP, mean PAP, PCWP, right ventricular pressure, right atrial pressure, aortic pressure, systolic left ventricular pressure and left ventricular end diastolic pressure.
PAH was defined according to echocardiography as mean PAP ≥ 25 mmHg and systolic PAP ≥ 40 mmHg. Also, those with mean PAP ≥ 25 mmHg in RHC or main pulmonary artery length (PUL) ≥ 29 mm in spiral CT were also considered as PAH.
The study endpoint was to assess the predictive value of both tools of Doppler echocardiography and chest spiral CT scan without injection in comparison with RHC to predict PAH in the patients. For statistical analysis, results were presented as mean ± standard deviation (SD) for quantitative variables and were summarized by absolute frequencies and percentages for categorical variables. Normality of data was analyzed using the Kolmogorov-Smirnoff test. Categorical variables were compared using chi-square test or Fisher’s exact test when more than 20% of cells with expected count of less than 5 were observed. Quantitative variables were also compared with t test or Mann-Whitney U test. The ROC curve analysis was applied to determine the value of two pointed procedures to discriminate PAH from normal PAP status. Then the best cutoff value for PAP parameter was determined to yield the optimized sensitivity and specificity. For the statistical analysis, the statistical software SPSS version 16.0 for windows (SPSS Inc., Chicago, IL) was used. P values of 0.05 or less were considered statistically significant.
Results
Comparing PUL in spiral CT scan with PAP in RHC yielded a sensitivity of 75.0%, a specificity of 100%, a positive predictive value (PPV) of 100%, a negative predictive value (NPV) of 91.7% and an accuracy of 93.3% for spiral CT for predicting PAH. Similarly, comparing PAP value in echocardiography with PAP in RHC achieved a sensitivity of 100%, a specificity of 63.6%, a PPV of 50.0%, a NPV of 100% and an accuracy of 73.3% for echocardiography to discriminate PAH from normal PAP condition. Assessing the agreement between spiral CT scan of the chest and echocardiography to assess PAH led to a partially significant but poor agreement between the two procedures (kappa value of 0.359, p = 0.070). However, there was a strong agreement between PAP in RHC and PAP in echocardiography (r = 0.884, p < 0.001) as well as between PAP in RHC and PUL in CT scan (r = 0.754, p < 0.001) (Figures 1 and 2). Analysis of the area under the ROC curve showed high power of CT scan to predict PAH (AUC = 1.000, P < 0.001). The best cutoff point for PUL to predict PAH was 29.95 yielding a sensitivity of 100% and a specificity of 100%. Also, ROC curve analysisshowed high value of echocardiography to discriminate PAH from normal PAP status (AUC = 0.841, P < 0.001) that considering a cutoff value of 22.88 for PAP assessed by echocardiography reached to a sensitivity of 72.7% and a specificity of 100%.
Figure 1.
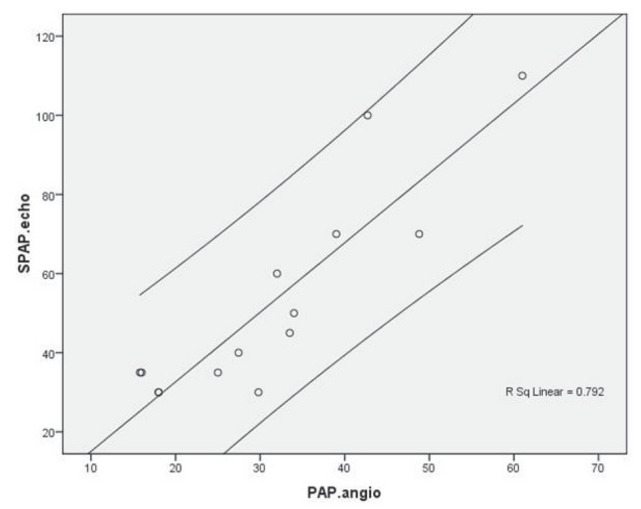
Correlation between PAP in RHC and PAP in Doppler echocardiography
Figure 2.
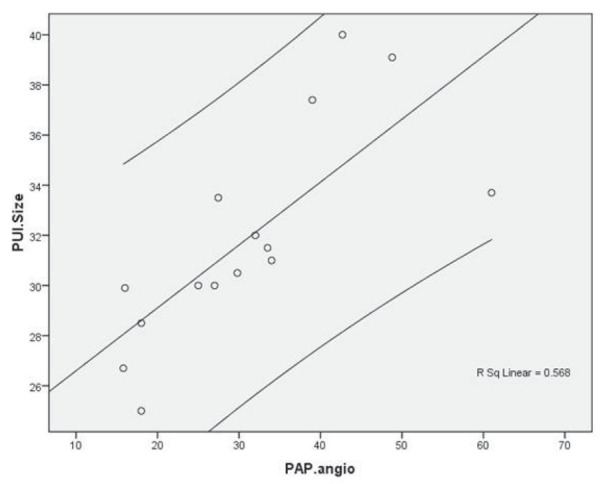
Correlation between PAP in RHC and PUL in chest spiral CT scan
Discussion
Although several studies have assessed the diagnostic value of echocardiography versus RHC in predicting PAH, but a few studies focused scleroderma subgroups. In general, a meta-analysis by Janda et al in 2011 on 29 previous studies (15) showed that the summary sensitivity and specificity for echocardiography for diagnosing pulmonary hypertension was 83% and 72%, respectively that was lower than the values obtained in our study regarding a study subgroup of scleroderma patients. However they also emphasized to use RHC as the gold standard to assess PAH more accurately. In another meta-analysis in 2013 by Taleb et al (16), the correlation between PAP estimated by Doppler echocardiography and RHC ranged from r = 0.65 to r = 0.97 with the pooled sensitivity, specificity, and accuracy of Doppler echocardiography as 88%, 56%, and 63%, respectively. Doppler echocardiography is a noninvasive modality in the screening and evaluation of PAH (17). This tool can successfully assess right-sided heart chamber size and its function. Mainly, Doppler echocardiography estimates the right ventricular systolic pressure by estimating the pressure gradient between the right ventricle and the right atrium. When an estimated right atrial pressure is added to this number, it can be approximated the right ventricular systolic pressure that is equal to the PAP measure. In this regard, a good correlation between PAP assessed by RHC and estimated by Doppler echocardiography can be explained (18,19). Although this powerful correlation is expected in general particularly in some settings such as scleroderma patients subgroup (as shown in our study), but, lower accuracy of Doppler echocardiography in some certain clinical settings remained questioned (20, 21).
According to our study results, the power of chest spiral CT scan without injection to predict PAH was even higher than Doppler echocardiography. In total, high-resolution CT scans is very helpful for diagnosing idiopathic PAH and detecting and identifying disorders underlying secondary PAH. In this regard, the characteristic morphologic CT features of PAH include dilatation of the pulmonary artery trunk, dilatation of the right and left main pulmonary arteries; abrupt narrowing and tapering of the peripheral pulmonary vessels; right ventricular hypertrophy; and right ventricular and atrial enlargement(22). The presence of a distal main pulmonary artery with a CT-demonstrated diameter greater than or equal to 29 mm at its widest point has a PPV of more than 95% and a specificity of 89%. In total and according to our results, this noninvasive tool can be the best procedure for predicting PAH similar to obtained using RHC. In fact, chest spiral CT scan is a reliable method to predict PAH when the CT-demonstrated diameter of the distal main pulmonary artery is greater than or equal to 29 mm with even a specificity of 100% (23). However, it seems that the accuracy of this tool may be affected by some factors such as patients’ age (24) and therefore the diagnostic performance of chest spiral CT scan should be reassessed by considering these variables.
Conclusion
In conclusion, both chest spiral CT scan and Doppler echocardiography are very useful to diagnose PAH and its severity in patients with scleroderma.
Acknowledgement:
The authors would like to thank the Rasool Akram Medical Complex Clinical Research Development Center (RCRDC) for its technical and editorial assists.
Conflict Of Interest:
Each author declares that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangement etc.) that might pose a conflict of interest in connection with the submitted article
References
- 1.Hachulla E, Gressin V, Guillevin L, Carpentier P, Diot E, Sibilia J, et al. Early detection of pulmonary arterial hypertension in systemic sclerosis: a French nationwide prospective multicenter study. Arthritis Rheum. 2005;52:3792–800. doi: 10.1002/art.21433. [DOI] [PubMed] [Google Scholar]
- 2.Mukerjee D, St George D, Coleiro B, Knight C, Denton CP, Davar J, et al. Prevalence and outcome in systemic sclerosis associated pulmonary arterial hypertension: application of a registry approach. Ann Rheum Dis. 2003;62:1088–93. doi: 10.1136/ard.62.11.1088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Phung S, Strange G, Chung LP, Leong J, Dalton B, Roddy J, et al. Prevalence of pulmonary arterial hypertension in an Australian scleroderma population: screening allows for earlier diagnosis. Intern Med J. 2009;39:682–91. doi: 10.1111/j.1445-5994.2008.01823.x. doi: 10.1111/j.1445-5994.2008.01823.x. [DOI] [PubMed] [Google Scholar]
- 4.Avouac J, Airò P, Meune C, Beretta L, Dieude P, Caramaschi P, et al. Prevalence of pulmonary hypertension in systemic sclerosis in European Caucasians and meta-analysis of 5 studies. J Rheumatol. 2010;37:2290–8. doi: 10.3899/jrheum.100245. [DOI] [PubMed] [Google Scholar]
- 5.Cox SR, Walker JG, Coleman M, Rischmueller M, Proudman S, Smith MD, et al. Isolated pulmonary hypertension in scleroderma. Intern Med J. 2005;35:28–33. doi: 10.1111/j.1445-5994.2004.00646.x. [DOI] [PubMed] [Google Scholar]
- 6.Robert-Thomson PJ, Mould TL, Walker JG, Smith MD, Ahern MJ. Clinical utility of telangiectasia of hands in scleroderma and other rheumatic disorders. Asian Pac J Allergy Immunol. 2002;20:7–12. [PubMed] [Google Scholar]
- 7.Shah AA, Wigley FM, Hummers LK. Telangiectases in scleroderma: a potential clinical marker of pulmonary arterial hypertension. J Rheumatol. 2010;37:98–104. doi: 10.3899/jrheum.090697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ong YY, Nikoloutsopoulos T, Bond CP, Smith MD, Ahern MJ, Roberts-Thomson PJ. Decreased nailfold capillary density in limited scleroderma with pulmonary hypertension. Asian Pac J Allergy Immunol. 1998;16:81–6. [PubMed] [Google Scholar]
- 9.Gaine S, Gibbs JS, Gomez-Sanchez MA, Jondeau G, Klepetko W, Opitz C, et al. Guidelines for the diagnosis and treatment of pulmonary hypertension. Eur Respir J. 2009;34:1219–63. doi: 10.1183/09031936.00139009. [DOI] [PubMed] [Google Scholar]
- 10.Steen V, Medsger TA Jr. Predictors of isolated pulmonary hypertension in patients with systemic sclerosis and limited cutaneous involvement. Arthritis Rheum. 2003;48:516–22. doi: 10.1002/art.10775. [DOI] [PubMed] [Google Scholar]
- 11.Kawut SM, Taichman DB, rcher-Chicko CL, Palevsky HI, Kimmel SE, et al. Hemodynamics and survival in patients with pulmonary arterial hypertension related to systemic sclerosis. Chest. 2003;123:344–50. doi: 10.1378/chest.123.2.344. [DOI] [PubMed] [Google Scholar]
- 12.Koh ET, Lee P, Gladman DD, bu-Shakra M. Pulmonary hypertension in systemic sclerosis: an analysis of 17 patients. Br J Rheumatol. 1996;35:989–93. doi: 10.1093/rheumatology/35.10.989. [DOI] [PubMed] [Google Scholar]
- 13.Rich S. Primary pulmonary hypertension. Curr Treat Options Cardiovasc Med. 2000;2:135–40. doi: 10.1007/s11936-000-0006-1. [DOI] [PubMed] [Google Scholar]
- 14.Preliminary criteria for the classification of systemic sclerosis (scleroderma) Subcommittee for Scleroderma Criteria of the ARA Diagnostic and Therapeutic Criteria Committee. Arthritis Rheum. 1980;23:581–90. doi: 10.1002/art.1780230510. [DOI] [PubMed] [Google Scholar]
- 15.Janda S, Shahidi N, Gin K, Swiston J. Diagnostic accuracy of echocardiography for pulmonary hypertension: a systematic review and meta-analysis. Heart. 2011;97:612–22. doi: 10.1136/hrt.2010.212084. [DOI] [PubMed] [Google Scholar]
- 16.Taleb M, Khuder S, Tinkel J, Khouri SJ. The diagnostic accuracy of Doppler echocardiography in assessment of pulmonary artery systolic pressure: a meta-analysis. Echocardiography. 2013;30:258–65. doi: 10.1111/echo.12061. [DOI] [PubMed] [Google Scholar]
- 17.Raymond RJ, Hinderliter AL, Willis PW, Ralph D, Caldwell EJ, Williams W, et al. Echocardiographic predictors of adverse outcomes in primary pulmonary hypertension. J Am Coll Cardiol. 2002;39:1214–9. doi: 10.1016/s0735-1097(02)01744-8. [DOI] [PubMed] [Google Scholar]
- 18.Berger M, Haimowitz A, Van Tosh A, Berdoff RL, Goldberg E. Quantitative assessment of pulmonary hypertension in patients with tricuspid regurgitation using continuous wave Doppler ultrasound. J Am Coll Cardiol. 1985;6:359–65. doi: 10.1016/s0735-1097(85)80172-8. [DOI] [PubMed] [Google Scholar]
- 19.Currie PJ, Seward JB, Chan KL, Fyfe DA, Hagler DJ, Mair DD, et al. Continuous wave Doppler determination of right ventricular pressure: a simultaneous Doppler-catheterization study in 127 patients. J Am Coll Cardiol. 1985;6:750–6. doi: 10.1016/s0735-1097(85)80477-0. [DOI] [PubMed] [Google Scholar]
- 20.Fisher MR, Criner GJ, Fishman AP, Hassoun PM, Minai OA, Scharf SM, et al. Estimating pulmonary artery pressures by echocardiography in patients with emphysema. Eur Respir J. 2007;30:914–21. doi: 10.1183/09031936.00033007. Epub 2007 Jul 25. [DOI] [PubMed] [Google Scholar]
- 21.Arcasoy SM, Christie JD, Ferrari VA, Sutton MS, Zisman DA, Blumenthal NP, et al. Echocardiographic assessment of pulmonary hypertension in patients with advanced lung disease. Am J RespirCrit Care Med. 2003;167:735–40. doi: 10.1164/rccm.200210-1130OC. [DOI] [PubMed] [Google Scholar]
- 22.Frazier AA, Galvin JR, Franks TJ, Rosado-de-Christenson ML. Pulmonary vasculature: hypertension and infarction. Radiographics. 2000;20:491–524. doi: 10.1148/radiographics.20.2.g00mc17491. [DOI] [PubMed] [Google Scholar]
- 23.Ng CS, Wells AU, Padley SP. A CT sign of chronic pulmonary arterial hypertension: the ratio of main pulmonary artery to aortic diameter. J Thorac Imaging. 1999;14:270–8. doi: 10.1097/00005382-199910000-00007. [DOI] [PubMed] [Google Scholar]
- 24.Tan RT, Kuzo R, Goodman LR, Siegel R, Haasler GB, Presberg KW. Utility of CT scan evaluation for predicting pulmonary hypertension in patients with parenchymal lung disease. Medical College of Wisconsin Lung Transplant Group. Chest. 1998;113:1250–6. doi: 10.1378/chest.113.5.1250. [DOI] [PubMed] [Google Scholar]


