Abstract
BACKGROUND AND PURPOSE: To investigate image quality and vascular delineation of multisection CT (MSCT) angiography of the cervicocranial vessels with sliding-thin-slab (STS) maximum intensity projections (MIP) and multiplanar reformations (MPR).
MATERIALS AND METHODS: Ten patients examined with a standardized protocol on a 16-section MSCT were included in the study. The data were reformatted as MIP and MPR in 3 planes for each subject; both reformatting techniques were applied in an STS technique with an increment of 3 mm. Images were evaluated independently by 3 blinded readers grading image quality parameters and vascular delineation of supra-aortic arteries and veins. An extension of the Mantel-Haenzel row mean score test was used to compare the distribution of scores for vascular delineation and image quality between STS MIP and STS MPR.
RESULTS: STS MIP reformations were significantly superior to STS MPR in the delineation of all extra- and intracranial arteries and arterial segments and in the delineation of the cavernous sinus and the internal cerebral veins (P < .05). No significant differences were found for the large venous vessels, the visual assessment of vascular contrast, or the impact of imaging artifacts.
CONCLUSION: Because STS MIP reformations were preferred to or equal to STS MPR in all aspects, we recommend STS MIP as the primary reformatting technique in MSCT angiography of the cervicocranial vessels in addition to viewing the source images.
The introduction of multisection CT (MSCT) has led to a steep increase in the amount of acquired data.1–3 Moreover, the acquisition of isotropic or near isotropic voxels has made the multiplanar display of the data an enticing option. Interactive viewing at a PACS console has become increasingly common in clinical routine. Thus, postprocessing methods have proportionally risen in importance even in primary diagnostic analysis.
Reformatting processes are able to present the CT voxels in off-axis views.4–7 The most simple and commonly applied reformatting methods are multiplanar reformations (MPR). In this approach, the data are sampled directly in the respective direction of interest.8 Maximum intensity projections (MIP), on the other hand, trace viewing rays from the expected operator position through the object, retaining only the relative maximum value along each ray path.8 Thus, the emphasis is put on structures with high attenuation.
Both techniques can be viewed with the aid of a sliding-thin-slab (STS) technique.8,9 Although the images are acquired at a small section thickness, they are viewed as so-called slabs by combining multiple images. This improves both noise and coplanar effects, while preserving the option to interactively scroll through the dataset on a PACS workstation. When employing an STS technique, the data are not displayed as one entire volume, as is common practice in MR angiography, but rather as slabs of sections that move through the volume of the dataset. The cross-sectional nature of the data is therefore emphasized.
In the past, the relative value of various reformatting techniques has for the most part been evaluated for the assessment of the degree of renal artery stenosis10–14 and carotid artery stenosis,15–18 yielding widely differing results and considerable controversy. These studies were generally conducted on single-section scanners and focused solely on the measurement of the degree of stenosis of the artery of interest. Moreover, for the most part they compared either MIP or MPR with a volume-rendering technique without comparing MIP and MPR with each other. In addition, most studies did not apply an STS technique when using MIP reformatting, but instead used a single projection of the entire data volume.
By now, both STS MPR and STS MIP reformations are offered by the various manufacturers as “push-button techniques”, thus adding little to no time to the imaging process. Although these reformations should certainly not replace the source images in the viewing process, they may serve as an important adjunct to facilitate data assessment. Until now, however, uncertainty prevailed regarding which reformatting technique should be applied in the diagnostic assessment of MSCT angiographies of the cervicocranial vasculature.
Therefore, in this study we attempted to compare STS MIP and STS MPR prospectively as reformatting methods in a multireader study of the same participant population, focusing both on image quality parameters and the delineation of the various supra-aortic arterial and venous vessels.
Materials and Methods
Participant Demographics and Imaging Protocol
Institutional review board approval was obtained before the commencement of the study, and informed consent was provided.
Ten consecutive patients with complete inclusion criteria and absence of exclusion criteria were included in the study. Of them, 5 were men and 5 were women. The mean age was 65.4 years, and the median age 71.5 years. Because our study design includes an implicit matching within an individual (intraindividual matching), covariate information is a lesser concern.
Inclusion criteria were a given clinical indication for CT angiography of the entire craniocervical vasculature as stated by the referring physician and established by the attending radiologist, and the ability to provide informed consent and to comply with the CT angiographic examination. Exclusion criteria consisted of contraindications to iodinated contrast media, such as a known allergy to iodinated contrast media or elevated renal function tests. Moreover, patients with a complete occlusion of a cervicocranial vessel (eg, complete ICA occlusion) were excluded from the study. The presence or absence of a vascular occlusion was ascertained by the consensus opinion of 2 radiologists who reviewed the datasets of potentially eligible patients before inclusion into the study. These radiologists did not take part as readers in the further course of the study. The presence of mere atherosclerotic disease without vascular occlusion was not viewed as an exclusion criterion.
All participants underwent MSCT angiography of the supra-aortic vasculature with a standardized protocol on a 16-section MSCT (Somatom Sensation 16; Siemens Medical Solutions, Erlangen, Germany). The following acquisition parameters were applied: 200 mAs, 120 kV, collimation of 16 × 0.75 mm with a table feed of 12 mm per rotation, resulting in a pitch factor of 1. By using a power injector at a flow rate of 4 mL/s, 120 mL of a nonionic contrast medium were injected into a cubital vein. Scan time delay was assessed with an automated bolus-tracking method with a monitoring section placed just above the carotid artery bifurcation. None of the patients included in the study had a medical history of cardiac output failure. The direction of acquisition was caudocranial. The volume of acquisition included the entire supra-aortic vasculature from the aortic arch to the vertex. All studies were of good or very good image quality. No study had to be excluded for technical reasons.
Image Evaluation
The acquired datasets were reformatted as both STS MIP and STS MPR in 3 planes with a respective increment of 3 mm. Thus, a total of 60 reformations were created. Image reformations were conducted on a Leonardo workstation, and data analysis was performed at a PACS workstation (MagicView 1000, Siemens Medical Solutions).
Qualitative image scoring was performed independently by 3 staff radiologists with at least 4 years of experience in MSCT angiography of the cervicocranial vasculature and longstanding experience in other neurovascular techniques such as digital subtraction angiography. All readers were blinded with regard to the reformatting technique, and scrubbed datasets were presented on a PACS workstation.
The readers were asked to evaluate the vascular delineation of various arterial and venous vessels, the overall image quality, the subjective perception of the vessel contrast, image artifacts, and the delineation of vessel calcification from the contrast-filled lumen.
The delineation of the respective vessels was rated on a 5-point scale, with 5 corresponding to a vessel or vascular segment with an optimal delineation in its entire length and 1 corresponding to a vessel or vascular segment that cannot be identified at all. The readers were asked to rate each of the following arterial vessels or vascular segments: common carotid arteries (CCAs), bifurcation of the carotid arteries, ICAs, external carotid arteries (ECAs), intraosseous portion of the internal carotid arteries, vertebral arteries, basilar artery, communicating arteries of the circle of Willis, first segments of the anterior, middle, and posterior cerebral arteries (A1, M1, P1), second segments of the anterior, middle, and posterior cerebral arteries (A2, M2, P2), and third segments of the anterior, middle, and posterior cerebral arteries (A3, M3, P3). Moreover, they were asked to rate each of the following venous vessels or vascular segments: internal cerebral veins, cavernous sinus, superior sagittal sinus, transverse and sigmoid sinus, and jugular veins.
All readers were asked to rate the overall image quality for each reformatting technique on a 5-point scale. On this scale, 5 corresponds to an excellent image quality, 4 to a good image quality, 3 to an adequate image quality, 2 to a marginally acceptable image quality, and 1 to an unacceptable image quality. Each reader was also asked to evaluate vessel contrast subjectively on a 5-point scale. On this scale, 5 corresponds to an excellent vessel contrast, 4 to a good vessel contrast, 3 to an adequate vessel contrast, 2 to a marginally acceptable vessel contrast, and 1 to an unacceptably poor vessel contrast. The readers were also asked to assess the impact of image artifacts on a 5-point scale. On this scale, 5 corresponds to a complete absence of imaging artifacts, 4 to mild artifacts not interfering with diagnostic decision making, 3 to moderate artifacts slightly interfering with diagnostic decision making, 2 to pronounced artifacts interfering with diagnostic decision making—though it is still possible to arrive at a diagnosis—and 1 to a situation in which artifacts completely hinder diagnostic decision making. The readers also assessed the impact of dental artifacts on a 5-point scale. On this scale, 5 again corresponds to a complete absence of imaging artifacts, 4 to mild artifacts not interfering with diagnostic decision making, 3 to moderate artifacts slightly interfering with diagnostic decision making, 2 to pronounced artifacts interfering with diagnostic decision making—though again not rendering it impossible to arrive at a diagnosis—and 1 to a situation in which artifacts completely hinder diagnostic decision making. Finally, the readers were also asked to evaluate the delineation of calcifications of the vessel wall from the contrast-filled vessel lumen. On this scale, 5 corresponds to an excellent and confident delineation of vascular calcifications, 4 to a good delineation of vascular calcifications, 3 to an adequate but not fully confident delineation of vascular calcifications, 2 to a poor delineation of vascular calcifications, and 1 to a complete inability to delineate vascular calcifications. The readers were asked to respond with “n/a,” if no calcifications were present.
Statistical Analysis
The paired nature of this design—namely, the MSCT for each subject being reformatted by both MIP and MPR techniques and subsequently each reformation technique being evaluated by each reader—precludes the need to adjust for potential confounders such as age or sex because each subject serves as his or her own control. This also results in reduced variation in response and more precision in detecting a difference in image quality or vascular delineation compared with a design by using 2 independent samples of the same size. The advantages of matched designs are well documented in the statistical literature, and they require special analysis techniques to take advantage of their natural efficiency.
Here we used an extension of the Mantel-Haenzel row mean score test, with stratification on the matched pairs.19 This technique is a generalization of the McNemar test for ordinal data.19,20 For each subject, or matched pair, a 2 × 5 table of reformation technique by score is produced, and the corresponding test statistic is calculated across all tables. This statistic tests for a “location” shift in the distribution of scores between the 2 techniques and adjusts for the matched pairing. The typical null hypothesis is that of no association between row and columns—in other words, the identical distribution of scores for MIP and MPR—versus an alternative hypothesis of a shift in row mean scores between MIP and MPR. Under the null hypothesis, the resulting test statistic is distributed as χ2 with 1 degree of freedom.
The Mantel-Haenzel row mean score test was calculated separately for each parameter and for each reader. We report the test statistic and P value under the null hypothesis, along with the median value and range for each reader parameter combination. All computations were performed by using SAS software (version 8.2; SAS Institute, Cary, NC).
To assess an overall effect for each parameter, the reader-specific test statistics described above were assumed to be independent and were summed. Then, under our null hypothesis, this new test statistic has a χ2 distribution with 3 degrees of freedom and can be used to test for global effect over all readers. Note that, because each reader evaluated the same case set, the reader-specific test statistics are not independent. Their correlation is positive, however, and hence ignoring it results only in a minor loss of efficiency. As a result, conclusions based on this global test statistic will be conservative.
In some instances we discovered that both MIP and MPR were scored identically for each subject by a reader. When this happens, the Mantel-Haenzel row mean score test cannot be computed because the covariance matrix is singular. We then used the McNemar test for 2 × 2 tables wherever possible. If >2 of the 5 possible scores were used for at least one subject, the Mantel-Haenzel row mean score test is technically undefined. However, because both techniques were scored identically for every subject—thus providing absolutely no evidence to reject the null hypothesis of identical distributions—a P value of 1 was reported by convention.
Results
Table 1 summarizes the median values and ranges for each parameter for the 2 different reformatting modalities, whereas Table 2 provides a summary of the Mantel-Haenzel test statistics with P values for each parameter for MIP and MPR reformations.
Table 1:
Median score (range) for every vessel and image quality parameter by reader
| Vessel | Type | Reader 1 | Reader 2 | Reader 3 |
|---|---|---|---|---|
| Arterial score 1: CCA | MIP | 5 (4, 5) | 5 (5, 5) | 4 (3, 5) |
| MPR | 4 (3, 4) | 5 (4, 5) | 4 (3, 5) | |
| Arterial score 2: Bifurcation | MIP | 5 (5, 5) | 5 (4, 5) | 5 (4, 5) |
| MPR | 3 (2, 4) | 4 (3, 4) | 4 (4, 5) | |
| Arterial score 3: ICA | MIP | 4 (4, 5) | 5 (4, 5) | 4 (3, 5) |
| MPR | 3 (2, 4) | 4 (3, 5) | 4 (2, 5) | |
| Arterial score 4: ECA | MIP | 4 (4, 5) | 5 (4, 5) | 4 (3, 5) |
| MPR | 3 (2, 4) | 4 (3, 4) | 4 (2, 5) | |
| Arterial score 5: Intraosseous portion of ICA | MIP | 5 (4, 5) | 5 (4, 5) | 4 (3, 5) |
| MPR | 2 (2, 3) | 3 (3, 4) | 3 (2, 4) | |
| Arterial score 6: Vertebral arteries | MIP | 4 (4, 5) | 5 (4, 5) | 4 (3, 5) |
| MPR | 3 (3, 4) | 4 (3, 4) | 3.5 (2, 5) | |
| Arterial score 7: Basilar artery | MIP | 4 (4, 5) | 5 (5, 5) | 4 (4, 5) |
| MPR | 3 (2, 4) | 4 (4, 4) | 4 (2, 4) | |
| Arterial score 8: Communicating arteries | MIP | 4 (4, 4) | 5 (4, 5) | 4 (3, 5) |
| MPR | 3 (2, 3) | 3.5 (3, 4) | 3 (2, 5) | |
| Arterial score 9: First segments: A1, M1, P1 | MIP | 5 (4, 5) | 5 (5, 5) | 5 (4, 5) |
| MPR | 4 (3, 4) | 4 (4, 5) | 4 (3, 4) | |
| Arterial score 10: Second segments: A2, M2, P2 | MIP | 4.5 (4, 5) | 5 (4, 5) | 4 (3, 4) |
| MPR | 3 (3, 3) | 4 (3, 4) | 3 (2, 3) | |
| Arterial score 11: Third segments: A3, M3, P3 | MIP | 4 (4, 5) | 5 (4, 5) | 3 (3, 4) |
| MPR | 2.5 (2, 3) | 3 (3, 4) | 2 (2, 3) | |
| Venous score 1: Internal and bridging cerebral veins | MIP | 4 (4, 5) | 5 (5, 5) | 4 (3, 5) |
| MPR | 3.5 (3, 4) | 4 (4, 5) | 4 (2, 4) | |
| Venous score 2: Cavernous sinus | MIP | 4 (4, 5) | 4 (4, 5) | 3 (3, 4) |
| MPR | 2 (2, 3) | 4 (3, 4) | 3 (2, 3) | |
| Venous score 3: Superior saggital sinus | MIP | 4 (4, 5) | 5 (5, 5) | 4 (4, 5) |
| MPR | 4 (4, 4) | 5 (3, 5) | 4 (4, 5) | |
| Venous score 4: Transverse and sigmoid sinus | MIP | 4 (4, 5) | 5 (4, 5) | 4 (4, 5) |
| MPR | 4 (4, 5) | 5 (4, 5) | 4 (3, 5) | |
| Venous score 5: Jugular veins | MIP | 3 (2, 5) | 4 (3, 5) | 3 (2, 5) |
| MPR | 3 (2, 4) | 4 (3, 5) | 3 (2, 5) | |
| Quality score 1: Quality overall: 1 (poor) to 5 (excellent) | MIP | 4 (4, 5) | 5 (4, 5) | 4.5 (4, 5) |
| MPR | 3 (3, 4) | 4 (4, 4) | 4 (4, 5) | |
| Quality score 2: Artifacts: 1 (cannot be interpreted) to 5 (no artifacts) | MIP | 4 (3, 5) | 4 (4, 5) | 4 (3, 5) |
| MPR | 3.5 (2, 4) | 4 (4, 5) | 4 (3, 5) | |
| Quality score 3: Dental artifacts: 1 (cannot be interpreted) to 5 (no artifacts) | MIP | 3.5 (2, 5) | 3.5 (3, 5) | 3.5 (2, 5) |
| MPR | 3.5 (2, 5) | 3.5 (2, 5) | 3.5 (2, 5) | |
| Quality score 4: Delineation of vascular calcification: 1 (poor) to 5 (excellent) | MIP | 5 (4, 5)† | 5 (4, 5)† | 5 (4, 5)† |
| MPR | 3 (2, 3)† | 4 (3, 4)† | 5 (3, 5)† | |
| Quality score 5: Subjective contrast: 1 (insufficient) to 5 (excellent) | MIP | 5 (4, 5) | 5 (5, 5) | 4.5 (4, 5) |
| MPR | 5 (4, 5) | 4 (4, 5) | 4.5 (4, 5) |
Note:—CCA indicates common carotid artery; ICA, internal carotid artery; ECA, external carotid artery.
In one of the 10 subjects, all readers chose n/a, as no calcifications were discerned with either technique.
Table 2:
Mantel-Haenzel row mean score test statistic (P value) based on a χ2 distribution with 1 degree of freedom (3 degrees of freedom for the overall analysis), stratified on matched pairs, for every vessel and image quality parameter by reader
| Vessel | Reader 1 | Reader 2 | Reader 3 | Overall |
|---|---|---|---|---|
| Arterial score 1: CCA | 9.3077 (0.0023) | 4.0000 (0.0455) | 2.0000 (0.1573) | 15.3077 (0.0016) |
| Arterial score 2: Bifurcation | 9.0000 (0.0027) | 8.3333 (0.0039) | 5.0000 (0.0253) | 22.3333 (<0.0001) |
| Arterial score 3: ICA | 8.8947 (0.0029) | 8.0000 (0.0047) | 4.0000 (0.0455) | 20.8947 (0.0001) |
| Arterial score 4: ECA | 8.8947 (0.0029) | 9.0000 (0.0027) | 4.0000 (0.0455) | 21.8947 (<0.0001) |
| Arterial score 5: Intraosseous portion of ICA | 9.2807 (0.0023) | 8.8947 (0.0029) | 5.0000 (0.0253) | 23.1754 (<0.0001) |
| Arterial score 6: Vertebral arteries | 6.4000 (0.0114) | 8.3333 (0.0039) | 7.0000 (0.0082) | 21.7333 (<0.0001) |
| Arterial score 7: Basilar artery | 8.9091 (0.0028) | 10.000 (0.0016) | 6.2308 (0.0126) | 25.1399 (<0.0001) |
| Arterial score 8: Communicating arteries | 8.8947 (0.0029) | 8.8947 (0.0029) | 6.2308 (0.0126) | 24.0202 (<0.0001) |
| Arterial score 9: First segments: A1, M1, P1 | 8.3333 (0.0039) | 6.0000 (0.0143) | 9.0000 (0.0027) | 23.3333 (<0.0001) |
| Arterial score 10: Second segments: A2, M2, P2 | 9.0000 (0.0027) | 8.3333 (0.0039) | 9.3077 (0.0023) | 26.3333 (<0.0001) |
| Arterial score 11: Third segments: A3, M3, P3 | 9.3226 (0.0023) | 9.1429 (0.0025) | 10.000 (0.0016) | 28.4655 (<0.0001) |
| Venous score 1: Internal and bridging cerebral veins | 5.4000 (0.0201) | 7.0000 (0.0082) | 4.4545 (0.0348) | 16.8545 (0.0008) |
| Venous score 2: Cavernous sinus | 9.0000 (0.0027) | 4.0000 (0.0455) | 6.0000 (0.0143) | 19.0000 (0.0003) |
| Venous score 3: Superior saggital sinus | 2.0000 (0.1573) | 1.0000 (0.3173) | 0 (1)‡ | 3.0000 (0.3916) |
| Venous score 4: Transverse and sigmoid sinus | 1.0000 (0.3173) | 1.0000 (0.3173) | 1.0000 (0.3173) | 3.0000 (0.3916) |
| Venous score 5: Jugular veins | 1.0000 (0.3173) | 1.0000 (0.3173) | 0 (1)††† | 2.0000 (0.5724) |
| Quality score 1: Quality overall: 1 (poor) to 5 (excellent) | 7.3636 (0.0067) | 9.0000 (0.0027) | 1.0000 (0.3173) | 17.3636 (0.0006) |
| Quality score 2: Artifacts: 1 (cannot be interpreted) to 5 (no artifacts) | 4.0000 (0.0455) | 1.0000 (0.3173) | 0 (1)††† | 5.0000 (0.1718) |
| Quality score 3: Dental artifacts: 1 (cannot be interpreted) to 5 (no artifacts) | 1.0000 (0.3173) | 1.0000 (0.3173) | 0 (1)††† | 2.0000 (0.5724) |
| Quality score 4: Delineation of vascular calcification: 1 (poor) to 5 (excellent) | 9.000 (0.0027)† | 7.118 (0.0076)† | 4.000 (0.0455)† | 20.1176 (0.0002)† |
| Quality score 5: Subjective contrast: 1 (insufficient) to 5 (excellent) | 0 (1)‡ | 6.0000 (0.0143) | 0 (1)‡ | 6.0000 (0.1116) |
Note:—In every instance where the test was significant, the shift in row mean scores was due to a higher distribution of scores for MIP. Significant results are marked in bold. CCA indicates common carotid artery; ICA, internal carotid artery; ECA, external carotid artery.
In one of the 10 subjects, all readers chose n/a, as no calcifications were discerned with either technique.
Only 2 of the possible 5 scores were used for every subject, for both MIP and MPR. The resulting 2 × 2 table has identical MIP and MPR scores within every subject. Thus, the Mantel-Haenzel row mean score test, stratified on matched pairs, cannot be computed due to a singular covariance matrix. However, in this situation, McNemar’s test for 2 × 2 tables can be used. Here, McNemar’s test statistic is 0 with a P value of 1.
MIP and MPR scores are identical within every subject, and thus the Mantel-Haenzel row mean score test, stratified on matched pairs, cannot be computed due to a singular covariance matrix.
In terms of image quality parameters, STS MIP reformations were significantly superior to STS MPR for both overall image quality (P < .01 for readers 1 and 2) and the delineation of vascular calcifications from the contrast-filled lumen (P < .05 for all readers). In the overall analysis, these differences in favor of STS MIP were significant for both parameters with P < .001.
Differences were not significant for most readers and for the overall assessment regarding the impact of artifacts in general and regarding the impact of dental artifacts. Differences were also not significant for the visual assessment of vessel contrast.
With regard to the delineation of vessels or vascular segments, the STS MIP reformations were significantly superior (P < .05) for almost all arterial vessels and vascular segments for almost all readers, with the exception of the common carotid artery for reader 3. In the overall analysis, differences in favor of STS MIP were significant for all arteries and arterial segments with a P < .005. This superiority of STS MIP versus STS MPR was demonstrated both for the extracranial and for the intracranial arteries and arterial segments.
With respect to the delineation of veins, MIP reformations were significantly superior to MPR for the cavernous sinus and for the bridging and internal cerebral veins for all readers (P < .05 for the respective readers, and P < .001 for the overall analysis). Differences between MIP and MPR were not significant for the superior sagittal sinus, the transverse and sigmoid sinus, and the jugular veins, for any of the readers and for the overall analysis (P > .05).
In the assessment of the superior sagittal sinus, one reader (reader 3) only used 2 of the possible 5 scores for every participant both for MIP and for MPR. The same happened in the evaluation of the visual assessment of the vascular contrast for readers 1 and 3. The resulting 2 × 2 table demonstrated identical MIP and MPR scores within every subject. The stratified Mantel-Haenzel row mean score test could not be computed in this setting, because of a singular covariance matrix. The McNemar test for 2 × 2 table demonstrated a test statistic of 0 with a P value of 1.
Reader 3 also gave identical scores within every subject for MIP and MPR reformations for the assessment of the jugular veins and also for the evaluation of artifacts and dental artifacts. Again, the Mantel-Haenzel row mean score test, stratified on matched pairs, could not be computed in this setting, because of a singular covariance matrix. Because all scores are identical within every subject, it is evident, however, that there are no differences between the groups for these parameters.
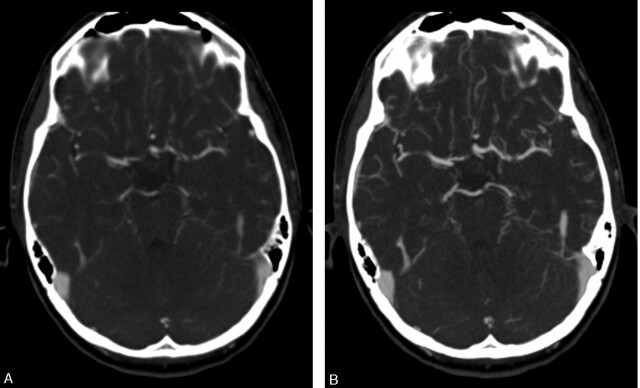
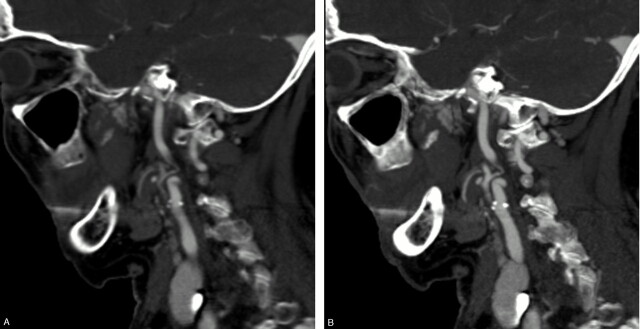
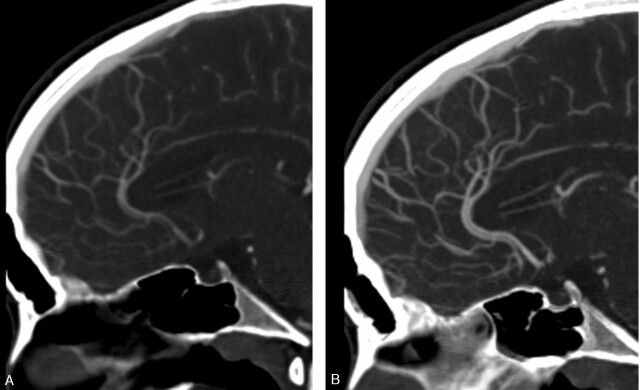
Figures 1–3 demonstrate corresponding axial and sagittal sections of STS MPR and STS MIP reformations in a 63-year-old man. Both extracranial and intracranial arteries are better delineated with the MIP technique, whereas most veins are equally well delineated with MPR and MIP reformations.
Fig 1.
Corresponding axial sections of STS MPR (A) and MIP (B) reformations in a 63-year-old man. The small intracranial arteries are better delineated with the MIP reformatting technique. Window and level settings were standardized and are the same in both panels.
Fig 3.
Corresponding sagittal of STS MPR (A) and MIP (B) reformations in a 78-year-old woman. The calcifications of the carotid bifurcation are better delineated in the MIP reformations. Window and level settings were standardized and are the same in both panels.
Discussion
In the past, controversial data have been published regarding the relative value of various reformatting techniques. Most of these studies focused on the quantitative evaluation of the degree of vascular stenoses and compared either MIP or MPR to volume-rendering techniques. Several studies demonstrated a superiority of volume-rendering techniques over either MPR or MIP,13,18,21 whereas others found MIP to be more reliable than volume-rendering techniques.14,16 One study reported MPR to be superior to MIP in the quantitative evaluation of renal artery stenoses,10 whereas others propagated a combination of both MIP and MPR in this setting.11,12 All of these studies were performed on single-section scanners, however, and most did not employ a STS technique for the MIP reformations.
Two more recent studies compared the use of STS MIP with STS MPR for the evaluation of chest CT on a 4-section MSCT and found a superiority of MIP over MPR in the delineation of the pulmonary arteries and in the detection of pulmonary nodules, whereas MPR was found to be superior in the delineation of the lung parenchyma and of central and peripheral bronchi.22,23 These results suggest that MIP in a STS technique may be superior to MPR as a primary reformatting technique in vascular imaging of the cervicocranial vasculature as well. Nevertheless, CT angiographies of the supra-aortic vessels pose different challenges from vascular imaging in other organ systems, because both intra- and extracranial vessels with a variety of luminal diameters need to be delineated and as the close proximity of complex osseous structures, such as the skull base, frequently impedes the vascular demarcation.
In our study, we chose to apply STS techniques, because these techniques tend to preserve a maximum of information while allowing the reader to view the dataset in multiple planes. The general impression of cross-sectional imaging remains preserved.8,9 In addition, the MPR technique inherently requires the application of a thin-slab technique, because the viewing of the dataset in just one large slab would literally eliminate the information contained in the dataset. MIP reformations, on the other hand, can be viewed as single slab projections, a technique well known from MR angiography.8,9 In CT angiography, however, this technique is severely hindered by the presence of the surrounding, highly attenuating skull.
In our study, we have demonstrated a superiority of STS MIP reformations over STS MPR for both extracranial and intracranial arteries, as well as for the cavernous sinus and the internal and bridging cerebral veins. There were no significant differences between STS MIP and STS MPR for the large venous vessels, such as the superior sagittal sinus, the transverse and sigmoid sinus, and the jugular veins. Regarding image quality parameters, MIP was shown to be superior to MPR in the overall image quality and in the delineation of vascular calcifications from the vessel lumen, though no differences were found for the severity of artifacts and for the visual assessment of the vascular contrast. Although MIP was demonstrated to be superior to MPR in most aspects, no significant differences were found in the remaining parameters. In no instance was a superiority of MPR over MIP found.
One of the potential reasons why MIP was preferred over MPR is the generally higher vessel-to-background contrast, because MIP reformations project only the pixel with the highest attenuation, whereas MPR averages the attenuation of the pixels along the axis of projection.8,9 Moreover, the vessels—representing highly attenuating structures in CT angiography—tend to appear more plastic and small vessels can be delineated and followed more easily.22,23
Our study has several limitations, which need to be taken into account when interpreting the data. First, we did not compare MIP or MPR with the various forms of 3D volume-rendering techniques. We aimed to compare reformatting techniques employing STSs, however, because these preserve a multitude of information, are rapidly performed, and are well suited for the primary diagnostic evaluation of the data. We did not intend to compare these techniques with the various volume-rendering techniques, because the latter are usually applied in a later stage of the diagnostic assessment of the data and are usually performed for selected indications only.
Second, our study population was relatively small. Nevertheless, we were able to use a matched-pair analysis, because both reformatting techniques were performed in every subject. This design has considerable efficiency and allows us to control for probable confounders automatically. This precludes the need to adjust the analysis for participant covariate makeup.
Third, our study design did not include a gold standard. We instead performed a qualitative comparison of 2 different reformatting techniques with special attention to the various vascular segments rendering the conception of a gold standard virtually impossible. Fourth, we purposely performed our evaluation in a general patient population and not in patients with one specific disease entity. Our aim was to evaluate the relative value of the 2 reformatting techniques with regard to image quality parameters and to the delineation of both intra- and extracranial arteries and veins. We did not aim to assess the relative value of the reformations for specific disease entities, but instead wanted to gain insight into the reformation techniques as general diagnostic tools in MSCT angiography of the cervicocranial vasculature. In the daily clinical routine, the diagnosis is often not known before the CTA, leaving the radiologist with a variety of potential differential diagnoses and sites of pathology and with a large volume of MSCT angiographic data. We therefore intended to evaluate which STS reformatting technique was superior independent of a specific disease category. Nevertheless, some disease categories may have specific requirements. The evaluation of carotid artery stenoses for example may profit from volume-rendering techniques or axial source images,17,18 just as the detection and evaluation of intracranial aneurysms may be augmented by volume-rendering techniques.21,24 To gain insight into the relative value of various reformatting techniques in such specific disease entities, focused studies with selected participant populations will need to be performed. It would not be feasible to incorporate all different disease categories into a single study design.
Conclusion
In conclusion, we have demonstrated a preference for STS MIP reformations compared with STS MPR for both extracranial and intracranial arteries, for the cavernous sinus and the internal cerebral veins, as well as for overall image quality and delineation of vascular calcifications. For all other parameters, we found no significant differences. MPR reformations, however, were not preferred to MIP reformations in any of the aspects we evaluated. We therefore recommend STS MIP as the primary reformation of choice in MSCT angiography of the cervicocranial vessels in addition to the viewing of source images. Volume-rendered images can play an important complementary role in the viewing process, especially after a provisional impression is gained on the STS images.
Fig 2.
Corresponding sagittal sections of STS MPR (A) and MIP (B) reformations in the same 63-year-old man. The intracranial arteries and small veins are better delineated with the MIP reformatting technique, whereas the superior sagittal sinus is about equally delineated. Window and level settings were standardized and are the same in both panels.
References
- 1.Rubin GD, Shiau MC, Schmidt AJ, et al. Computed tomographic angiography: historical perspective and new state-of-the-art using multi detector-row helical computed tomography. J Comput Assist Tomogr 1999;23(suppl 1):S83–90 [PubMed] [Google Scholar]
- 2.Rankin SC. Spiral CT: vascular applications. Eur J Radiol 1998;28:18–29 [DOI] [PubMed] [Google Scholar]
- 3.Fuchs T, Kachelriess M, Kalender WA. Technical advances in multi-slice spiral CT. Eur J Radiol 2000;36:69–73 [DOI] [PubMed] [Google Scholar]
- 4.Tampieri D, Leblanc R, Oleszek J, et al. Three-dimensional computed tomographic angiography of cerebral aneurysms. Neurosurgery 1995;36:749–54;discussion 754–45 [DOI] [PubMed] [Google Scholar]
- 5.Preda L, Gaetani P, Rodriguez y Baena R, et al. Spiral CT angiography and surgical correlations in the evaluation of intracranial aneurysms. Eur Radiol 1998;8:739–45 [DOI] [PubMed] [Google Scholar]
- 6.Villablanca JP, Martin N, Jahan R, et al. Volume-rendered helical computerized tomography angiography in the detection and characterization of intracranial aneurysms. J Neurosurg 2000;93:254–64 [DOI] [PubMed] [Google Scholar]
- 7.Villablanca JP, Hooshi P, Martin N, et al. Three-dimensional helical computerized tomography angiography in the diagnosis, characterization, and management of middle cerebral artery aneurysms: comparison with conventional angiography and intraoperative findings. J Neurosurg 2002;97:1322–32 [DOI] [PubMed] [Google Scholar]
- 8.Cody DD. AAPM/RSNA physics tutorial for residents: topics in CT: image processing in CT. Radiographics 2002;22:1255–68 [DOI] [PubMed] [Google Scholar]
- 9.Napel S, Rubin GD, Jeffrey RB Jr. STS-MIP: a new reconstruction technique for CT of the chest. J Comput Assist Tomogr 1993;17:832–38 [PubMed] [Google Scholar]
- 10.Galanski M, Prokop M, Chavan A, et al. Renal arterial stenoses: spiral CT angiography. Radiology 1993;189:185–92 [DOI] [PubMed] [Google Scholar]
- 11.Brink JA, Lim JT, Wang G, et al. Technical optimization of spiral CT for depiction of renal artery stenosis: in vitro analysis. Radiology 1995;194:157–63 [DOI] [PubMed] [Google Scholar]
- 12.Berg MH, Manninen HI, Vanninen RL, et al. Assessment of renal artery stenosis with CT angiography: usefulness of multiplanar reformation, quantitative stenosis measurements, and densitometric analysis of renal parenchymal enhancement as adjuncts to MIP film reading. J Comput Assist Tomogr 1998;22:533–40 [DOI] [PubMed] [Google Scholar]
- 13.Davros WJ, Obuchowski NA, Berman PM, et al. A phantom study: evaluation of renal artery stenosis using helical CT and 3D reconstructions. J Comput Assist Tomogr 1997;21:156–61 [DOI] [PubMed] [Google Scholar]
- 14.Rubin GD, Dake MD, Napel S, et al. Spiral CT of renal artery stenosis: comparison of three-dimensional rendering techniques. Radiology 1994;190:181–89 [DOI] [PubMed] [Google Scholar]
- 15.Castillo M, Wilson JD. CT angiography of the common carotid artery bifurcation: comparison between two techniques and conventional angiography. Neuroradiology 1994;36:602–604 [DOI] [PubMed] [Google Scholar]
- 16.Leclerc X, Godefroy O, Pruvo JP, et al. Computed tomographic angiography for the evaluation of carotid artery stenosis. Stroke 1995;26:1577–81 [DOI] [PubMed] [Google Scholar]
- 17.Dix JE, Evans AJ, Kallmes DF, et al. Accuracy and precision of CT angiography in a model of carotid artery bifurcation stenosis. AJNR Am J Neuroradiol 1997;18:409–15 [PMC free article] [PubMed] [Google Scholar]
- 18.Addis KA, Hopper KD, Iyriboz TA, et al. CT angiography: in vitro comparison of five reconstruction methods. AJR Am J Roentgenol 2001;177:1171–76 [DOI] [PubMed] [Google Scholar]
- 19.Stokes E, Davis C, Koch G. Categorical data analysis using the SAS system. Cary, NC: SAS Institute;2000
- 20.Mantel N. Chi-square tests with one degree of freedom: extensions of the Mantel-Haenzel procedure. J Am Statistical Assoc 1963;58:690–700 [Google Scholar]
- 21.Kallmes DF, Evans AJ, Woodcock RJ, et al. Optimization of parameters for the detection of cerebral aneurysms: CT angiography of a model. Radiology 1996;200:403–405 [DOI] [PubMed] [Google Scholar]
- 22.Eibel R, Bruning R, Schopf UJ, et al. [Image analysis in multislice spiral CT of the lung with MPR and MIP reconstructions]. Radiologe 1999;39:952–57 [DOI] [PubMed] [Google Scholar]
- 23.Eibel R, Turk TR, Kulinna C, et al. [Multidetector-row CT of the lungs: multiplanar reconstructions and maximum intensity projections for the detection of pulmonary nodules]. Rofo Fortschr Geb Rontgenstr Neuen Bildgeb Verfahr 2001;173:815–21 [DOI] [PubMed] [Google Scholar]
- 24.Kato Y, Nair S, Sano H, et al. Multi-slice 3D-CTA: an improvement over single slice helical CTA for cerebral aneurysms. Acta Neurochir (Wien) 2002;144:715–22 [DOI] [PubMed] [Google Scholar]