Abstract
SUMMARY: Plexiform neurofibroma of the submandibular gland is an extremely rare tumor. We report the CT findings in a 6-year-old girl with type 1 neurofibromatosis who had a histopathologically proven submandibular gland plexiform neurofibroma. A “branching” hypodense mass was noted on the CT scan infiltrating the submandibular gland and the adjacent spaces of the neck. CT could be extremely valuable in suggesting the diagnosis.
Plexiform neurofibromas are locally infiltrative, slow-growing tumors. They are uncommon tumors of the salivary glands and most often have been described in the parotid gland. Reports of plexiform neurofibromas of the submandibular gland have been rare.1–4 We present the CT findings of submandibular plexiform neurofibroma in a patient and review the features in the 4 prior reported cases, in only 2 of which CT findings were described.
Case Report
A 6-year-old girl with type 1 neurofibromatosis was evaluated for abnormality in the right floor of the mouth that was detected during a routine dental examination 4 months before presentation. There was no family history of neurofibromatosis. The patient had 8–9 café-au-lait spots of ≥5 mm on her legs, buttock, and torso. A small neurofibroma was also noted on the dorsum of the right hand. An MR imaging of the brain in the previous year showed small rounded lesions in the bilateral basal ganglia, right cerebellar white matter, and left medulla/inferior cerebellar peduncle, consistent with hamartomatous/vacuolar lesions seen with type 1 neurofibromatosis. Examination of the oral cavity revealed vague fullness involving the right floor of the mouth. The oral mucosa was healthy. The right submandibular gland was somewhat larger than the left and was not tender. The patient had no history of recurrent swelling or pain in the submandibular region. There were no pathologic lymph nodes within the neck. Otherwise, the child seemed healthy.
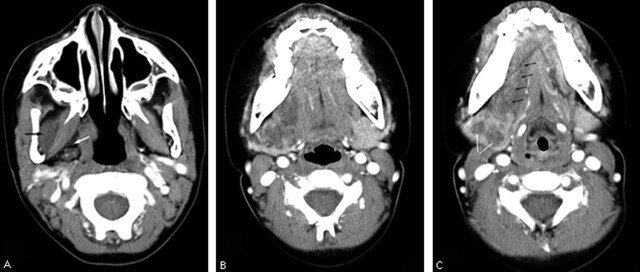
A contrast-enhanced CT scan of the neck (Fig 1) showed enlargement of the right submandibular gland measuring 2.7 × 2.3 cm, with well-defined margins, an enhancing periphery similar to that of the normal left submandibular gland, and a central hypoattenuated core. The central core was somewhat lobulated and had a “branching” appearance, the stem of which was extending into the adjacent soft tissues. Hypoattenuated tubular masses were seen extending into the right sublingual space as well as the right masticator space and the right parapharyngeal space. The branching pattern was more readily appreciated on scrolling through the images on a monitor. Prominent lymph nodes were seen in bilateral deep cervical and posterior cervical group in the upper neck, which were felt to be reactive. A 1.2-cm hypoattenuated nodular mass was also noted in the superior mediastinum near the suprasternal notch, which was suspicious for a nerve sheath tumor or an enlarged lymph node. A CT-guided fine needle aspiration cytology of the right submandibular mass proved to be nondiagnostic. Because it was not possible to exclude the possibility of an infiltrative primary submandibular tumor, surgical resection of the mass was planned.
Fig 1.
Sequential images from axial contrast-enhanced CT scan demonstrating the plexiform neurofibroma of the right submandibular gland.
A–C, Tubular hypoattenuated masses are seen in the right masticator space (A, black arrow), parapharyngeal space (A, white arrow) and in the right submandibular space surrounding the submandibular gland. The right submandibular gland is enlarged and has peripheral enhancing parenchyma similar to that of the normal left submandibular gland (B, C). There is a central branching hypoattenuated mass (C, white arrows), which is the infiltrating plexiform neurofibroma. Note the extension of the plexiform neurofibroma into the right sublingual space along the course of the lingual nerve (C, black arrows).
At surgery there appeared to be a tumor with vegetations on the superior aspect of the submandibular gland infiltrating into the gland itself. With further dissection of fascial planes superiorly, it was evident that the tumor was following the course of the lingual nerve. A small portion of the tumor was biopsied and sent for frozen section, which was consistent with a neurofibroma. The tumor mass was completely dissected from the operative field. Several small remnants were then dissected from the lingual nerve. The lingual nerve was preserved. During the dissection, the hypoglossal nerve was identified and preserved and there was no evidence of involvement of the hypoglossal nerve.
Histopathologic examination of the resected submandibular mass revealed a myxoid background containing loosely arranged sinusoidal-shaped spindle cells and scattered mast cells. Superimposed upon this diffuse infiltrate of neuroid spindle cells were denser encapsulated proliferations of similar cells. These features were typical of plexiform neurofibromas.
The patient recovered well in the postoperative period. A follow-up CT scan of the neck 4 months after surgery showed postoperative changes in the right submandibular region and stable appearance of the lesions in the right masticator, sublingual, parapharyngeal spaces and in the superior mediastinum. An examination of the patient 8 months after surgery revealed decrease in the fullness in the floor of the mouth and good healing of the incision. The patient was otherwise asymptomatic and routine follow-up was advised.
Discussion
Plexiform neurofibromas demonstrate diffuse cylindrical enlargement of multiple fascicles of a nerve including the nerve branches leading to a diffuse mass of thickened nerves.5 These tumors may be superficial or deep and have an appearance of growth along the course of the nerves, extending into adjacent tissues. They are locally infiltrative benign tumors that tend to grow slowly. Although they may grow any time, growth spurts are particularly seen in early childhood and during puberty or pregnancy. Histologically they consist of Schwann cells, nerve fibers, mast cells, and perineurial and endoneurial fibroblasts in a myxoid matrix. Plexiform neurofibromas are frequently seen in patients with type 1 neurofibromatosis, with most being asymptomatic. In one CT study in adults with type 1 neurofibromatosis they were found in the chest in 20% and in the abdomen and pelvis in 40%.6
Neurofibromas are rarely seen in the salivary glands and have been reported mostly in the parotid glands. Seifert et al7 found neurofibromas to account for only 0.4% of salivary gland tumors. Plexiform neurofibromas of the salivary glands are even more rare. Castro et al8 found in a review only 2 plexiform neurofibromas among 300 cases of major salivary gland tumors in children. They are exceedingly rare in the submandibular glands and sublingual glands.1–4,9 A Medline search of literature revealed only 4 cases of submandibular plexiform neurofibromas, and CT findings were described in only 2.1–4
Bourgeois et al1 reported a case of submandibular plexiform neurofibroma in a 3-year-old boy with a history of neurofibromatosis type 1. The mass had grown rapidly over the preceding 6–12 months. It had been present since infancy. A CT scan demonstrated a well-defined mass with low attenuation and some internal apparent stranding. Fine-needle aspiration cytology (FNAC) showed spindle cells, which was suggestive but not diagnostic of neurofibroma. Surgical excision revealed findings typical of a plexiform neurofibroma with normal-appearing hypoglossal and laryngeal nerves.
Tsutsumi et al2 reported a 29-year-old woman with repeated swelling of submandibular gland for 10 years who was found to have a plexiform neurofibroma. The patient did not have a family history of neurofibromatosis and did not demonstrate evidence of neurofibromatosis. A CT scan demonstrated an enlarged submandibular gland surrounding a low-attenuation area. There was no significant enhancement. FNAC was nondiagnostic. Histopathologic examination revealed a characteristic plexiform neurofibroma permeating the entire gland. The origin of this tumor was not obvious at surgery, though the hypoglossal and lingual nerves were clinically intact. The tumor was thought to have originated from the secreting nerve.
Derekoy et al reported a case of plexiform neurofibroma of the submandibular gland in a 20-year-old man with signs of Von Recklinghausen disease.3 The patient also had macroglossia (regional gigantism). No imaging findings were described in this patient but on pathologic examination the submandibular gland was found to be indented and infiltrated by the lesion.
Weitzner reported 2 cases of salivary gland plexiform neurofibromas4: sublingual gland plexiform neurofibroma in a 17-month-old boy and parotid and submandibular gland plexiform neurofibromas in a 3-year-old girl. Both patients had other manifestations of type 1 neurofibromatosis. Imaging findings have not been reported in these patients.
The 2 patients in whom CT findings were described1,2 had central soft tissue hypoattenuation within the submandibular gland mass with “interconnecting strands of hyperattenuation” described in one of them.1 A detailed description of the CT imaging findings is not given in these case reports but a review of the published images revealed well-defined margins of the submandibular gland mass in both the patients. Similar to the findings in our patient, the periphery of the submandibular mass showed enhancement akin to that of the normal submandibular gland, which possibly represents the parenchyma of the submandibular gland that has been expanded by a central infiltrating core of plexiform neurofibroma. In both of these patients, there has been no CT description of soft tissue masses in the adjacent spaces of the neck, but in one of them1 a firm tubular mass was described at the edge of the surgical specimen that proved to be a neurovascular bundle that was also involved with plexiform neurofibroma. These findings in conjunction with those described in our patient (Fig 1) hint at the possibility of plexiform neurofibroma of the submandibular gland arising as a consequence of infiltration of the tumor along the nerves as a central core into the substance of the submandibular gland.
The diagnostic yield of FNAC appears to be rather low. A plexiform neurofibroma may be suspected in the appropriate clinical setting, with the help of cross-sectional imaging. CT and MR imaging of plexiform neurofibroma may show conglomerate multilobulated masses that may at times appear as a “bag of worms.” On CT they appear hypoattenuated, whereas on T1-weighted MR images they are isointense to hypointense when compared with muscle signal intensity. These masses may show a “target sign” on T2-weighted images with peripheral hyperintense signal intensity and central isointense to hypointense signal intensity. Contrast enhancement may be heterogeneous.10 To date, there have been no reports of MR imaging features of plexiform neurofibroma of the submandibular gland.
A stable plexiform neurofibroma may be observed closely for any change in size. If the mass is growing or causing cosmetic disfigurement, excision of the tumor, as much as is possible, is the treatment of choice. Recurrence is seen in as many as 20% of the patients with a plexiform neurofibroma after complete resection and increases to 44% with subtotal resection.11 Younger children, whose tumors of the head/neck/face, and who have tumors that cannot be completely removed, are at particular risk for recurrence. The natural history of plexiform neurofibromas has not been determined, but malignant peripheral nerve sheath tumors are reported to occur in 2%–5% of patients with type 1 neurofibromatosis, with a lifetime risk approaching 10%. Most of these arise in pre-existing plexiform neurofibromas.12 Plexiform neurofibromas that are more deeply located and are more extensive appear to have a greater chance of malignancy. Compression of adjacent critical structures such as the airway and extension into the spinal canal is of particular concern in plexiform neurofibromas of the head and neck.
In conclusion, submandibular gland plexiform neurofibroma is an extremely rare tumor. The diagnosis, however, may be entertained in a patient with type 1 neurofibromatosis presenting with a slow-growing submandibular region mass. Four of the 5 reported patients, including our patient, had type 1 neurofibromatosis. It appears to be a childhood mass with 3 of 5 occurring in patients younger than 6 years of age. The mass appears hypoattenuated and less enhancing when compared with the submandibular gland. A characteristic “branching” hypoattenuated mass on CT scan that appears to be infiltrating the submandibular gland associated with branching tubular masses in the adjacent tissues in the neck could be virtually diagnostic in this clinical setting. The “branching pattern” may be more easily appreciated on scrolling through the images on a computer monitor. CT imaging features could be extremely helpful to the clinician in appropriately advising the patients, planning surgery, and for follow-up.
References
- 1.Bourgeois JM, Radhi J, Elden L, et al. Plexiform neurofibroma of the submandibular salivary gland in a child. Can J Gastroenterol 2001;15:835–37 [DOI] [PubMed] [Google Scholar]
- 2.Tsutsumi T, Oku T, Komatsuzaki A. Solitary plexiform neurofibroma of the submandibular salivary gland. J Laryngol Otol 1996;110:1173–75 [DOI] [PubMed] [Google Scholar]
- 3.Derekoy S, Sefali M. Plexiform neurofibroma of the submandibular gland. J Laryngol Otol 2000;114:643–45 [DOI] [PubMed] [Google Scholar]
- 4.Weitzner S. Plexiform neurofibroma of major salivary glands in children. Oral Surg Oral Med Oral Pathol 1980;50:53–57 [DOI] [PubMed] [Google Scholar]
- 5.Korf B. Plexiform neurofibromas. Am J Med Genet 1999;89:31–37 [DOI] [PubMed] [Google Scholar]
- 6.Tonsgard JH, Short MP, Kwak S, et al. Computed tomographic imaging in neurofibromatosis. Neurology 1998;50:1755–60 [DOI] [PubMed] [Google Scholar]
- 7.Seifert, G., Miehlke, A., Haubrich, J, et al. Pathology, diagnosis, treatment, facial nerve surgery. Stuttgart: Georg Thieme Verlag;1986;171–301
- 8.Castro EB, Huvos AG, Strong EW, et al. Tumors of the major salivary glands in children. Cancer 1972;29:312–17 [DOI] [PubMed] [Google Scholar]
- 9.Kahwaji G, Hamdan AL, Mufarij A, et al. Plexiform neurofibroma of the sublingual gland. Otolaryngol Head Neck Surg 2000;122:927. [DOI] [PubMed] [Google Scholar]
- 10.Lin J, Martel W. Cross-sectional imaging of peripheral nerve sheath tumors: characteristic signs on CT, MR imaging, and sonography. AJR Am J Roentgenol 2001;176:75–82 [DOI] [PubMed] [Google Scholar]
- 11.Needle MN, Cnaan A, Dattilo J, et al. Prognostic signs in the surgical management of plexiform neurofibroma: the Children’s Hospital of Philadelphia experience, 1974–1994. J Pediat 1997;131:678–82 [DOI] [PubMed] [Google Scholar]
- 12.Ferner, Rosalie E, Gutmann, David H. International consensus statement on malignant peripheral nerve sheath tumors in neurofibromatosis 1. Cancer Res 2002;62:1573–77 [PubMed] [Google Scholar]