Abstract
BACKGROUND AND PURPOSE: An earlier retrospective study indicated that the neck size of elastase-induced aneurysms could be controlled by adjusting the position of the inflated balloon. We report the current prospective study to confirm our previous work.
METHODS: Ninety elastase-induced aneurysms were created in rabbits. Group 1 (n = 62) included cases in which the occlusion balloon resided low, completely within the brachiocephalic/subclavian arteries. Group 2 (n = 28) included cases in which the balloon resided high, within both the common carotid artery and brachiocephalic/subclavian arteries. Follow-up digital subtraction angiography was performed. The aneurysm sizes were measured and compared between groups. The Student t test and the Fisher exact test were used for statistical analysis.
RESULTS: The mean aneurysm neck diameter and width for group 1 was significantly larger than that of group 2 (3.4 ± 1.2 and 2.3 ± 0.9 mm, P < .001; 3.8 ± 1.0 and 3.3 ± 0.9 mm, P < .05, respectively). The proportion of wide-necked aneurysms in group 1 was significantly larger than that in group 2 (29% vs 4%; P < .005). Mean dome-to-neck ratios were 1.2 ± 0.4 and 1.7 ± 0.7 for groups 1 and 2 (P < .005). There was no significant difference in aneurysm height between groups 1 and 2 (8.0 ± 1.7 and 7.5 ± 2.2 mm; P > .05).
CONCLUSION: The neck size of elastase-induced aneurysm models in rabbits can be controlled by adjusting the position of the inflated balloon.
Among the different animal aneurysm models reported (1–7), the elastase-induced aneurysm model in rabbits has been validated by a series of investigations (7–10). This model has been successfully used for testing various endovascular devices (11–16). One potential disadvantage of the elastase-induced aneurysm model is apparent lack of control of neck size, which has relevance for testing of devices aimed at either narrow- or wide-necked aneurysms. Creation of elastase-induced aneurysms involves isolation of the common carotid artery (CCA) lumen by distal ligation and temporary, proximal balloon occlusion. Elastase is then incubated above the occlusion balloon. In this study, we report that the neck size of the aneurysm model can be controlled by adjusting the position of the inflated balloon during elastase incubation.
Methods
Aneurysm Creation
Elastase-induced, saccular aneurysms were created in 90 New Zealand white rabbits. All procedures were approved by the institutional animal care and use committee at our institution. Detailed procedures for aneurysm creation have been described elsewhere (2, 7). In brief, New Zealand white rabbits (3–4 kg) were anesthetized with intramuscular injection of ketamine, xylazine, and acepromazine (75, 5, and 1 mg/kg, respectively). By using a sterile technique, the right common carotid artery (RCCA) was exposed and ligated distally. A 5F sheath (Cordis Endovascular, Miami Lakes, FL) was advanced retrograde in the RCCA to a point approximately 3 cm cephalad to the origin of RCCA. A roadmap image was obtained by injection of contrast through the sheath retrograde in the RCCA, to identify the junction between the RCCA and the subclavian and brachiocephalic arteries (Advantx; General Electric Company, Milwaukee, WI). Through the indwelling sheath, a 3F Fogarty balloon (Baxter Healthcare Corporation, Irvine, CA) was advanced to the origin of the RCCA at its junction with the right subclavian artery. The entire balloon was inserted into the subclavian and brachiocephalic arteries in 62 rabbits (group 1); only part of the balloon was inserted into the subclavian and brachiocephalic arteries, and the rest of balloon was inserted into proximal RCCA in the other 28 rabbits (group 2). The balloon was inflated with just enough iodinated contrast material to achieve flow arrest in the RCCA. Porcine elastase (5.23 U/mgP, 40.1 mgP/mL, approximately 200 U/mL; Worthington Biochemical Corporation, Lakewood, NJ) mixed with iodinated contrast material was incubated in the dead space of the RCCA, above the inflated balloon, through a microcatheter (Tracker 10, Target Therapeutics, Fremont, CA). Balloon position and shape were documented by using fluoroscopic spot imaging, which was saved and printed. After incubation of the elastase solution, the balloon and sheath were removed, and the RCCA was ligated below the sheath entry site.
Follow-Up Angiography
Intra-arterial DSA (IADSA) was performed at least 3 weeks after creation, because our previous study has indicated that the elastase-induced aneurysms remain stable beyond 3 weeks (8). The animals were anesthetized as described above. By using a sterile technique, surgical exposure of the right common femoral artery was performed and a 5F vascular sheath was placed. Heparin (100 U/kg) was administered intravenously. A 5F catheter (Envoy, Cordis Endovascular) was advanced into the brachiocephalic artery and digital subtraction angiography (DSA) was performed. An external sizing device was in place during IADSA. Two observers (Y.H.D. and M.A.D.) measured the sizes of the aneurysms independently, which were determined in reference to the external sizing device. Aneurysm formation was considered to have been achieved when the maximum diameter of the RCCA exceeded 2.5 mm. The necks of aneurysms were characterized as narrow (neck diameter, ≤4 mm) or wide (neck diameter, > 4 mm). Continuous variables were compared by using the Student t test. Proportions were compared by using Fisher exact test (J.N.M. and Y.H.D.).
Definition of Experimental Groups
A single experienced observer (Y.H.D.) viewed the spot films of balloon position obtained during aneurysm creation surgery, to determine group assignment. We defined the study sample on the basis of height of the balloon relative to the CCA. Group 1 had lower balloon position, where the inflated balloon was located completely in the brachiocephalic artery and right subclavian artery across the origin of RCCA, without herniation of the balloon into the RCCA (Fig 1). Group 2 had higher balloon position, where the inflated balloon was located not only in the brachicephalic/subclavian arteries, but also within the proximal RCCA (Fig 2).
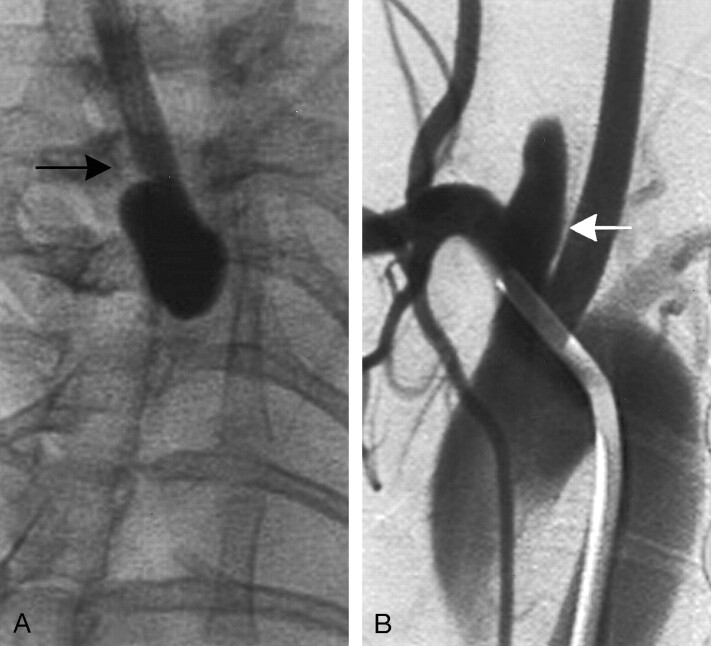
Fig 1.
Group 1 subject (low balloon position).
A, Anteroposterior (AP) spot film obtained during aneurysm creation surgery. The RCCA is opacified with the elastase/iodinated contrast mixture. Note that the inflated balloon is completely in right subclavian artery and brachiocephalic artery (black arrow).
B, Intra-arterial digital subtraction angiogram, right anterior oblique view, demonstrating a wide-necked aneurysm (white arrow). Neck size is 5.3 mm.
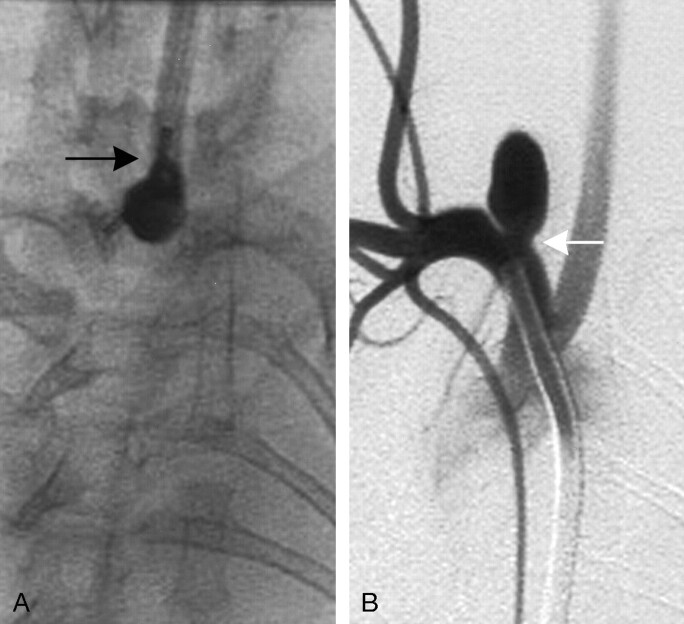
Fig 2.
Group 2 subject (high balloon position).
A, AP spot film obtained during aneurysm creation surgery. The RCCA is opacified with the elastase/iodinated contrast mixture. Note that a small portion of the inflated balloon has herniated into the proximal RCCA (black arrow).
B, Intra-arterial digital subtraction angiogram, right anterior oblique view, demonstrating a narrow-neck aneurysm (white arrow). Neck size is 1.9 mm.
Interobserver variability was measured by using intraclass correlation (ICC). ICC of <0.4 indicates poor reproducibility, ICC between 0.4 and 0.75 indicates fair to good reproducibility, and ≥0.75 indicates excellent reproducibility.
Results
Aneurysm sizes are shown in the Table. Representative images are shown in Figs 1 and 2. Interobserver reproducibility was excellent for all measurements (ICC > 0.75). Mean aneurysm widths for groups 1 and 2 were 3.8 ± 1.0 mm (range, 2.1–6.6 mm) and 3.3 ± 0.9 mm (range, 1.4–4.8 mm), respectively (P < .05). Mean aneurysm neck sizes for groups 1 and 2 were 3.4 ± 1.2 mm (range, 1.6–6.3 mm) and 2.3 ± 0.9 mm (range, 1.4–4.6 mm), respectively (P < .001). Eighteen (29%) of 62 aneurysms in group 1 were wide necked; in group 2, 1 (4%) of 28 aneurysms was wide necked (P < .005). Mean dome-to-neck ratios for groups 1 and 2 were 1.2 ± 0.4 (range, 0.7–2.7) and 1.7 ± 0.7 (range, 0.9–3.7), respectively (P < .005). Mean heights for groups 1 and 2 were 8.0 ± 1.7 mm (range, 5.2–12.9 mm) and 7.5 ± 2.2 mm (range, 3.1–13.3 mm), respectively (P > .05).
Aneurysm sizes in Groups 1 and 2
| Group 1 (n = 62) | Group 2 (n = 28) | P Value | |
|---|---|---|---|
| Width (mm) | 3.8 ± 1.0 | 3.3 ± 0.9 | <.05 |
| Neck diameter (mm) | 3.4 ± 1.2 | 2.3 ± 0.9 | <.001 |
| Dome: neck ratio | 1.2 ± 0.4 | 1.7 ± 0.7 | <.005 |
| Height (mm) | 8.0 ± 1.7 | 7.5 ± 2.2 | >.05 |
Values are expressed as mean ± SD.
Discussion
Elastase-induced aneurysms in rabbits represent an important advance in aneurysm model research; however, unlike surgical models in which the size of the aneurysm cavity and neck can be controlled by choice of vein pouch and suture technique (4), control of elastase-induced aneurysm morphology is difficult (7–9). We previously conducted a retrospective study, which indicated that neck size of elastase-induced aneurysm can be controlled by adjusting position of the occlusion balloon during elastase incubation (Y. H. Ding et al, unpublished data). In the current, prospective study, the results showed higher position of the balloon during aneurysm creation induced narrow necks and higher dome-to-neck ratio aneurysms. Conversely, lower position of the balloon induced wide necks and lower dome-to-neck ratio aneurysms. These findings are consistent with the results shown in our retrospective study.
We can only conjecture about the reason that the higher position of the inflated balloon induced narrow neck and higher dome-to-neck ratio aneurysms. It is possible that the inflated balloon herniating cephalad into the proximal RCCA protects the neck region from elastase injury. Conversely, if the inflated balloon is placed entirely in the brachiocephalic and right subclavian artery, without herniation into the proximal RCCA, the most proximal segment of the RCCA would have been exposed to elastase injury. Because the balloon position only involved the origin of RCCA, the distal RCCA was exposed to elastase in a similar situation between group 1 and 2, so there was no significant difference of the height of aneurysms between these 2 groups. These results should prove useful to investigators who employ the rabbit elastase-induced aneurysm model for preclinical testing of aneurysm occlusion devices, which requires certain shapes of aneurysms, especially with narrow or wide necks.
Our previous, retrospective study demonstrated a significant difference in neck diameter between low and high balloon position, but no difference in aneurysm width. This current, prospective study showed differences in both neck size and aneurysm width. Disparity between these 2 studies may reflect a more consistent balloon position in the prospective trial as compared with the retrospective trial.
Although we found differences in mean neck and aneurysm widths, investigators cannot expect that all aneurysms made with low balloon position will be wide necked or that high position will guarantee a narrow neck. These data reflect differences in mean dimensions, with some overlap between groups.
This study suffers from several limitations. First, exact aneurysm cavity and neck dimensions are subject to interpretation error. Thus, we employed 2 readers for measurement in this study to diminish such errors. Second, the numbers in the higher position group still are not large, and additional studies are ongoing.
Conclusion
Neck size of elastase-induced aneurysm models in rabbits can be controlled by adjusting the position of the inflated balloon, which makes this model relevant for testing of neurointerventional devices.
References
- 1.Hashimoto N, Handa H, Hazama F. Experimentally induced cerebral aneurysms in rats. Part III. Pathology. Surg Neurol 1979;11:299–304 [PubMed] [Google Scholar]
- 2.Cloft HJ, Altes TA, Marx WF, et al. Endovascular creation of an in vivo bifurcation aneurysm model in rabbits. Radiology 1999;213:223–228 [DOI] [PubMed] [Google Scholar]
- 3.Sorteberg A, Sorteberg W, Rappe A, et al. Effect of Guglielmi detachable coils on intraaneurysmal flow: experimental study in canines. AJNR Am J Neuroradiol 2000;23:288–294 [PMC free article] [PubMed] [Google Scholar]
- 4.Guglielmi G, Ji C, Massoud TF, et al. Experimental saccular aneurysms. II. A new model in swine. Neuroradiology 1994;36:547–550 [DOI] [PubMed] [Google Scholar]
- 5.Stehbens WE. Histological changes in chronic experimental aneurysms surgically fashioned in sheep. Pathology 1997;29:374–379 [DOI] [PubMed] [Google Scholar]
- 6.Reul J, Weis J, Spetzger U, et al. A long-term angiographic and histopathologic findings in experimental aneurysms of the carotid bifurcation embolized with platinum and tungsten coils. AJNR Am J Neuroradiol 1997;18:35–42 [PMC free article] [PubMed] [Google Scholar]
- 7.Altes TA, Cloft HJ, Short JG, et al. 1999 ARRS Executive Council Award: creation of saccular aneurysms in the rabbit: a model suitable for testing endovascular devices: American Roentgen Ray Society. AJR Am J Roentgenol 2000;174:349–354 [DOI] [PubMed] [Google Scholar]
- 8.Fujiwara NH, Cloft HJ, Marx WF, et al. Serial angiography in an elastase-induced aneurysm model in rabbits: evidence for progressive aneurysm enlargement after creation. AJNR Am J Neuroradiol 2001;22:698–703 [PMC free article] [PubMed] [Google Scholar]
- 9.Short JG, Fujiwara NH, Marx WF, et al. Elastase-induced saccular aneurysms in rabbits: comparison of geometric features with those of human aneurysms. AJNR Am J Neuroradiol 2001;22:1833–1837 [PMC free article] [PubMed] [Google Scholar]
- 10.Kallmes DF, Fujiwara NH, Berr SS, et al. Elastase-induced saccular aneurysms in rabbits: a dose-escalation study. AJNR Am J Neuroradiol 2002;23:295–298 [PMC free article] [PubMed] [Google Scholar]
- 11.Kallmes DF, Helm GA, Hudson SB, et al. Histologic evaluation of platinum coil embolization in an aneurysm model in rabbits. Radiology 1999;213:217–222 [DOI] [PubMed] [Google Scholar]
- 12.Kallmes DF, Fujiwara NH. New expandable hydrogel-platinum coil hybrid device for aneurysm embolization. AJNR Am J Neuroradiol 2002;23:1580–1588 [PMC free article] [PubMed] [Google Scholar]
- 13.Kallmes DF, Fujiwara NH, Yuen D, et al. A collagen-based coil for embolization of saccular aneurysms in a New Zealand White rabbit model. AJNR Am J Neuroradiol 2003;24:591–596 [PMC free article] [PubMed] [Google Scholar]
- 14.Fujiwara NH, Kallmes DF. Healing response in elastase-induced rabbit aneurysms after embolization with a new platinum coil system. AJNR Am J Neuroradiol 2002;23:1137–1144 [PMC free article] [PubMed] [Google Scholar]
- 15.Marx WF, Cloft HJ, Helm GA, et al. Endovascular treatment of experimental aneurysms by use of biologically modified embolic devices: coil-mediated intraaneurysmal delivery of fibroblast tissue allografts. AJNR Am J Neuroradiol 2001;22:323–333 [PMC free article] [PubMed] [Google Scholar]
- 16.De Gast AN, Altes TA, Marx WF, et al. Transforming growth factor beta-coated platinum coils for endovascular treatment of aneurysms: an animal study. Neurosurgery 2001;49:690–696 [DOI] [PubMed] [Google Scholar]