Abstract
BACKGROUND AND PURPOSE: Carotid angioplasty and stent placement may be the preferred treatment in patients with carotid dissection who have failed medical management. The goal of this study was to determine the procedural feasibility and safety as well as long-term complication rates of carotid angioplasty and stent placement in a consecutive cohort of relatively young, high-surgical-risk patients.
PATIENTS AND TECHNIQUES: A series of 26 consecutive patients (mean age, 49 years; 15 men and 11 women) who underwent angioplasty and stent placement for carotid dissection with or without pseudoaneurysm from April 1997 to April 2005 at our institution (9 traumatic, 8 spontaneous, and 9 iatrogenic) was retrospectively reviewed. Twenty-eight stents were used in 29 procedures performed on 27 vessels (20 internal carotid arteries and 7 common carotid arteries). Patients were followed with cerebral angiography, CT, sonography, or clinically for a mean of 14.6 months (range, 5 days to 48.2 months) with 17 of 26 patients having at least 6 months of follow-up. Procedural and long-term complication rates were calculated.
RESULTS: Dissection-induced stenosis was reduced from 71 ± 18% to no significant stenosis in 20 of the 21 patients with measurable stenosis. The procedural transient ischemic attack (TIA) rate was 3 of 29 procedures (10.3%). There were no procedural strokes. One patient required angioplasty of a common femoral artery. One procedure was terminated when an asymptomatic new intimal flap was created before intervention. Two patients had occlusions of the treated vessel noted at 22 days (presented with contralateral stroke) and 3.4 months (asymptomatic). There were 2 unrelated deaths from myocardial infarction at 8 days and 15.2 months. Two patients had recurrent ipsilateral TIA at 2.7 months and 12 months. The 30-day occlusion and death rate was 2 of 29 procedures (6.9%).
CONCLUSION: In this series, angioplasty and stent placement were effective in relieving stenosis secondary to carotid dissection with or without pseudoaneurysm and have low rates of ischemic complications.
Dissection of the carotid artery is an important cause of stroke in young patients, accounting for approximately 20% of stroke in patients <45 years of age (1–3). Dissection may be spontaneous, traumatic, or iatrogenic in origin (4, 5). Patients typically present with pain, Horner syndrome, or ischemia (6) that usually occurs within the first week (7).
Conservative treatment with medical therapy may be used in patients who remain asymptomatic and possibly in some symptomatic patients if no contraindications exist. Medical therapy generally consists of anticoagulant or antiplatelet agents (2, 3). No randomized prospective studies have defined optimal treatment (5, 8). Some retrospective studies have shown benefit of anticoagulation, and one study did not demonstrate any difference between anticoagulant and antiplatelet agents (9). Symptomatic patients are usually systemically anticoagulated with heparin and then, possibly, warfarin (3, 10). If symptoms persist or progress despite medical therapy, prompt intervention is indicated (7). More aggressive treatment may be indicated in selected asymptomatic patients with persistent significant stenosis as well.
Surgical intervention is possible but is often difficult because of the typically distal location of carotid dissections and longer length of lesions compared with atherosclerotic stenosis. Surgical intervention is associated with a high complication rate and normally consists of either ligation or bypass, because carotid endarterectomies (CEAs) are generally not recommended (11, 12). Endovascular treatment with angioplasty and stent placement has supplanted surgery when intervention is indicated and is now the treatment of choice in symptomatic dissections not responding to anticoagulants (13–16). Endovascular techniques also permit possible treatment of associated pseudoaneurysms.
Angioplasty and stent placement in carotid dissection has not been thoroughly studied. Aside from multiple case reports generally consisting of one or 2 patients, the largest reported series to date included 10 patients (17–28). We report the results of endovascular treatment in 26 patients with extracranial carotid dissections with or without associated pseudoaneurysms.
Patients and Techniques
Patient Selection
Between April 4, 1997, and April 7, 2005, 175 patients underwent carotid angioplasty and/or stent placement at our institution. Of them, 26 patients were treated for extracranial carotid dissections in a total of 29 procedures (one patient had 4 procedures).
Patients were selected for treatment if the dissection and/or pseudoaneurysm caused a high-grade stenosis by the North American Symptomatic Carotid Endarterectomy Trial (NASCET) criteria for symptomatic patients (29) or Asymptomatic Carotid Atherosclerosis Study (ACAS) criteria for asymptomatic patients (30). In patients with a pseudoaneurysm and no stenosis, treatment was pursued if it was thought that angioplasty and/or stent placement would prevent distal emboli arising from the pooling of blood (all patients with pseudoaneurysm and no stenosis were treated). Patients were also treated to control bleeding.
Institutional review board approval was obtained for the study, and written informed consent was obtained for the procedures. The patients’ medical records were retrospectively reviewed for imaging reports (cerebral angiography, CT, or sonography) and available clinical follow-up. Brief telephone interviews with patients, immediate family, or care personnel were also used.
Patient Characteristics
The 26 patients ranged in age from 19 to 81 years (mean, 49 years). Fifteen were men, and 11 were women. Fourteen patients (53.8%) presented with focal neurologic symptoms referable to the subsequently treated carotid dissection. Eleven of the 14 symptomatic patients presented with hemispheric or ocular transient ischemic attacks (TIAs; n = 7) or strokes (n = 4). Three of 14 symptomatic patients presented with a cranial nerve palsy (n = 2) or Horner syndrome (n = 1). Patient characteristics are reviewed in Table 1.
TABLE 1:
Patient characteristics
| Patient No./Age (y)/Sex | Symptomatic | Vessel | Etiology of Dissection |
|---|---|---|---|
| 1/66/M | No | RCCA | Iatrogenic |
| 2/51/M | TIA | RICA | Iatrogenic |
| 3/43/F | No | RICA | Spontaneous |
| 4/36/F | CN palsy | LICA | Trauma |
| 5/43/M | No | LICA | Spontaneous |
| 6/56/M | TIA | RICA | Spontaneous (FMD) |
| 7/56/F | Stroke | LCCA | Iatrogenic |
| 8/45/F | No | RICA | Spontaneous |
| 9/76/F | CN palsy | LICA | Spontaneous |
| 10/47/M | No | LICA | Iatrogenic |
| 11/40/F | No | LICA | Spontaneous |
| 12/34/F | Stroke | LICA | Trauma |
| 13/45/F | Stroke | RICA | Spontaneous (FMD) |
| 14/44/M | No | RCCA | Iatrogenic |
| 15/52/M | TIA | LCCA | Iatrogenic |
| 16/35/F | TIA | RICA | Trauma |
| 17/81/F | No | LICA | Spontaneous |
| 18/22/M | No | RICA, LCCA | Trauma |
| 19/19/M | No | LICA | Trauma |
| 20/60/M | TIA | LICA | Trauma |
| 21/42M | TIA | LICA | Trauma |
| 22/51/M | No | LICA | Trauma |
| 23/52/M | Horner syndrome | LICA | Trauma |
| 24/66/M | No | RCCA | Iatrogenic |
| 25/46/M | TIA | RICA | Iatrogenic |
| 26/72/F | Stroke | LCCA | Iatrogenic |
Note.—TIA indicates transient ischemic attack; CN, cranial nerve; R, right; L, left; ICA, internal carotid artery; CCA, common carotid artery; FMD, fibromuscular dysplasia.
The 12 patients without neurologic symptoms referable to the subsequently treated dissection were treated for varied reasons. Two patients were treated for restenosis on postendarterectomy follow-up imaging (patients 1 and 24 with 80% and 90% restenosis, respectively). Two patients were either symptomatic or occluded on the contralateral side (patients 3 and 5). One patient was treated to prepare for a contralateral carotid sacrifice (patient 8).
Three patients presented with bleeding. Patient 10 suffered from massive oral and nasal hemorrhage following resection of an oropharyngeal carcinoma. Patient 14 developed an enlarging neck hematoma after placement of a right internal jugular Quinton catheter (Quinton Instruments Co., Seattle, WA). Patient 18 presented with epistaxis following a high-speed motor vehicle crash.
One patient experienced daily headaches, neck pain, and dizziness (patient 11; Fig 1). One patient was treated for an incidental pseudoaneurysm noted during stent placement for a prior symptomatic atherosclerotic stenosis (patient 17). One young patient with a long segment of dissection from the mid-C2 vertebral body to the level of the cavernous internal carotid artery was unresponsive after a gunshot wound to the neck (patient 19; Fig 2). The last patient had an incidental dissection noted on a MR angiographic screening examination for a family history of intracranial aneurysms (patient 22).
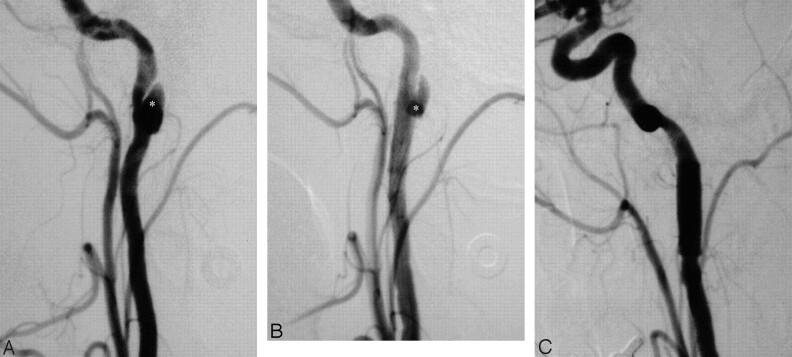
Fig 1.
Patient 11.
A, Lateral digital subtraction angiography (DSA) of a 40-year-old woman with an intimal flap within the distal cervical portion of the left internal carotid artery resulting in pseudoaneurysm (windsock deformity, asterisk) and 75% stenosis.
B, A 6 × 20 mm Smart stent (Cordis Corp.) was placed with no residual stenosis and improved anterograde flow (lateral projection). There was residual slow filling of the pseudoaneurysm (asterisk).
C, Follow-up angiography at 25 months revealed a widely patent stent with no filling of the pseudoaneurysm (lateral projection).
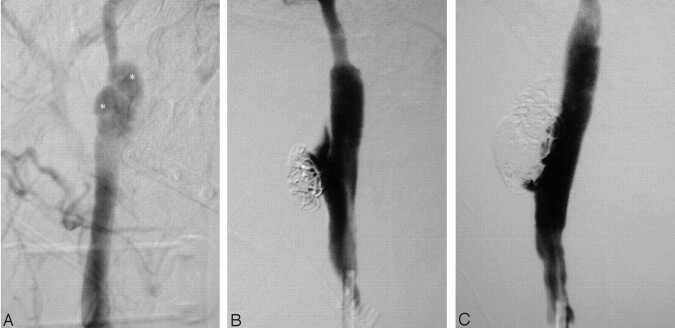
Fig 2.
Patient 19.
A, Lateral DSA of a 19-year-old man with a traumatic pseudoaneurysm arising from the left internal carotid artery at the level of the mid-C2 vertebral body. There was a long segment of dissection flap (arrows) from the pseudoaneurysm (asterisk) to the level of the cavernous internal carotid artery.
B, Road-mapping guidance was used to select the true lumen with a 0.018-inch Roadrunner guidewire (Cook Inc.). A 9 × 30 mm Precise stent (Cordis Corp.) was placed across the neck of the pseudoaneurysm (asterisk), which resulted in slower flow within the pseudoaneurysm (lateral projection).
C, Follow-up angiography at 6.2 months showed normal caliber at the site of injury with healing of the pseudoaneurysm and dissection flap (lateral projection).
The carotid dissections were traumatic (9 patients), spontaneous (8 patients), or iatrogenic (9 patients) in origin. Of the patients with spontaneous dissections, 2 had findings strongly suggestive of fibromuscular dysplasia (patients 6 and 13). The iatrogenic dissections were due to intimal flaps following CEA (patients 1, 2, 15, and 26), arterial injury during superior hypophyseal aneurysm clipping (patient 7), injury during oropharyngeal or laryngeal carcinoma resection (patients 10 and 25), carotid injury during placement of a right internal jugular catheter (patient 14), and an intimal flap formed at the junction of 2 previously placed stents (patient 24).
As traumatic or spontaneous dissections commonly occur in areas of high mobility, 13 of the 17 cases (76.5%) of traumatic or spontaneous dissections occurred at or near the skull base. In the 9 patients with iatrogenic dissections, 8 (88.9%) occurred near the bifurcation of the common carotid artery.
Procedure
Procedures were performed by one of 3 neurointerventional staff (C.J.M., D.T.C., C.P.D.) and the neurointerventional fellow. Elective patients were pretreated with aspirin 325 mg orally each day 5 days before the procedure and, beginning in 1999, clopidogrel bisulfate 75 mg (Plavix, Bristol-Myers Squibb/Sanofi Pharmaceuticals Partnership, New York, NY) in addition to aspirin. Hospitalized patients with acute dissections were treated with heparin. During the procedure, intravenous heparin was used to maintain an activated clotting time between 250 and 300 seconds. Most procedures (n = 26) were performed with intravenous conscious sedation; the remainder (n = 3) were performed with general anesthesia to protect the airway, control patient movement, and/or manage an uncooperative patient.
All patients initially underwent diagnostic cerebral angiography on a dedicated biplanar neuroangiographic unit (Neurostar; Siemens AG, Munich, Germany). Transfemoral arterial access was used for all procedures. Carotid dissection with or without pseudoaneurysm was documented in either the internal or common carotid artery. Intracranial images were routinely obtained before and after the interventions to confirm patency of intracranial vessels.
For the intervention, a 6- or 7F long sheath (Shuttle, Cook Inc., Bloomington, IN) or equivalent was placed in the carotid artery proximal to the dissection. Using road-mapping guidance, the dissection was crossed with a 0.018-inch exchange length guidewire (Roadrunner, Cook Inc.) over which the angioplasty balloon and stent were advanced as needed. The true lumen was readily apparent in the patients when dissection was remote. In the acute setting, the true lumen was assured by placing the wire above the re-entry site of the flap. In only one instance was there some difficulty ascertaining the position of the guidewire within the true lumen. Intravenous atropine or glycopyrrolate (American Regent, Inc., Shirley, NY) was administered in 3 of the 29 procedures for prophylaxis or treatment of bradycardia. No cerebral protection devices were used.
A total of 28 self-expanding stents—12 Precise stents (Cordis Corp., Miami Lakes, FL), 9 Smart stents (Cordis Corp.), and 7 Wallstents (Boston Scientific Corp., Natick, MA)—were used in 29 procedures performed on 27 vessels (20 internal carotid arteries and 7 common carotid arteries) in the 26 patients in the present series as shown in Table 2. In the case of one patient involved in a motor vehicle crash, stents were placed in an internal carotid artery on one side and a common carotid artery on the other (patient 18). In the case of this patient, 3 procedures were performed on each of the 2 vessels, with the common carotid artery receiving 2 stents in the second procedure. Two patients did not receive a stent. Of them, one patient had angioplasty only (patient 13), and the other had the procedure terminated with no intervention performed because a new intimal flap was raised (patient 9).
TABLE 2:
Treatment
| Patient No. | Prestent Stenosis (%) | Poststent Stenosis (%) | Pseudo-aneurysm | Stent | Size (mm) |
|---|---|---|---|---|---|
| 1 | 80 | 0 | No | Wallstent | 10 × 42 |
| 2 | 70 | 0 | No | Wallstent | 10 × 20 |
| 3 | 75 | 0 | 1 | Wallstent | 5 × 20 |
| 4 | 60 | 0 | 1 | Wallstent | 5 × 20 |
| 5 | 95 | 0 | No | Wallstent | 6 × 20 |
| 6 | 95 | 0 | 1 | Wallstent | 8 × 20 |
| 7 | 60 | 0 | No | Wallstent | 10 × 42 |
| 8 | 50 | 0 | 1 | Smart | 10 × 40 |
| 9 | 60 | No intervention | 1 | N/A | N/A |
| 10 | 60 | 0 | 1 | Smart | 6 × 20 |
| 11 | 75 | 0 | 1 | Smart | 6 × 20 |
| 12 | 60 | 0 | 1 | Smart | 7 × 20 |
| 13 | 80 | 0 | No | Angioplasty only | N/A |
| 14 | 0 | 0 | 1 | Smart | 10 × 20 |
| 15 | 85 | 0 | No | Smart | 9 × 30 |
| 16 | 50 | 0 | 2 | Precise | 6 × 40 |
| 17 | 0 | 0 | 1 | Precise | 6 × 30 |
| 18: 1st RICA | 0 | 0 | 1 | Precise | 7 × 30 |
| 18: 1st LCCA | 0 | 0 | 1 | Smart | 12 × 40 |
| 18: 2nd RICA | 0 | 0 | 1 | Precise | 7 × 30 |
| 18: 2nd LCCA | 0 | 0 | 1 | Smart, | 12 × 40, |
| Smart | 12 × 40 | ||||
| 19 | 90 | 0 | 1 | Precise | 9 × 30 |
| 20 | 70 | 50 | No | Precise | 6 × 40 |
| 21 | 99 | 0 | 1 | Precise | 7 × 40 |
| 22 | 65 | 0 | 1 | Precise | 7 × 40 |
| 23 | 25 | 0 | 1 | Precise | 8 × 40 |
| 24 | 90 | 0 | No | Precise | 9 × 20 |
| 25 | 0 | 0 | 1 | Precise | 9 × 40 |
| 26 | 0 | 0 | 2 | Precise | 7 × 30 |
Note.—R indicates right; L, left; ICA, internal carotid artery; CCA, common carotid artery; N/A, not applicable; Wallstent (Boston Scientific, Natick, MA); Smart, Precise (Cordis, Miami Lakes, FL).
The stents were oversized by 1–2 mm to the largest diameter of the artery to be treated. The first 7 procedures used Wallstents (Boston Scientific Corp.), and the last Wallstent was used in October 1998. The Smart (Cordis Corp.) or Precise (Cordis Corp.) stent was adapted in lieu of the Wallstent, because their cell characteristics allowed for abrupt changes in stent lumen diameter. Two procedures resulted in a stent placed across the carotid bifurcation; however, the external carotid remained patent in both cases.
Stent placement without angioplasty was performed in 21 procedures. The criteria for this choice were an adequate lumen to position the stent-delivering catheter and no residual stenosis after stent expansion. Balloon angioplasty was required in 2 procedures before stent placement and in 5 procedures after stent placement. One case required both prestent and poststent angioplasty. Poststent angioplasty was not performed in vessels that were sufficiently dilated with initial angioplasty and stent placement.
A total of 21 dissection-associated pseudoaneurysms in 19 vessels were detected in 18 patients. Two patients had two pseudoaneurysms in a single vessel (patients 16 and 26). Another patient had an associated pseudoaneurysm in each of 2 vessels (patient 18). A pseudoaneurysm was defined as an outpouching of the vessel wall; vessel dilations secondary to dissection flap formation were not included in this group. The average pseudoaneurysm measured 13 mm in the longest dimension (parallel to the path of the vessel). All pseudoaneurysms were treated with a stent across the neck of the aneurysm.
Four pseudoaneurysms in 4 different patients were additionally treated with one or more Guglielmi detachable coils delivered by using a microcatheter (Prowler Plus, Cordis Corp.) placed over a guidewire (Transcend; Boston Scientific Corp.) through the interstices of the stent into the pseudoaneurysm lumen.
Three were done because the patients presented with bleeding from blood collecting in the adjacent tissue spaces: patient 10 presented with massive postsurgical hemorrhage from resection of an oropharyngeal cancer, patient 14 presented with a large (4-cm) iatrogenic pseudoaneurysm after line placement, and patient 18 presented with traumatic epistaxis (Fig 3). The fourth coiled pseudoaneurysm was done because the pseudoaneurysm failed to collapse after deployment of the stent (patient 12).
Fig 3.
Patient 18.
A, Oblique frontal DSA of a 22-year-old man with a traumatic dissection with flow-limiting stenosis and a large pseudoaneurysm (asterisks) of the upper cervical right internal carotid artery near the skull base.
B, A 7 × 30 mm Precise stent (Cordis Corp.) was placed with reversal of the associated stenosis (lateral projection). The pseudoaneurysm associated with the dissection, aside from stent placement, was also treated by coil embolization with a reduction in its size; however, the tear in the internal carotid artery at this level was large and the pseudoaneurysm partially filled.
C, There was an interval increase in the size of the pseudoaneurysm with coil compaction at 19 days (lateral projection). The pseudoaneurysm was retreated by placement of additional coils and deployment of a second 7 × 30 mm Precise stent (Cordis Corp.) across the pseudoaneurysm neck, which resulted in near-total obliteration. The internal carotid artery flow remained normal and the true lumen fully patent and clear of thrombus.
A femoral closure device was used in 10 procedures. The devices included 7 Perclose (Abbott Laboratories, Abbott Park, IL), 2 AngioSeal (St. Jude Medical Inc., St. Paul, MN), and 1 Duett (Vascular Solutions Inc., Minneapolis, MN). Manual compression was used in the remaining 19 procedures after the activated clotting time had returned to normal. Patients were monitored in the intensive care unit following the procedure with mean arterial pressure maintained within 20 mmHg above or below baseline. They were discharged the following day with the exception of those who experienced periprocedural neurologic symptoms. Aspirin and Plavix were continued for 30 days postprocedure, and aspirin was continued indefinitely.
Results
Technical Outcome
Twenty-one patients had a dissection-induced stenosis. Five patients (6 vessels) had pseudoaneurysms with no stenosis (patients 14, 17, 18, 25, and 26). In patients with a stenosis, the mean measured 71 ± 18% calculated according to the NASCET method (29).
Following treatment, all patients had no significant residual stenosis, with one exception. Patient 20 was left with 50% residual stenosis in light of transient left middle cerebral artery territory deficits (without an angiographic correlate) that developed after stent placement. It was decided not to pursue a second stent placement or poststent angioplasty, because the deficits were likely due to small emboli, which suggests the dissection may have had associated adherent thrombus. All pseudoaneurysms, regardless of whether they were coiled, were completely obliterated by the end of the procedure or on follow-up angiography.
Immediate Clinical Outcome
The procedural TIA rate was 3 of 29 procedures (10.3%; patients 13, 18, and 20). Only one of these patients was previously neurologically asymptomatic. There were no procedural strokes. One patient had decreased distal pulses, which resulted in angioplasty of the left common femoral artery (patient 12). One procedure was terminated when a new intimal flap was created before the intervention was performed (patient 9). The patient remained asymptomatic. There were no significant groin hematomas that required blood transfusion or prolonged hospitalization.
Follow-Up Observations
The mean follow-up was 14.6 months (range, 5 days to 48.2 months), with 17 of 26 patients having at least 6 months’ follow-up (Table 3). Nine patients had clinical follow-up only; the remaining 17 patients had clinical and imaging follow-up in the form of cerebral angiography (13 patients), CT (CT of head and neck in patient 10 and CT of head only in patients 14 and 17), or sonography (patient 15).
TABLE 3:
Complications
| Patient No. | Procedural | Long-term | Imaging Follow-up (mo) | Clinical Follow-up (mo) |
|---|---|---|---|---|
| 1 | No | Deceased post-MI | 0.3 | |
| 2 | No | Recurrent TIA | Angiography (12) | 12 |
| 3 | No | No | 48.2 | |
| 4 | No | Asymptomatic ipsilateral occlusion | Angiography (3.4) | 3.4 |
| 5 | No | Ipsilateral occlusion, contralateral stroke | Angiography (0.7) | 0.7 |
| 6 | No | Contralateral CEA, stroke | Angiography (7.4) | 7.4 |
| 7 | No | No | 1.3 | |
| 8 | No | No | Angiography (2.1) | 2.1 |
| 9 | New intimal flap | No | 19.0 | |
| 10 | No | No | CT (41.5) | 41.5 |
| 11 | No | No | Angiography (25.0) | 25.0 |
| 12 | Decreased distal pulses | No | 28.0 | |
| 13 | TIA | No | Angiography (40.1) | 40.1 |
| 14 | No | No | CT (18.4) | 18.5 |
| 15 | No | No | US (24.4) | 24.4 |
| 16 | No | Recurrent TIA | Angiography (2.7) | 2.7 |
| 17 | No | Deceased post-MI | CT (15.2) | 15.2 |
| 18: 1st RICA | No | No | Angiography (10.8) | 16.0 |
| 18: 1st LCCA | No | No | Angiography (10.8) | 16.0 |
| 18: 2nd RICA | TIA | No | Angiography (10.2) | 15.4 |
| 18: 2nd LCCA | No | No | Angiography (10.2) | 15.4 |
| 19 | No | No | Angiography (6.2) | 23.9 |
| 20 | TIA | No | Angiography (11.2) | 11.2 |
| 21 | No | No | Angiography (6.4) | 13.4 |
| 22 | No | No | 5.3 | |
| 23 | No | No | Angiography (5.6) | 9.5 |
| 24 | No | No | 7.0 | |
| 25 | No | No | 1.6 | |
| 26 | No | No | 0.2 |
Note.—R indicates right; L, left; ICA, internal carotid artery; CCA, common carotid artery; TIA, transient ischemic attack; MI, myocardial infarction; CEA, carotid endarterectomy; CT, computed tomography; US, ultrasound.
In the cases of 2 patients, interval occlusion of treated internal carotid arteries was demonstrated on repeat angiography (patients 4 at 3.4 months and patient 5 at 22 days). Patient 4 remained asymptomatic. Patient 5 initially presented with a stroke and occlusion contralateral to his treated side. He returned with a recurrence of symptoms on the contralateral side and a new occlusion on the treated side. There were 2 deaths from unrelated myocardial infarction 8 days (patient 1) and 15.2 months (patient 17) postprocedure. Two patients had recurrent ipsilateral TIAs 2.7 months (patient 16) and 12 months (patient 2) postprocedure. Both patients had repeat diagnostic angiograms that showed no abnormalities. Patient 6 suffered a contralateral stroke after undergoing a CEA on that side 1 month postprocedure; however, he has remained asymptomatic with a normal angiogram on his stented side at 7.4 months. The composite 30-day occlusion and death rate was 2 of 29 procedures (6.9%).
Discussion
A tear in the wall of a carotid artery—whether spontaneous, traumatic, or iatrogenic in origin—may allow blood to divide its layers, resulting in a false lumen causing carotid stenosis, pseudoaneurysm, or both. This phenomenon had historically been known to be a rare cause of stroke, and, until the use of modern diagnostic techniques in the late 1970s, the diagnosis was generally made postmortem (31–33). Today, on the basis of MR imaging and angiographic data, the annual incidence of spontaneous carotid dissection is estimated to be 2.5–3 per 100,000 (34, 35). Although dissections account for only 2% of all ischemic strokes, they are an important cause of stroke in younger patients.
NASCET demonstrated the unequivocal benefit of endarterectomy over medical management in symptomatic patients with severe carotid stenosis of at least 70% (17% absolute risk reduction of ipsilateral stroke during a 2-year period). More recently, the benefit of carotid endarterectomy in patients with symptomatic but more moderate stenosis of 50%–69% has been reported (6.5% absolute risk reduction of ipsilateral stroke during a 5-year period; 29). In the case of asymptomatic disease, ACAS estimated the 5-year risk of ipsilateral stroke and any perioperative stroke or death in good surgical candidates with carotid artery stenosis of 60% or greater was 5.1% versus 11.0% in medically treated patients (30). These studies are the basis for surgical treatment of moderate to severe carotid stenosis in good surgical candidates and also served as criteria for endovascular treatment of dissections causing such stenosis in the present series.
The use of carotid stents for atherosclerotic disease has been widely studied and shown to be an effective therapeutic alternative to carotid endarterectomy (36–43). Although risks associated with stent placement for atherosclerosis are not necessarily the same as risks associated with stent placement for dissection, the latest randomized controlled trial, Stent placement and Angioplasty with Protection in Patients at HIgh Risk for Endarterectomy (SAPPHIRE), found that carotid stent placement with a cerebral protection device was not inferior to endarterectomy in a population of high-surgical-risk patients (42). Most recently, the procedural stroke rate in a large series of unprotected patients was found to be 2.4% with a 30-day stroke and death rate of 5% (43).
The management of carotid dissections has remained controversial. Although many patients who have failed conservative medical therapy are referred for endovascular treatment with angioplasty and stent placement, there have been no well-designed studies to support this practice. In the largest series to date, Malek et al reported 10 patients who had extracranial carotid dissections treated with endovascular stent placement with clinical follow-up of 16.5 months (14). They reported no periprocedural complications and demonstrated significant improvement of clinical outcome measures.
Liu et al reported a series of 7 patients with no procedural complications, one asymptomatic occlusion at 3 months, and no other complications, angiographic or clinical, during a mean follow-up period of 3.5 years (28). Bejjani et al reported 5 patients with symptomatic carotid dissections with all good clinical outcomes, though follow-up was very limited (15). Bush et al reported 5 symptomatic patients with pseudoaneurysms with 100% technical success in obliterating the pseudoaneurysms (16). Three of the 5 patients had mean angiographic follow-up of 11.7 months that showed continued vessel patency. All 5 patients had mean clinical follow-up of 8.4 months with no complications.
In our series, 3 of 29 procedures (10.3%) had procedural TIAs; however, only one of these procedures (3.4%) involved a patient who was initially neurologically asymptomatic. At long-term follow-up, 2 patients had occlusions of their treated vessels, one of which was asymptomatic (stented before the use of clopidogrel bisulfate). The other presented with a mild contralateral infarct, from which he made a full recovery. He had not received anticoagulation following the procedure, despite the recommendation of the neurointerventional team. A limitation of this study is the lack of a control group to compare the natural history of dissection in matched patients.
The natural history of carotid dissection with or without pseudoaneurysm is not well defined. Touze et al (44) retrospectively studied 71 patients with cervical artery dissection, among whom 35 had a total of 42 aneurysms (33 aneurysms of internal carotid arteries: 23 symptomatic and 10 asymptomatic). During a mean follow-up of >3 years, no patient had ischemic complications; most were treated with antiplatelet or anticoagulant therapy.
More recently, Kremer et al have prospectively studied the natural history of spontaneous dissection resulting in persistent stenosis or pseudoaneurysm (45). They compared a group of 46 patients with persistent severe stenosis or occlusion of the carotid artery with a group of 46 age- and latency-matched patients with transient stenosis (complete recanalization or <50% restenosis). With the exception of 3 cases with permanent severe stenosis or occlusion of the internal carotid artery, all patients presented with ischemic events. Antithrombotic therapy was given at the discretion of the treating physician; patients who received surgical, endovascular, or fibrinolytic therapy were excluded. Patients were followed annually with clinical examination and sonography. The group with persistent stenosis had a 0.7% annual risk of ipsilateral stroke and 1.4% risk of any stroke. The transient stenosis group had a 0.3% annual risk of ipsilateral stroke and 0.6% risk of any stroke. Although the risk of stroke was low in both groups, the risk of stroke in the persistent stenosis group was approximately double that of the transient group. These studies demonstrate that carotid dissections appear to have a relatively benign long-term course even in symptomatic patients.
Surgical treatment of carotid dissections is an alternative to angioplasty and stent placement. Surgery, however, is associated with high complication rates. Schievink et al reported a 9% overall postoperative stroke rate in 22 patients (12 symptomatic and 10 asymptomatic) treated with ligation (n = 5), resection of pseudoaneurysm and reconstruction of internal carotid artery (n = 13), and cervical-to-intracranial internal carotid artery bypass (n = 4) (11). Transient cranial nerve palsies were common after high cervical exposure (11 of 13 resections; 1 of 4 bypasses). Patients who underwent ligation did not experience ischemic complications or cranial nerve palsies. In the present study, there were also no postprocedure cranial nerve palsies. Muller et al reported a similar postoperative stroke rate of 10% in the treatment of 50 carotid dissections (12). Eighty percent of the patients underwent resection and vein graft placement. Fifty-eight percent experienced cranial nerve palsy, mostly transient. On long-term follow-up in both surgical series, no patients experienced an ischemic event referable to the treated lesion.
In light of the relatively benign long-term outcomes of most carotid dissection, it is important to proceed with caution when considering invasive therapy such as angioplasty and stent placement. The risks and benefits of medical, surgical, and endovascular treatments must be made on a patient-specific basis.
Our current practice is to treat symptomatic patients if they have stenosis and/or pseudoaneurysm. Restoration of a normal lumen diameter increases flow through the previously narrowed vessel and eliminates the relatively stagnant flow of the compressed and soon-to-be-obliterated pseudoaneurysm. The asymptomatic patient with either stenosis and/or pseudoaneurysm is counseled in light of ACAS, and these patients have chosen to be treated with stents.
Conclusion
Endovascular stent placement is the treatment of choice for patients who present acutely and fail medical therapy. It may also be appropriate in other select asymptomatic patients, especially because delayed neurologic deficits from dissection have been reported. Because clopidogrel bisulfate was not used in the 2 patients who returned with occlusion, the use of antiplatelet agents may be particularly important for long-term patency. In this series, angioplasty and stent placement were effective in relieving stenosis secondary to carotid dissection as well as in obliterating associated pseudoaneurysms. The technique was safe, with low rates of ischemic complications as demonstrated with long-term clinical and imaging follow-up.
References
- 1.Leys D, Lucas C, Gobert M, et al. Cervical artery dissections. Eur Neurol 1997;37:3–12 [DOI] [PubMed] [Google Scholar]
- 2.Lucas C, Moulin T, Deplanque D, et al. Stroke patterns of internal carotid artery dissection in 40 patients. Stroke 1998;29:2646–2648 [DOI] [PubMed] [Google Scholar]
- 3.Schievink WI. The treatment of spontaneous carotid and vertebral artery dissections. Curr Opin Cardiol 2000;15:316–321 [DOI] [PubMed] [Google Scholar]
- 4.Batnitzky S, Price HI, Holden RW, Franken EA Jr. Cervical internal carotid artery injuries due to blunt trauma. AJNR Am J Neuroradiol 1983;4:292–295 [PMC free article] [PubMed] [Google Scholar]
- 5.Brandt T, Caplan L. Spontaneous arterial dissection. Curr Treat Options Neurol 2001;3:463–469 [DOI] [PubMed] [Google Scholar]
- 6.Schievink WI. Spontaneous dissection of the carotid and vertebral arteries. N Engl J Med 2001;344:898–906 [DOI] [PubMed] [Google Scholar]
- 7.Biousse V, D’Anglejan-Chatillon J, Touboul PJ, et al. Time course of symptoms in extracranial carotid artery dissections: a series of 80 patients. Stroke 1995;26:235–239 [DOI] [PubMed] [Google Scholar]
- 8.Kalb R. Spontaneous dissection of the carotid and vertebral arteries. N Engl J Med 2001;345:467. [DOI] [PubMed] [Google Scholar]
- 9.Lyrer P, Engelter S. Antithrombotic drugs for carotid artery dissection. Cochrane Database Syst Rev 2003;CD000255. [DOI] [PubMed]
- 10.Engelter ST, Lyrer PA, Kirsch EC, Steck AJ. Long-term follow-up after extracranial internal carotid artery dissection. Eur Neurol 2000;44:199–204 [DOI] [PubMed] [Google Scholar]
- 11.Schievink WI, Piepgras DG, McCaffrey TV, Mokri B. Surgical treatment of extracranial internal carotid artery dissecting aneurysms. Neurosurgery 1994;35:809–815 [DOI] [PubMed] [Google Scholar]
- 12.Muller BT, Luther B, Hort W, et al. Surgical treatment of 50 carotid dissections: indications and results. J Vasc Surg 2000;31:980–988 [DOI] [PubMed] [Google Scholar]
- 13.Morris P. Interventional and endovascular therapy of the nervous system: a practical guide. New York: Springer-Verlag;2002
- 14.Malek AM, Higashida RT, Phatouros CC, et al. Endovascular management of extracranial carotid artery dissection achieved using stent angioplasty. AJNR Am J Neuroradiol 2000;21:1280–1292 [PMC free article] [PubMed] [Google Scholar]
- 15.Bejjani GK, Monsein LH, Laird JR, et al. Treatment of symptomatic cervical carotid dissections with endovascular stents. Neurosurgery 1999;44:755–60 [DOI] [PubMed] [Google Scholar]
- 16.Bush RL, Lin PH, Dodson TF, et al. Endoluminal stent placement and coil embolization for the management of carotid artery pseudoaneurysms. J Endovasc Ther 2001;8:53–61 [DOI] [PubMed] [Google Scholar]
- 17.Perez-Cruet MJ, Patwardhan RV, Mawad ME, Rose JE. Treatment of dissecting pseudoaneurysm of the cervical internal carotid artery using a wall stent and detachable coils: case report. Neurosurgery 1997;40:622–625 [DOI] [PubMed] [Google Scholar]
- 18.DeOcampo J, Brillman J, Levy DI. Stenting: a new approach to carotid dissection. J Neuroimaging 1997;7:187–190 [DOI] [PubMed] [Google Scholar]
- 19.Malek AM, Higashida RT, Halbach VV, et al. Patient presentation, angiographic features, and treatment of strangulation-induced bilateral dissection of the cervical internal carotid artery: report of three cases. J Neurosurg 2000;92:481–487 [DOI] [PubMed] [Google Scholar]
- 20.Redekop G, Marotta T, Weill A. Treatment of traumatic aneurysms and arteriovenous fistulas of the skull base by using endovascular stents. J Neurosurg 2001;95:412–419 [DOI] [PubMed] [Google Scholar]
- 21.Hong MK, Satler LF, Gallino R, Leon MB. Intravascular stenting as a definitive treatment of spontaneous carotid artery dissection. Am J Cardiol 1997;79:538. [DOI] [PubMed] [Google Scholar]
- 22.Klein GE, Szolar DH, Raith J, et al. Posttraumatic extracranial aneurysm of the internal carotid artery: combined endovascular treatment with coils and stents. AJNR Am J Neuroradiol 1997;18:1261–1264 [PMC free article] [PubMed] [Google Scholar]
- 23.Horowitz MB, Miller G 3rd, Meyer Y, et al. Use of intravascular stents in the treatment of internal carotid and extracranial vertebral artery pseudoaneurysms. AJNR Am J Neuroradiol 1996;17:693–696 [PMC free article] [PubMed] [Google Scholar]
- 24.Lee DH, Hur SH, Kim HG, et al. Treatment of internal carotid artery dissections with endovascular stent placement: report of two cases. Korean J Radiol 2001;2:52–56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Huang A, Baker DM, al-Kutoubi A, Mansfield AO. Endovascular stenting of internal carotid artery false aneurysm. Eur J Vasc Endovasc Surg 1996;12:375–377 [DOI] [PubMed] [Google Scholar]
- 26.Biggs KL, Chiou AC, Hagino RT, Klucznik RP. Endovascular repair of a spontaneous carotid artery dissection with carotid stent and coils. J Vasc Surg 2004;40:170–173 [DOI] [PubMed] [Google Scholar]
- 27.Pride GL Jr, Replogle RE, Rappard G, et al. Stent-coil treatment of a distal internal carotid artery dissecting pseudoaneurysm on a redundant loop by use of a flexible, dedicated nitinol intracranial stent. AJNR Am J Neuroradiol 2004;25:333–337 [PMC free article] [PubMed] [Google Scholar]
- 28.Liu AY, Paulsen RD, Marcellus ML, et al. Long-term outcomes after carotid stent placement treatment of carotid artery dissection. Neurosurgery 1999;45:1368–1373 [DOI] [PubMed] [Google Scholar]
- 29.Barnett HJ, Taylor DW, Eliasziw M, et al. Benefit of carotid endarterectomy in patients with symptomatic moderate or severe stenosis: North American Symptomatic Carotid Endarterectomy Trial Collaborators. N Engl J Med 1998;339:1415–1425 [DOI] [PubMed] [Google Scholar]
- 30.Executive Committee for the Asymptomatic Carotid Atherosclerosis Study. Executive Committee for the Asymptomatic Carotid Atherosclerosis Study: endarterectomy for asymptomatic carotid artery stenosis. JAMA 1995;273:1421–1428 [PubMed] [Google Scholar]
- 31.Fisher CM, Ojemann RG, Roberson GH. Spontaneous dissection of cervico-cerebral arteries. Can J Neurol Sci 1978;5:9–19 [PubMed] [Google Scholar]
- 32.Mokri B, Sundt TM Jr, Houser OW. Spontaneous internal carotid dissection, hemicrania, and Horner’s syndrome. Arch Neurol 1979;36:677–680 [DOI] [PubMed] [Google Scholar]
- 33.Hart RG, Easton JD. Dissections of cervical and cerebral arteries. Neurol Clin 1983;1:155–182 [PubMed] [Google Scholar]
- 34.Schievink WI, Mokri B, Whisnant JP. Internal carotid artery dissection in a community: Rochester, Minnesota, 1987–1992. Stroke 1993;24:1678–1680 [DOI] [PubMed] [Google Scholar]
- 35.Giroud M, Fayolle H, Andre N, et al. Incidence of internal carotid artery dissection in the community of Dijon. J Neurol Neurosurg Psychiatry 1994;57:1443–1443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Theron JG, Payelle GG, Coskun O, et al. Carotid artery stenosis: treatment with protected balloon angioplasty and stent placement. Radiology 1996;201:627–636 [DOI] [PubMed] [Google Scholar]
- 37.Bettmann MA, Katzen BT, Whisnant J, et al. Carotid stenting and angioplasty: a statement for healthcare professionals from the Councils on Cardiovascular Radiology, Stroke, Cardio-Thoracic and Vascular Surgery, Epidemiology and Prevention, and Clinical Cardiology, American Heart Association. Stroke 1998;29:336–338 [DOI] [PubMed] [Google Scholar]
- 38.White CJ, Gomez CR, Iyer SS, et al. Carotid stent placement for extracranial carotid artery disease: current state of the art. Catheter Cardiovasc Interv 2000;51:339–346 [DOI] [PubMed] [Google Scholar]
- 39.Wholey MH, Wholey M, Mathias K, et al. Global experience in cervical carotid artery stent placement. Catheter Cardiovasc Interv 2000;50:160–167 [DOI] [PubMed] [Google Scholar]
- 40.Vitek JJ, Roubin GS, Al-Mubarek N, New G, Iyer SS. Carotid artery stenting: technical considerations. AJNR Am J Neuroradiol 2000;21:1736–1743 [PMC free article] [PubMed] [Google Scholar]
- 41.Phatouros CC, Higashida RT, Malek AM, et al. Clinical use of stents for carotid artery disease. Neurol Med Chir (Tokyo) 1999;39:809–827 [DOI] [PubMed] [Google Scholar]
- 42.Yadav JS, Wholey MH, Kuntz RE, et al. Protected carotid artery stenting versus endarterectomy in high-risk patients. N Engl J Med 2004;351:1493–501 [DOI] [PubMed] [Google Scholar]
- 43.Kadkhodayan Y, Derdeyn CP, Cross DT, Moran CJ. Procedure complications of carotid angioplasty and stent placement without cerebral protection devices. Neurosurg Focus 2005;18:1–7 [DOI] [PubMed] [Google Scholar]
- 44.Touze E, Randoux B, Meary E, et al. Aneurysmal forms of cervical artery dissection: associated factors and outcome. Stroke 2001;32:418–423 [DOI] [PubMed] [Google Scholar]
- 45.Kremer C, Mosso M, Georgiadis D, et al. Carotid dissection with permanent and transient occlusion or severe stenosis: long-term outcome. Neurology 2003;60:271–275 [DOI] [PubMed] [Google Scholar]