Abstract
BACKGROUND AND PURPOSE: Adjacent fracture formation after percutaneous vertebroplasty has been reported in literature. The purpose of this study was to determine whether intervertebral disk extravasation is related to adjacent fracture formation in low-volume cement-filling vertebroplasty.
METHODS: A retrospective analysis of 308 patients having vertebroplasty was undertaken. Anteroposterior and lateral procedural fluoroscopy radiographs were analyzed for mild, moderate, or severe disk extravasation. Symptomatic refracture location relative to the presence or absence of extravasation was analyzed on follow-up fluoroscopy radiographs.
RESULTS: Of the 308 patients in the study, 81 patients had disk extravasation at a total of 85 vertebral levels; 40 levels had mild extravasation, 38 levels had moderate extravasation, and 7 had severe extravasation. Of the 40 levels with mild extravasation, 6 new adjacent fractures occurred next to the disk leakage. Of the 38 with moderate extravasation, 6 new adjacent fractures occurred. Of the 7 levels of severe extravasation, only one new adjacent fracture occurred. Hence, a total of 13 adjacent fractures occurred next to disk extravasation; 13 nonadjacent fractures also occurred in the patients with disk extravasation. In the patients without disk extravasation, 28 adjacent and 24 nonadjacent subsequent fractures occurred. The average available cement volumes injected into vertebral bodies causing disk leakage ranged from 4.78 to 5.60 mL.
CONCLUSIONS: With low-volume cement-filling percutaneous vertebroplasty, we cannot conclude (level of significance α = .05) that for patients who have a new fracture there is significance between the location of the fracture and the occurrence of disk extravasation.
Vertebral body compression fractures usually result in acute pain that is frequently disabling, resulting in decreased quality of life and increased medical costs (1–5). Traditionally, conservative treatment of vertebral fractures included analgesics, bed rest, bracing, and antiosteoporitic medications (6–10). Recently, percutaneous vertebroplasty has been used to treat painful vertebral fractures secondary to osteoporosis, which is refractory to medical therapy, benign or malignant tumors, or osteonecrosis (11). Most of the patients undergoing this procedure have vertebral compression fractures secondary to osteoporosis. Degree of osteoporosis, cement volume, disk extravasation, and level of activity are factors in adjacent fracture formation after vertebroplasty (12). Adjacent fracture formation after percutaneous vertebroplasty has been reported to occur in as many as two-thirds of new fractures, with an average cement volume of 9.14 mL (13). The purpose of this study was to analyze adjacent fracture formation in cases of disk extravasation after low-volume cement-filling percutaneous vertebroplasty.
Methods
A retrospective analysis reviewed 308 patients (average age, 76.2 years) having vertebroplasties performed from August 1999 to August 2004. Intradiskal extravasation was noted on biplanar procedural fluoroscopy radiographs. Disk extravasation occurred in 81 of the 308 patients. Of these 81 patients, 2 had breast cancer, 2 had lung cancer, one had multiple myeloma, and 76 had osteoporosis. For level treated with vertebroplasty, anteroposterior (AP) and lateral fluoroscopy radiographs were taken. From these radiographs, the degree of extravasation was classified into minor, moderate, or severe. Mild disk extravasation was quantified when cement leakage was less than one-third of the adjacent nonfractured vertebral body on both AP and lateral fluoroscopy procedural radiographs. This method of disk extravasation quantification accounts for the axial measurements in the x and y coordinates. The height (or z coordinate) was not accounted for in the classification of the degree of disk extravasation because the axial directions of a vertebral disk are greater than the height. Figure 1 illustrates a line drawing for the measurements of disk extravasation. Similarly, moderate disk extravasation was defined when cement leakage occupied from one-third to two-thirds of the adjacent nonfractured vertebral body on both AP and lateral procedural radiographic views. Severe extravasation was defined when cement leakage occupied more than two-thirds on AP and lateral views. Examples of mild, moderate, and severe extravasation can be viewed in Figs 2, 3, and 4.
Fig 1.
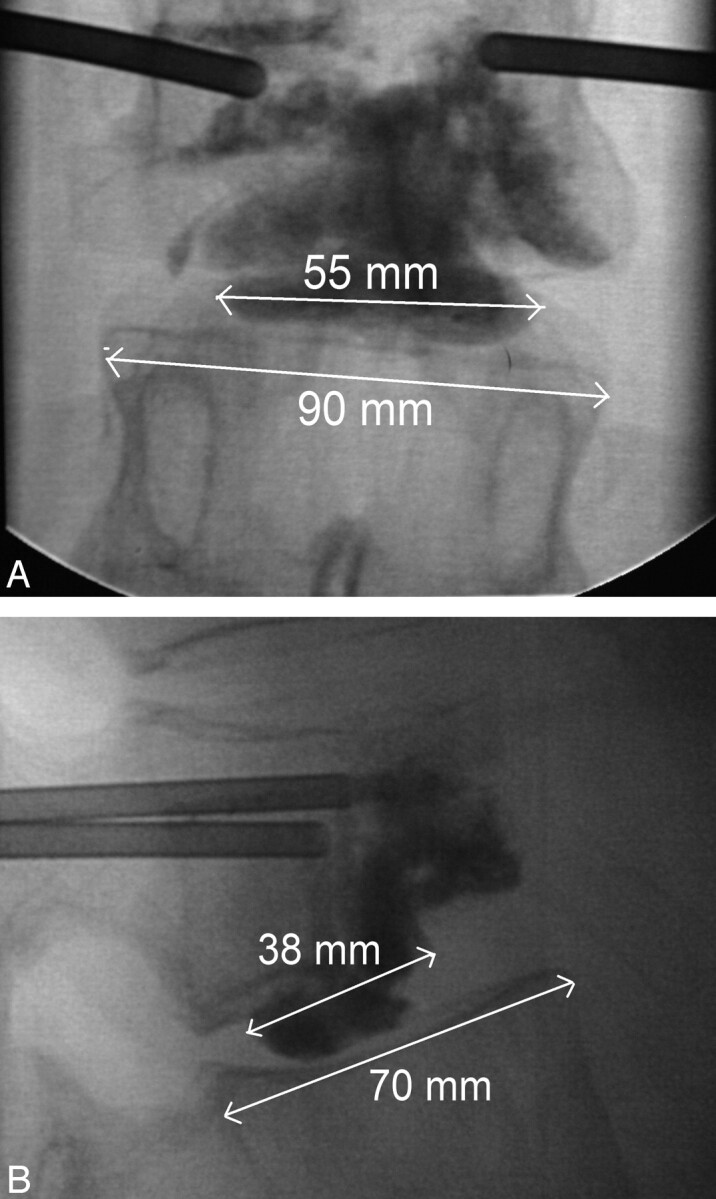
A, Line drawing on AP fluoroscopic view for calculation of moderate extravasation; 55 mm/90 mm is less than two-thirds the adjacent nonfractured vertebral body dimensions (figure not to scale).
B, Line drawing on lateral fluoroscopic view for calculation of moderate extravasation; 38 mm/70 mm is less than two-thirds the adjacent nonfractured vertebral body dimensions (figure not to scale).
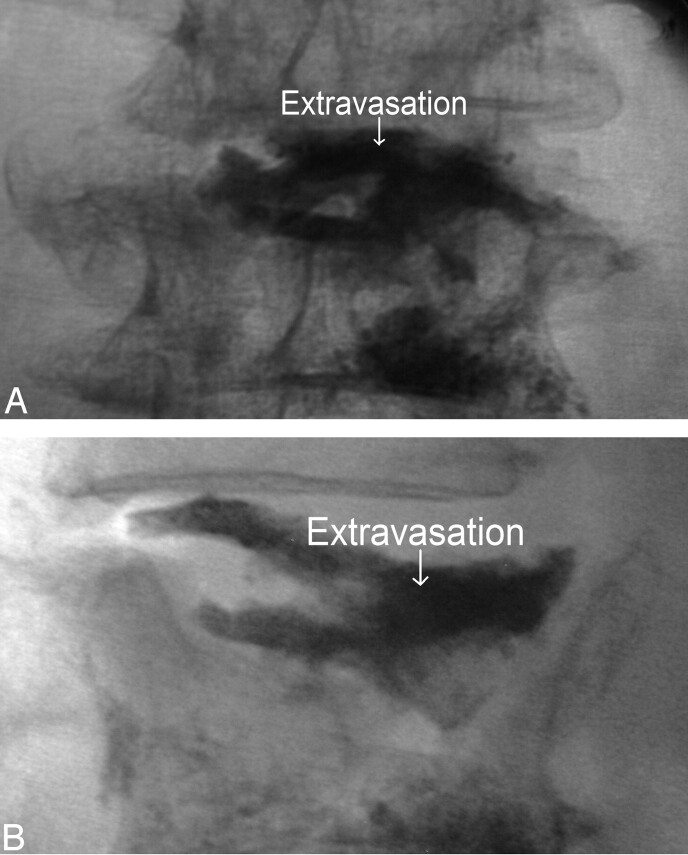
Fig 2.

A, AP fluoroscopic view of mild extravasation.
B, Lateral fluoroscopic view of mild extravasation.
Fig 3.

A, AP fluoroscopic view of moderate extravasation.
B, Lateral fluoroscopic view of moderate extravasation.
Fig 4.
A, AP fluoroscopic view of severe extravasation.
B, Lateral fluoroscopic view of severe extravasation.
Follow-up conventional radiographs, CT, or MR were taken only in patients who experienced continued or new back pain. Patients with disk extravasation between 2 levels that were treated at the same time were excluded because potential fracture sites were already treated. Patients with disk extravasation next to chronic fractures or previously treated levels were also excluded.
Typical cases involved elderly women with a short history of back pain after falling or performing a normal activity of daily living. The back pain was usually described as 10 of 10 and was associated with significant decrease in mobility and quality of life. After ordering conventional radiographs to detect vertebral fracture, the primary care physician referred the patient to the radiology clinic. A thorough history and physical was performed by our interventional radiologists, focusing on spinal point tenderness and neurologic function. Further imaging usually involved MR images to detect the presence of acute fracture and to determine whether retropulsion was present. After vertebroplasty, patients usually experienced significant pain relief within the first 2 weeks. If back pain recurred, the patient was asked to return to the radiology clinic for further evaluation.
Our group of 3 interventional radiologists performed the vertebroplasty procedures by using the same technique. Sedation, pain control, and prophylactic antibiotics were provided by the anesthesiology department. Bupivacaine was used to anesthetize the skin and soft tissues to and including the periosteum over each fractured vertebra. An 11- or 13-gauge trocar was then advanced through the pedicle under biplanar fluoroscopy guidance into the anterior most portion of the vertebral body. Codman cranioplastic polymethacrylate (Depuy CMW, Blackpool, UK), mixed with sterile barium sulfate (Bryan Corporation, Woburn, MA) and vancomycin, was delivered by using the EZflow Cement Delivery System (Paralax, Sunnyvale, CA) during the period 1999 to mid-2002. During the period mid-2002 to present, Simplex-P polymethylmethacrylate, sterile barium sulfate, and vancomycin were injected by using the Percutaneous Cement Delivery System (Stryker-Howmedica Osteonics, Kalamazoo, MI). Bone cement was injected into the central anterior intravertebral space until adequate filling was achieved without extravasation. If cross-filling was inadequate, a bipedicular approach was then performed. If any paraspinal or interdisk leakage of cement occurred, the injection was temporarily halted to allow hardening of cement and reattempted. If any epidural extravasation occurred, the injection phase was terminated. All patients were observed in the recovery room for 2 hours before being discharged to their previous disposition.
Follow-up phone calls were made after 1–2 days, 1 week, 2 weeks, 1 month, 3 months, and 6 months. After 6 months, all patients were asked to contact the radiology clinic if new pain occurred. For those patients with recurrent pain, follow-up was extended to 1 year or longer. Patients directly contacted the radiology clinic in the event of any continued or new pain. All follow-up imaging ordered by primary care physicians for subsequent back pain after initial procedure was performed at our community hospital. Patients who refractured after vertebroplasty were usually symptomatic. These patients typically presented within the first several weeks after their procedure with severe back pain associated with significant decrease in mobility and quality of life. Physical examination focused on spinal point tenderness and neurologic function. Further imaging usually involved MR images to detect the presence of fracture and presence of retropulsion. Follow-up radiographs were available for 59 of the 81 patients with disk extravasation. The average time for subsequent imaging was 36.5 weeks after the initial procedure. Patients not requiring further imaging did not complain of back pain during follow-up calls and were satisfied with the procedure.
Statistical analysis was performed by the Wright State University Statistical Consulting Center.
Results
Biplanar fluoroscopy radiographs for 313 patients were analyzed for evidence of extravasation. Five patients were excluded because extravasation occurred at sites adjacent to chronic fractures, previously treated fractures, or between 2 levels that were treated during the same vertebroplasty session. Of the remaining 308 patients, 81 had disk extravasation in a total of 85 vertebral disks. (Four of these patients had extravasation in 2 disk spaces.) In 227 patients, there was no evidence of extravasation at any of their vertebroplasty sessions.
Of the 85 levels with extravasation, 40 levels had mild extravasation, 38 had moderate extravasation, and 7 had severe leakage. Cement volumes were available for most of the levels with extravasation. Cement volumes were available for 72.5% of the mild extravasation levels, 84.2% of the moderate extravasation levels, and 71.4% of the severe extravasation levels. Cement volumes were reported in 73.6% of levels without extravasation. Available average cement volumes (in cubic centimeters) for extravasation are 4.96 ± 2.44 (mild, 4.78 ± 2.10; moderate, 4.89 ± 2.71; severe, 5.60 ± 2.51) and for no extravasation are 5.26 ± 2.48. The number of subsequent fractures next to disk extravasation are as follows: mild extravasation, 40 levels (6 adjacent and 7 nonadjacent fractures); moderate extravasation, 38 levels (6 adjacent and 5 nonajacent fractures); severe, 7 levels (1 adjacent and 1 nonadjacent fracture).
The average time for 11 of the 13 patients with subsequent adjacent fractures after disk extravasation was 6.3 weeks (2 of the 13 patients refractured after 2 years). Only 3 of these 13 patients had bone mineral densities (BMDs). The average t score was −2.33 in these patients. The number of adjacent and nonadjacent fractures with levels with or without extravasation for the 308 patients in the study were 13 adjacent and 13 nonadjacent fractures for patients with extravasation and 28 adjacent and 24 nonadjacent fractures for patients without extravasation (χ2 = 0.1028; P = .7485, df = 1).
Three of the 13 nonadjacent fractures with extravasation were actually adjacent to the original vertebral body causing the leakage, but not next to the disk leakage.
Discussion
Adjacent fracture formation after percutaneous vertebroplasty is a topic of concern in the literature. In vitro studies have revealed that cement-filled bone is 36 times stronger than spinal cancellous bone (14). In a computational and experimental study, Baroud et al found that cement in injected vertebral bodies reduces the endplate physiologic inward bulge, causing a net “pillar effect” (14). This results in a marked increase in the pressure within the intervertebral disk, which is further transferred to the adjacent disk. Baroud et al stated that stiffness from the bone cement increases the risk of adjacent vertebral fractures. It is postulated that stiffness can be reduced by decreasing the amount of cement injected—hence, adjacent fracture formation also may be decreased (14). In our series of patients, only 13 of the 85 levels with extravasation experienced a new adjacent fracture. In addition, 13 subsequent nonadjacent fractures occurred in the levels with disk extravasation. In the Results section, the distribution of new fractures (whether adjacent or nonadjacent) was analyzed in correlation with the presence or absence of disk extravasation for all 308 patients. At a level of significance α = 0.05, we cannot conclude that for patients who have a new fracture there is a significant association between the location of the fracture and the occurrence of extravasation with low-volume filling.
By using the biomechanical analysis of vertebroplasty, we believe the most important factors for a vertebral fracture adjacent to disk extravasation are the degree of osteoporosis, the volume of cement injected, and level of postprocedural activity. Only 3 of the 13 patients with adjacent fractures next to disk extravasation had BMDs. The average t score was −2.33 in these patients. Hence, no definite conclusions can be drawn from so few BMDs. It has been found that given a prevalent osteoporotic fracture treated with conservative medical therapy, the chance of having an incident fracture within one year is 21.9% (15). Elsewhere, we found similar rates of incident fractures within 1 year in patients having prevalent acute/subacute osteoporotic fractures treated with vertebroplasty (16).
Our technique of cement filling involved halting injection when disk extravasation was observed during the procedure. Injection was either resumed once the extravasation hardened or a bipedicular injection was then attempted. The average volume for the mild, moderate, and severe extravasation groups ranged from 4.78 to 5.60 mL. Hence, low-volume cement injection was used in these groups. Ex vivo studies on osteoporotic cadavers revealed that vertebral body strength is restored in all regions of the spine with 2 mL of Simplex 20 and stiffness is restored with 4 mL in the thoracic and lumbar areas, whereas the thoracolumbar region requires 8 mL (17). With such low-volume filling and halting of injection once extravasation occurred, we feel that the degree of osteoporosis was the overwhelming factor of fracture formation next to disk extravasation.
A study by Lin et al revealed that cement leakage into the disk during vertebroplasty increases the risk of subsequent fracture of adjacent vertebral bodies (12). In this study of 38 patients having vertebroplasty, 14 refractured. Ten of the 14 patients had fractures at adjacent vertebral bodies next to the disk extravasation (12). This study clearly demonstrates that adjacent fracture formation is linked to disk extravasation. In our study of 308 patients, only 13 of the 85 levels with extravasation had a fracture at the adjacent vertebral level. We feel that most of our 13 vertebral fractures next to the disk extravasation were primarily due to the natural progression of osteoporosis. The difference between the high rate of adjacent fracture formation in the study by Lin et al and our analysis probably is related to technique of filling and amount of cement injected. With low-volume filling, less extravasation is likely to occur. In addition, our data reveal that the net “pillar effect” described by Baroud et al seems to decrease by lower cement injection, because our rate of adjacent fracture formation was less than in the study by Lin et al.
A limitation to this study is that volume of disk extravasation was not quantified. We determined the degree of extravasation by calculating the percentage of adjacent vertebral body in both the AP and lateral fluoroscopy views from the original procedure in which the extravasation occurred. Most of the biplanar fluoroscopy radiographs for the 85 levels with disk extravasation revealed minor to moderate extravasation; however, 7 levels had severe extravasation and only one adjacent fracture occurred with this extravasation group. With more cement in the intervertebral disks, it is likely that there is more increased pressure within the disks from the “pillar effect.” This, along with increased physical activity postprocedurally, may increase the risk for adjacent fracture. Further studies correlating quantity of extravasation and level of activity with adjacent fracture formation would be helpful in understanding the consequences of cement leakage.
Another limitation to our study is that only symptomatic patients were reimaged. Ideally, all patients would have follow-up radiographs at a specified time after the procedure. In clinical practice, however, this is not feasible. Only patients who complained of significant pain were further imaged. Hence, patients with asymptomatic fractures may have been missed. We feel that, even though asymptomatic fractures are important, if they do not cause any pain or decreased activities of daily living, they should not be treated. Fifty-nine of the 81 patients with disk extravasation had subsequent imaging. The average time imaging was taken for these 59 patients after the initial vertebroplasty was 36.5 weeks. The average time for 11 of the 13 patients with subsequent adjacent fractures after disk extravasation was 6.3 weeks. Hence, most refractures occurred several weeks after the initial procedure. For the patients who did not have further imaging, they usually had significant improvement in pain during follow-up phone calls and were satisfied with the procedure. Our follow-up was similar to that of Lin et al.
Conclusions
From our series of patients, subsequent adjacent and nonadjacent fractures after percutaneous vertebroplasty occur roughly equally for each of the disk extravasation and the no disk extravasation groups. Hence, with low-volume cement-filling percutaneous vertebroplasty, we cannot conclude (α = 0.05) that there is a significant relationship between intradiskal extravasation and location of subsequent fracture. In general, our criteria for cement filling involve trying to obtain a column-like effect within the vertebral body. When injecting bone cement on the AP fluoroscopic view, we try to produce cement filling in the lateral third of the vertebral body or cement filling in the central and lateral third on either side of the vertebral body. On the lateral fluoroscopic view, these columns of cement should occupy the anterior two-thirds of the vertebral body. We feel that the goal of vertebroplasty should be to use the least amount of cement to provide sufficient strength and stiffness as discussed by Belkoff et al, because the bone cement is more attenuated than the osteoporotic bone (17). We usually try not to fill >4 mL in the thoracic levels and 6 mL in the lumbar regions (dependent on morphology of the vertebral fracture), deferring to the principle “less is more.” The goal of vertebroplasty is not to overfill, but to provide the critical minimal volume needed for mechanical support. If a subsequent fracture occurs at a level adjacent to intradiskal extravasation from a vertebral body having low-volume cement filling, the new fracture is most likely secondary to the underlying degree of osteoporosis.
References
- 1.Evans AJ, Jensen ME, Kip KE, et al. Vertebral compression fractures: pain reduction and improvement in functional mobility after percutaneous polymethacrylate vertebroplasty: retrospective report of 245 cases. Radiology 2003;226:366–372 [DOI] [PubMed] [Google Scholar]
- 2.Melton LJ III. Epidemiology of spinal osteoporosis. Spine 1997;22(suppl 24):2S–11S [DOI] [PubMed] [Google Scholar]
- 3.Cooper C, Atkinson EJ, O’Fallon WM, Melton LJ III. Incidence of clinically diagnosed vertebral fractures: a population-based study in Rochester, Minnesota, 1985–1989. J Bone Miner Res 1992;7:221–227 [DOI] [PubMed] [Google Scholar]
- 4.Lykes KW, Gold DT, Shipp KM, et al. Association of osteoporotic vertebral compression fractures with impaired functional status. Am J Med 1993;94:595–601 [DOI] [PubMed] [Google Scholar]
- 5.Ross PD, Davis JW, Epstein RS, Wasnich RD. Pain and disability associated with new vertebral fractures and other spinal conditions. Am J Epidemiol 1994;47:231–239 [DOI] [PubMed] [Google Scholar]
- 6.Phillips FM, Pfeifer BA, Lieberman IH, et al. Minimally invasive treatments of osteoporotic vertebral compression fractures: vertebroplasty and kyphoplasty. AAOS Instructional Course Lectures 2003;52:559–567 [PubMed] [Google Scholar]
- 7.Rapado A. General management of vertebral fractures. Bone 1996;18(suppl 13):191S–196S [DOI] [PubMed] [Google Scholar]
- 8.Lukert BP. Vertebral compression fractures: how to manage pain, avoid disability. Geriatrics 1994;49:22–26 [PubMed] [Google Scholar]
- 9.Eck JC, Hodges SD, Humphreys SC. Vertebroplasty: a new treatment strategy for osteoporotic compression fractures. Am J Orthop 2002;31:123–128 [PubMed] [Google Scholar]
- 10.Meunier PJ, Delmas PD, Eastell R, et al. Diagnosis and management of osteoporosis in postmenopausal women: clinical guidelines: International Committee for Osteoporosis Clinical Guidelines. Clin Ther 1999;21:1025–1044 [DOI] [PubMed] [Google Scholar]
- 11.McGraw JK, Cardella J, Barr JD, et al. Society of interventional radiology quality improvement guidelines for percutaneous vertebroplasty. J Vasc Interv Radiol 2003;14:827–831 [DOI] [PubMed] [Google Scholar]
- 12.Lin EP, Ekholm S, Hiwatashi A, Westesson P. Vertebroplasty: cement leakage into the disk increases the risk of new fracture of adjacent vertebral body. AJNR Am J Neuroradiol 2004;25:175–80 [PMC free article] [PubMed] [Google Scholar]
- 13.Uppin AA, Hirsch JA, Centenera LV, et al. Occurrence of new vertebral body fracture after percutaneous vertebroplasty in patients with osteoporosis. Radiol 2003;226:119–124 [DOI] [PubMed] [Google Scholar]
- 14.Baroud G, Heini P, Nemes J, et al. Biomechanical explanation of adjacent fractures following vertebroplasty. Radiology 2003;229:606–608 [DOI] [PubMed] [Google Scholar]
- 15.Lindsay R, Silverman S, Cooper C, et al. Risk of new vertebral fracture in the year following a fracture. JAMA 2001;285:320–323 [DOI] [PubMed] [Google Scholar]
- 16.Syed MI, Patel NA, Jan S, et al. New symptomatic vertebral compression fractures within a year following vertebroplasty in osteoporotic women. AJNR Am J Neuroradiol 2005;26:1601–1604 [PMC free article] [PubMed] [Google Scholar]
- 17.Belkoff SM, Mathis JM, Jasper LE, Deramond H. The biomechanics of vertebroplasty: the effect of cement volume on mechanical behavior. Spine 2001;26:1537–1541 [DOI] [PubMed] [Google Scholar]