Abstract
Summary: We report the case of a patient with Fahr disease presenting with schizophrenia-like psychosis for whom a technetium Tc99 methyl cysteinate dimmer brain study was used to evaluate regional blood flow. A brain single photon-emission CT study showed increased cerebral blood flow to the bilateral temporal lobes. Such perfusion abnormalities may reflect psychotic symptoms, including auditory hallucinations and delusions, which suggests a disruption of the cortico-subcortical neural circuits in psychosis.
Idiopathic calcification of the basal ganglia (ICBG), also known as Fahr disease, is a rare neurologic disorder of unknown etiology characterized by neuropsychiatric abnormalities, Parkinsonian or choreoathetotic-type movement disturbance, and extensive symmetrical calcification of the basal ganglia and dentate nuclei in the cerebellum. These symptoms cannot be explained by any particular disorder of the calcium phosphorus metabolism or other diseases.
Dementia is a well-recognized neuropsychiatric manifestation of ICBG that is manifested as memory disturbances, deterioration of intellectual function, and a slowing of cognitive processes. In addition, a schizophrenia-like psychosis characterized by paranoia, hallucinations, and delusions has been reported (1). The pathophysiology of psychosis in ICBG remains unknown, though previous studies have found a decreased cerebral blood flow matching the distribution of calcification or decreased perfusion in the cortex, which may reflect secondary deficits due to calcification (2–4).
In the present study, we report the case of a patient with Fahr disease presenting with a schizophrenia-like psychosis for whom a technetium Tc99 methyl cysteinate dimmer (Tc99m-ECD) brain study was used to evaluate cerebral blood flow.
Case Report
A 32-year-old, right-handed woman was referred from a local hospital for an evaluation of schizophrenia-like psychosis and brain CT abnormalities that revealed pronounced symmetrical calcifications in the basal ganglia and dentate nuclei of the cerebellum. There were no special notes in her family history, though she was reported to be obsessive and inactive since childhood. The patient had finished a school for domestic training with poor grades following junior high school graduation and later acquired a driving license. She married at 25 years of age and was a housewife. At 31 years of age, the patient became suspicious and developed unsubstantiated ideas of her neighborhood, which progressed to prominent auditory verbal hallucinations, disorganized speech, and delusions of persecution.
At the time of admission to our hospital, the patient was alert and oriented, though her face was expressionless and apathetic in appearance. Disorganized and obsessive behavior along with emotional inconsistencies were seen—ie, she was reported to fall to her knees to ask for pardon without reason, seek confirmation signatures regarding trivial matters by using a memo pad, and weep suddenly. Auditory verbal hallucinations and delusions were also in evidence. For example, she often said that she had received revelations about her relative’s death. A physical examination showed that she was well developed, with no deformities or Albright osteodystrophy, and vital signs were within normal limits.
On a neurologic examination, extrapyramidal signs were evidenced by micrographia, cogwheel rigidity in the arms, bradykinesia, and a Parkinsonian gait, whereas cerebellar signs were also evidenced by results of a finger-nose test and hand pronation supination test. Cranial nerve function, motor strength, sensation, and reflexes were intact.
Laboratory tests, including serum calcium, phosphorus, and parathyroid hormone (PTH) levels, were within normal limits (Ca 8.8 mg/day [Alb 4.0 g/dL], Ip 4.0 m g/dL, intact-PTH 24 pg/mL, high-sensitivity PTH 290 pg/mL). In addition, a CSF sample was normal, electrocardiogram findings were within a normal range, an electroencephalographic examination showed no focal abnormalities, and conventional radiographic images of the hands and chest were normal. Results of a Wechsler Adult Intelligence Scale-Revised emanation showed a full-scale intelligence quotient (IQ) of 43, verbal IQ of 50, and performance IQ of 45.
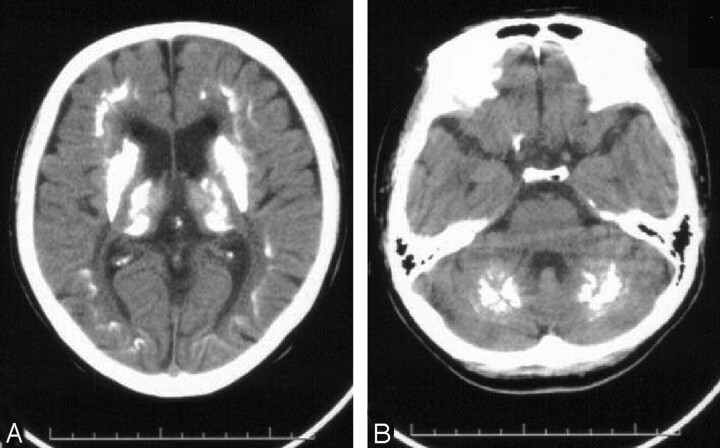
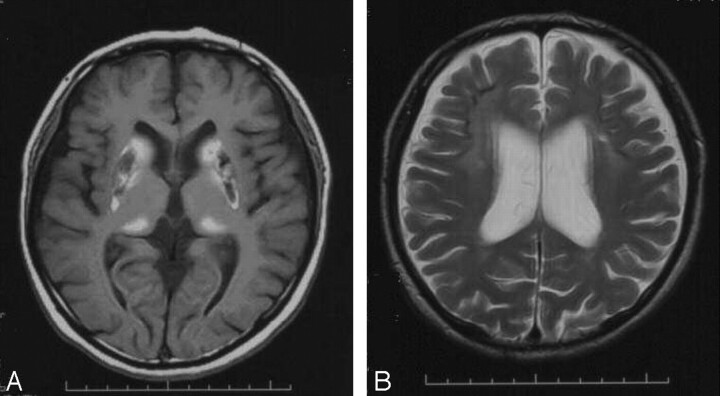
A neuropsychologic evaluation revealed perseveration and inattention, though aphasia, apraxia, and agnosia were not evident. A CT scan revealed attenuated calcification of the basal ganglia, thalamic nuclei, and cerebral and cerebellar white matter, as well as atrophy of the frontal lobe (Fig 1). Axial T1-weighted MR images showed a hyperintense area in the bilateral basal ganglia and thalami (Fig 2A), whereas axial T2-weighted MR images showed a hypointense area in the bilateral basal ganglia and thalami and a hyperintense periventricular area (Fig 2B).
Fig 1.
CT scan showing symmetrical calcifications in the basal ganglia and thalamic nuclei, as well as in the cerebral and cerebellar white matter.
Fig 2.
A, Axial T1-weighted MR images showing hyperintense areas in the bilateral basal ganglia and thalami.
B, Axial T2-weighted MR images showing a hyperintense area in the periventricular region.
Secondary changes due to the calcifications or gliosis were considered. Calcified lesions of the dentate nuclei of the cerebellum were not shown in MR images. Single photon-emission CT (SPECT) scintigraphy was performed after the patient had received haloperidol for about 4 weeks (8 mg/day), followed by 4 weeks of risperidone (4 mg/day). At that time, she still showed delusional and disorganized behavior, though auditory hallucinations could not be self-reported because of disorganization. The patient was injected with 600 MBq (16 mCi) of Tc99m-ECD 5 minutes before scanning.
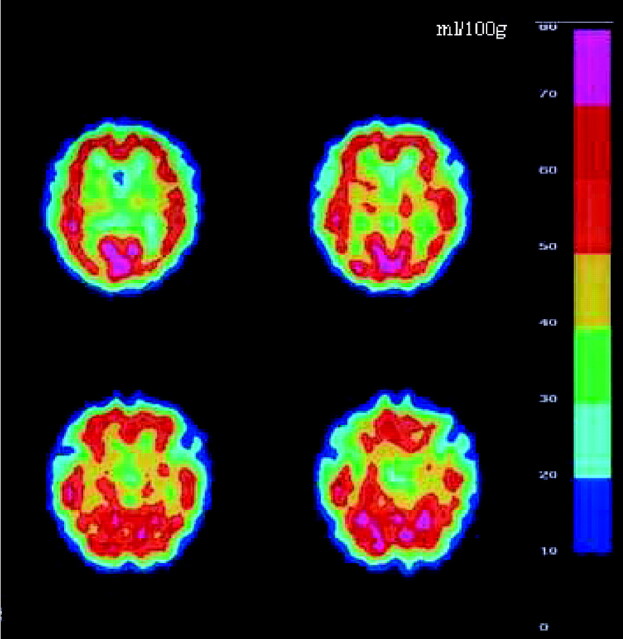
Scanning was performed by using a dual-head gamma camera (GE Yokokawa Millennium VG), with the acquisition parameters set at 120 projections recorded in step-and-shoot mode over a 360° rotation arch (each head acquired 60 projections). The angular step was 3° and the frame time was 17 seconds per step, whereas the acquisition matrix was 64 × 64 and zoom set at 2.2. All projection data were prefiltered through a Butterworth filter (cutoff at 0.5), which resulted in axial image sections sized at 64 × 64 × 8 mm. SPECT images showed increased cerebral blood flow in the bilateral lateral temporal lobes and decreased cerebral blood flow in the basal ganglia (Fig 3).
Fig 3.
Tc99m-ECD brain SPECT findings showing increased radiotracer uptake in the lateral temporal lobes, especially in the right side, and decreased uptake in the basal ganglia.
About 4 weeks later, the auditory hallucinations and delusions disappeared. The patient was discharged from our hospital and treated on an outpatient basis with low-dose risperidone.
Discussion
We treated a patient with Fahr disease who presented with a schizophrenia-like psychosis. CT and MR imaging findings revealed a bilateral calcification of the putamen and globus pallidus consistent with Fahr disease, along with frontal brain atrophy.
Hypoparathyroidism, pseudohypoparathyroidism, and hyperparathyroidism were denied on the basis of normal levels of serum calcium and phosphorus metabolism and lack of Albright osteodystrophy. Calcifications following congenital, infectious, traumatic, ischemic, neoplastic, vascular, and toxic brain insults also were not seen. The patient was able to acquire a driving license at 20 years of age. On the assumption that her obsessional and introverted personality was associated with the disease, calcification may have existed at an early age, which led to the development of progressive dementia.
Presenile cortical dementia with Fahr-type calcification can be diagnosed from the presence of diffuse neurofibrillary tangles with calcification (DNTC) (5). In the present case, DNTC was unlikely, because of the early-stage onset and lack of temporal lobe atrophy. Brain SPECT images were acquired when the patient was showing delusion, auditory hallucinations, and deterioration of intellectual function, and previous studies have reported decreased perfusion abnormalities in patients with dementia. Smith et al (3) reported a patient with Fahr disease who showed a perfusion deficit in the basal ganglia, whereas Uygur et al (4) described a patient with Fahr disease who had decreased blood flow in the basal ganglia and frontoparietal cortex. The latter patient was 43 years of age and showed dementia, as well as cerebellar and basal ganglia dysfunction. Further, Hempel et al (2) reported a 25-year-old patient with Fahr disease who presented with frontal lobe syndrome and dementia. In that case, reduced glucose uptake in positron-emission tomographic images was not restricted to the basal ganglia, but also involved the frontal, temporal, and parietal cortices. Others have reported cases with hypoperfusion in both thalami (6) and low metabolic changes of the corpus striatum and posterior cingulate (7). In addition, previous studies have found perfusion deficits in the basal ganglia matching the distribution of calcifications in the cortex that may reflect secondary deficits due to calcifications of the basal ganglia. To the best of our knowledge, hyperperfusion in the lateral temporal lobe cortex has not been reported in a patient with Fahr disease.
Several neuroimaging studies have detected hyperactivation in the temporal region along with auditory hallucinations in schizophrenic patients. A magnet-encephalography study (8) demonstrated left superior temporal cortex activations including the auditory area, suggesting that auditory hallucinations reflect an abnormal activation of the auditory pathways. Activation, including the bilateral temporal region, was also detected in a functional MR imaging study (9), whereas, recently, Andreasen et al (10) proposed that a disruption in the cortical-thalamic-cerebellar-cortical circuit leads to a disconnection syndrome, termed “cognitive dysmetria,” and impairment in this neural circuit produces diverse symptoms of schizophrenia.
The present findings suggest that the basal ganglia impairment in ICBG led to abnormal hyperactivity in the cortex mediated by the cortico-subcortical neural network, which generated psychotic symptoms. Although we attempted to demonstrate regional cerebral blood flow (rCBF) findings associated with hallucinatory experiences or delusions, there are limitations to the design of our study. In the present patient, haloperidol was administered first for about 4 weeks, followed by risperidone for another 4 weeks. The rCBF evaluation was performed under the use of antipsychotic medications and the patient was unable to self-report auditory hallucinations; however, disorganized behavior and delusions were identified at the time of the SPECT examination. The increase in rCBF in the lateral temporal cortex may have reflected her pathologic experiences, including the auditory hallucinations.
Neuroleptics are considered to inhibit cortex activities. One SPECT study of schizophrenia patients found that improvements after risperidone treatment were associated with a decrease in frontal and temporal activities, as well as a reduction in rCBF in the entire cortical area (11). The rCBF increase in the lateral temporal cortex in the present patient could not be explained by the effects of neuroleptics, though it may have reflected hyperactivation in this area that was related to pathologic experiences, such as the delusions or auditory hallucinations.
Conclusion
We treated a patient with Fahr disease who presented a schizophrenia-like psychosis. A brain SPECT study showed increased blood flow in the bilateral temporal lobes. The perfusion abnormalities may have reflected hyperactivation in the cortex related to auditory hallucinations or delusions and supports the theory that a disruption of the cortico-subcortical neural circuits produces psychotic symptoms.
References
- 1.Cummings JL, Gosenfeld LF, Houlihan JP, et al. Neuropsychiatric disturbances associated with idiopathic calcification of basal ganglia. Biol Psychiatry 1983;18:591–601 [PubMed] [Google Scholar]
- 2.Hempel A, Henze M, Berghoff C, et al. PET findings and neuropsychological deficits in a case of Fahr’s disease. Psychiatry Res 2001;108:133–140 [DOI] [PubMed] [Google Scholar]
- 3.Smith FW, Gemmell HG, Sharp PF, Besson JAO. Technetium-99m HM PAO imaging in patients with basal ganglia disease. Br J Radiol 1988;61:914–920 [DOI] [PubMed] [Google Scholar]
- 4.Uygur In GA, Liu Y, Hellman RS, et al. Evaluation of regional cerebral blood flow in massive intracerebral calcifications. J Nucl Med 1995;36:610–612 [PubMed] [Google Scholar]
- 5.Kosaka K. A diffuse neurofibrillary tangles with calcification: a new presenile dementia. J Neurol Neurosurg Psychiatry 1994;57:594–596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ogi S, Fukumitsu N, Tsuchida D, et al. Imaging of bilateral striopallidodentate calcinosis. Clin Nucl Med 2002;27:721–724 [DOI] [PubMed] [Google Scholar]
- 7.Le Ber I, Marie RM, Lalevee C, et al. Familial idiopathic striato-pallido-dentate calcifications: clinical and brain imaging study in a family. Rev Neurol (Paris)2003;159:43–49 [PubMed] [Google Scholar]
- 8.Ishii R, Shinosaki K, Ikejiri Y, et al. Theta rhythm increases in left superior temporal cortex during auditory hallucinations in schizophrenia: a case report. Neuroreport 2000;11:3283–3287 [DOI] [PubMed] [Google Scholar]
- 9.Lennox BR, Park SB, Medley I, et al. The functional anatomy of auditory hallucinations in schizophrenia. Psychiatry Res 2000;100:13–20 [DOI] [PubMed] [Google Scholar]
- 10.Andreasen NC, Nopoulos P, O’Leary DS, et al. Defining the phenotype of schizophrenia: at cognitive dysmetria and its neural mechanisms. Biol Psychiatry 1999;46:908–920 [DOI] [PubMed] [Google Scholar]
- 11.Berman I, Merson A, Sison C, et al. Regional cerebral blood flow changes associated with risperidone treatment in elderly schizophrenia patients: a pilot study. Psychopharmacol Bull 1996;32:95–100 [PubMed] [Google Scholar]