Abstract
Summary: Clear-cell meningioma is a rare disease entity showing a more aggressive nature, clinically, than those of other subtypes of meningioma. It occurs in younger persons and commonly in the spinal canal. The recurrence rate has been reported to be as high as 60%. We present a case of clear-cell meningioma in a 17-year-old man in whom initial MR imaging showed localized leptomeningeal enhancement that had progressed into the entire subarachnoid space after surgical resection of the primary tumor.
Clear-cell meningioma is a recently described histologic subtype of meningioma (1), which shows unusual clinical aggressiveness despite its benign histologic nature (2). Metastasis and recurrence are more frequent in clear-cell meningioma than in other subtypes of meningioma (1). The patients' ages are younger than those of other subtypes of meningioma and the common sites are the spinal canal and the posterior fossa (2). We report a clear-cell meningioma with diffuse leptomeningeal seeding in a 17-year-old man and review the previous literature.
Case Report
A 17-year-old man presented with seizure. Initial brain MR imaging showed a 3-cm dural-based mass in the left parietal convexity. The mass was isointense on a T1-weighted MR image, hyperintense on a T2-weighted image, and strongly enhanced with a contrast-enhanced T1-weighted image. Mild communicating hydrocephalus and localized leptomeningeal enhancement around the ipsilateral sylvian fissure was noticed also (Fig 1A). Meningioma was diagnosed, and gross total resection of the main mass was performed. The area of the left sylvian fissure, showing the leptomeningeal enhancement, was not exposed during the operation. Pathologic examination revealed that the tumor was composed of monotonous round cells with a fine nuclear chromatin and perinuclear halo of clear cytoplasm (Fig 1B). Collagen bundles were scattered in the tumor; however, whorls of meningothelial cells were noted only occasionally. Mitoses were noted up to six per ten high-power fields in the most active area. Neither nuclear pleomorphism nor tumor necrosis was present. Brain parenchymal invasion was absent. Immunohistochemical studies showed no expression of vimentin, epithelial membrane antigen, glial fibrillary acidic protein, or p53 in the tumor cells. Clear-cell meningioma and metastatic clear-cell carcinoma were considered as a differential diagnosis on a pathologic basis. Metastasis workup revealed no primary focus including the kidneys, and the tumor cells did not express cytokeratin immunohistochemically. Therefore, the mass was diagnosed as clear-cell meningioma.
fig 1.
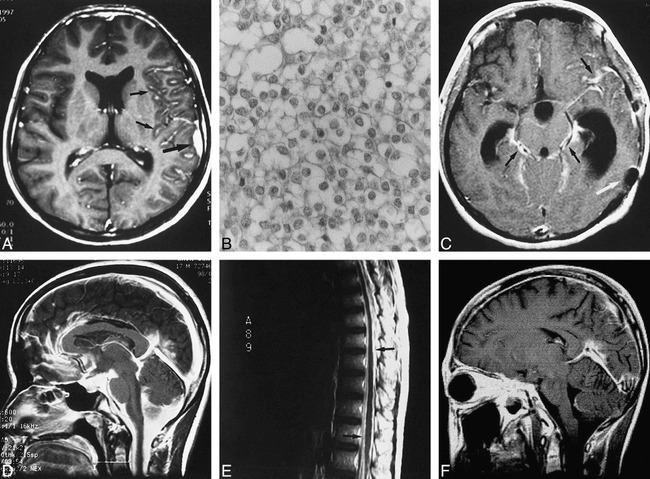
MR imaging findings of clear-cell meningioma with diffuse leptomeningeal seeding in 17-year-old man.
A, Initial contrast-enhanced T1-weighted axial MR image shows 1 × 3-cm, strongly enhancing mass at left parietal convexity (arrow) associated with localized leptomeningeal enhancement in ipsilateral sylvian fissure (small arrows). Mild hydrocephalus is noted also. Mass was isointense on T1-weighted image and slightly hyperintense on T2-weighted image (not shown).
B, Photomicrograph of cerebral tumor. Tumor is composed of back-to-back monotonous round cells with clear cytoplasm and fine nuclear chromatin. (hematoxylin & eosin stain, × 200).
C, Contrast-enhanced T1-weighted axial MR image obtained 7 months later shows extension of leptomeningeal enhancement into subarachnoid space around anterior portions of left frontal and parietal lobes and perimesencephalic cistern (small arrows). Hydrocephalus was greater. Round low intensity in left posterior temporal calvarial region is owing to susceptibility artifact secondary to previous surgery (arrow).
D, Contrast-enhanced T1-weighted sagittal MR image obtained another 7 months later shows more diffuse enhancement of almost entire subarachnoid space. Hydrocephalus disappeared after placement of ventriculoperitoneal shunt (not shown).
E, Contrast-enhanced T1-weighted sagittal MR image of whole spine taken at same time as D shows diffuse leptomeningeal enhancement along surface of whole spinal cord and nerve roots (small arrows).
F, Contrast-enhanced T1-weighted sagittal MR image 2 months after radiation therapy shows marked decrease of diffuse enhancement of subarachnoid space compared with that of figure D.
Seven months later, the patient complained of headache. Follow-up brain MR imaging showed markedly increased communicating hydrocephalus and increased diffuse leptomeningeal enhancement along the surface of both cerebral hemispheres and the pons, and around the basal cisterns (Fig 1C). No parenchymal abnormality, including the primary tumor site, was noticed. Ventriculoperitoneal shunt was performed and the hydrocephalus disappeared. Another 7 months later, the patient complained of another seizure and coccygeal pain. The third brain MR series showed homogeneous enhancement of almost the entire subarachnoid space, including the basal cisterns and the fourth ventricle (Fig 1D). MR imaging of the spine, performed during the same imaging session, also showed diffuse leptomeningeal enhancement along the entire spinal cord (Fig 1E). No parenchymal abnormalities in the brain and the spinal cord, however, were noted. These findings suggested diffuse leptomeningeal seeding of previously existing clear-cell meningioma. In the CSF exam, RBC was more than 1012/mm3, WBC was 259/mm3 and protein was 2155 mg/dL. Clinical symptoms and signs of infection, such as fever and elevated ESR or CRP, were not noticed. Total laminectomy and dural biopsy at the L4–5 level were performed. When the dura was opened, gelatinous material gushed out. Pathologic examination revealed infiltration of monotonous round cells, with clear cytoplasm in the meningeal fibrous tissue. Immunohistochemical studies revealed no expression of cytokeratin, epithelial membrane antigen, vimentin, or CD-68 (macrophage marker) in the tumor cells. Because the cytologic and histologic features were the same as those of the cerebral clear-cell meningioma, leptomeningeal seeding of clear-cell meningioma was confirmed.
Seven months after lumbar surgery, the patient underwent radiation therapy to the whole brain and the whole spine, with a radiation dose of 3960 to 5400 cGy and 3600 to 4500 cGy, respectively. Two months after the radiation therapy, brain MR imaging showed marked decrease of the leptomeningeal enhancement (Fig 1F). Currently, the patient has mild headaches and seizures, which are controlled with medication.
Discussion
The clear-cell meningioma is a meningioma variant in the new World Health Organization classification of tumors of the central nervous system (1). It is rare and potentially aggressive clinically in that it may recur, spread locally, and even metastasize, despite its bland histologic appearance (3). Cytologically, clear-cell meningioma has a whorled, syncytial architecture and spindled-to-polygonal, bland-appearing nuclei. In contrast to the more classic meningioma, the clear-cell variety has vacuolated cytoplasm (4). Mitoses are rare in primary tumors. Immunohistochemistry shows that tumor cells are positive for vimentin and epithelial membrane antigen (1). Clear-cell meningioma is histologically unique but should be differentiated from other similar clear cell tumors of the central nervous system, such as metastatic renal cell carcinoma, hemangioblastoma, oligodendroglioma, germinoma, pleomorphic xanthoastrocytoma, lipid-rich glioblastoma, and clear-cell ependymoma (3, 5).
We reviewed 28 cases of clear-cell meningioma reported in the previous literature (1–11) and our one case. Mean age of previously studied patients was 29.8 years and ranged from 22 months to 67 years. There were 13 male patients, 14 female patients, and two of unknown gender, suggesting no sex predilection. Of the 29 cases of clear-cell meningioma, 14 (48%) were spinal-intradural, six were supratentorial, four arose in the cerebellopontine angle, two were tentorial, one was on the skull base, and one was centered on the foramen magnum. A brain parenchymal clear-cell meningioma was reported also (6). Two of the spinal clear-cell meningiomas were reported as nondural-based masses (1, 7). In reviewing the previous reports on the radiologic aspects, most primary clear-cell meningiomas did not show any different features from those of conventional meningiomas. Nonetheless, nondural-based or parenchymal tumors may not be so rare in clear-cell meningioma, considering that only 29 cases of clear-cell meningioma have been reported. The most interesting aspect of clear-cell meningioma is the high recurrence rate. Zorludemir et al (1) reported that clear-cell meningioma showed 61% recurrence, including 15% local discontinuous spread and 8% widespread cranial to spinal metastasis in their 13-case series (1). There was another report of clear-cell meningioma that showed an extensive infiltrative growth pattern and high recurrence rate (9). We found 14 recurrences in 23 clear-cell meningiomas described in the literature. The overall recurrence rate was 60.9%; the recurrence rate of intracranial clear-cell meningioma was 80% (8/10), whereas that of spinal clear-cell meningioma was 46% (6/13). The patterns of recurrent tumor were: local recurrence in seven cases; nodular mass, probably seeding through the CSF space, in four cases; diffuse leptomeningeal seeding in two cases, including our case; and locally infiltrative growth in one case. There was a report of clear-cell meningioma that showed extraspinal and retropleular extension but no recurrence after gross total resection (1).
There was no report regarding the long-term result of clear-cell meningioma except one by Zorludemir et al (1). In that report, of the six patients who had been followed more than 5 years, three patients died of tumor at 1 month, 27 months, and 12 years, respectively, after diagnosis. Two of the remaining three patients had been alive with disease for 8 years and 13 years, respectively. The last patient had been alive with no evidence of disease for 7 years. All of the previous six patients experienced recurrence of tumor once or twice.
Treatment of choice in clear-cell meningioma is surgical removal. Radiosurgery and radiotherapy have been considered generally as a treatment option in recurring cases.
Extensive contrast enhancement of the entire cisternal spaces on MR imaging suggestive of extensive CSF seeding, as seen in our case, appears to be rare and, to our knowledge, has not been reported previously. The gelatinous material found during lumbar surgery probably was responsible for the enhanced CSF space on MR imaging (Fig 1D–E).
The meningioma associated with leptomeningeal enhancement on the preoperative neuroimaging study may suggest clear-cell meningioma, even though leptomeningeal seeding has been reported in other types of meningioma (12, 13).
Histologic parameters do not predict recurrence, because cellular anaplasia is lacking and growth fraction is low in most clear-cell meningioma. Neuroimaging findings of localized leptomeningeal enhancement associated with meningioma, as seen in the first MR imaging of our case (Fig 1A), may be the predictable finding of clear-cell meningioma.
Conclusion
Clear-cell meningioma is a histologically unique, rare subtype of meningioma that has a higher recurrence rate than typical meningiomas. Its recurrence occurs through either local recurrence or CSF seeding.
Neuroimaging findings typical of meningioma, but accompanied with leptomeningeal enhancement, may suggest clear-cell meningioma. Clear-cell meningioma must be followed up carefully because of its aggressive behavior, even when benign histologic results are obtained.
Footnotes
Address reprint request to Kee-Hyun Chang, MD, Department of Radiology, Seoul National University, College of Medicine, 28, Yongon-dong, Chongno-gu, Seoul, 110–744, Korea.
References
- 1.Zorludemir S, Scheithauer BW, Hirose T, Van Houten C, Miller G, Meyer FB. Clear cell meningioma. A clinicopathologic study of a potentially aggressive variant of meningioma. Am J Surg Pathol 1995;19:493-505 [PubMed] [Google Scholar]
- 2.Pimentel J, Fernandes A, Pinto AE, Fonseca I, Moura Nunes JF, Lobo Antunes J. Clear cell meningioma variant and clinical aggressiveness. Clin Neuropathol 1998;17:141-146 [PubMed] [Google Scholar]
- 3.Shih DF, Wang JS, Pan RG, Tseng HH. Clear cell meningioma: a case report. Chung Hua I Hsueh Tsa Chih 1996;57:452-456 [PubMed] [Google Scholar]
- 4.Imlay SP, Snider TE, Raab SS. Clear-cell meningioma: diagnosis by fine-needle aspiration biopsy. Diagn Cytopathol 1998;18:131-136 [DOI] [PubMed] [Google Scholar]
- 5.Gokden M, Roth KA, Carroll SL, Wick MR, Schmidt RE. Clear cell neoplasms and pseudoneoplastic lesions of the central nervous system. Semin Diagn Pathol 1997;14:253-269 [PubMed] [Google Scholar]
- 6.Teo JG, Goh KY, Rosenblum MK, Muszynski CA, Epstein FJ. Intraparenchymal clear cell meningioma of the brainstem in a 2-year-old child. Case report and literature review. Pediatr Neurosurg 1998;28:27-30 (abst) [DOI] [PubMed] [Google Scholar]
- 7.Holtzman RN, Jormark SC. Nondural-based lumbar clear cell meningioma. Case report. J Neurosurg 1996;84:264-266 [DOI] [PubMed] [Google Scholar]
- 8.Matsui H, Kanamori M, Abe Y, Sakai T, Wakaki K. Multifocal clear cell meningioma in the spine: a case report. Neurosurg Rev 1998;21:171-173 [DOI] [PubMed] [Google Scholar]
- 9.Prinz M, Patt S, Mitrovics T, Cervos-Navarro J. Clear cell meningioma: report of a spinal case. Gen Diagn Pathol 1996;141:261-267 [PubMed] [Google Scholar]
- 10.Cances C, Chaix Y, Karsenty C, et al. Clear cell meningioma: recurrent intraspinal tumor in a child. Arch Pediatr 1998;5:758-762 [DOI] [PubMed] [Google Scholar]
- 11.Ito T, Nakamura H, Oka K, Nakagawara J, Nagashima K. A case of clear cell meningioma originating from the cerebellar tentorium. No Shinkei Geka 1998;26:265-270 (abst) [PubMed] [Google Scholar]
- 12.Kamiya K, Inagawa T, Nagasako R. Malignant intraventricular meningioma with spinal metastasis through the cerebrospinal fluid. Surg Neurol 1989;32:213-218 [DOI] [PubMed] [Google Scholar]
- 13.Miller AA, Ramsden F. Malignant meningioma with extracranial metastases and seeding of the subarachnoid space and the ventricles. Pathol Eur 1972;7:167-175 [PubMed] [Google Scholar]


