Abstract
Summary: CT fluoroscopy may be used as a rapid and effective means of guiding needle placement when performing selective lumbar nerve root blocks. In this set of patients, the average external radiation dose was 0.73 mrem per procedure, with an average of 2 seconds of CT-fluoroscopy time and four images per procedure. Average physician room time was 7 minutes. Use of intermittent CT fluoroscopy during lumbar selective nerve root blocks can result in minimal radiation dose levels and procedure times that are comparable to fluoroscopic guidance.
Selective lumbar nerve root blocks (SNRB) have long been a staple of anesthesiologists and orthopedic surgeons, but have been increasingly performed by neuroradiologists and interventional radiologists (1). Initially performed by using deep and surface anatomic landmarks and a large amount of local anesthetic, the procedures were not very specific. Fluoroscopic guidance increased the accuracy of needle placement, and thus the specificity of the examination, and is still used by many practitioners. Numerous articles have described and advocated CT guidance for SNRB, citing the excellent visualization of the nerve root, ganglion, and surrounding structures, thus allowing precise placement of the needle tip without the use of iodinated contrast medium (2–4). One disadvantage often cited by opponents of CT guidance is the increased physician time involved in the procedure, as opposed to fluoroscopic guidance. Low-dose CT fluoroscopy is a relatively new technique that allows rapid imaging during needle placement while the operator is standing at the bedside, dramatically reducing the procedure time while retaining the benefits of CT guidance. This study evaluates operator time, fluoroscopic time, and radiation dose of CT fluoroscopic-guided lumbar SNRB.
Description of Technique, Patients Studied, and Results
This study includes 348 selective lumbar nerve root blocks performed at our institution over a 38-month period. Over a 5-month subperiod, 54 sequential CT fluoroscopically guided lumbar SNRBs were performed in 54 patients and used to determine procedure time and radiation dose. All procedures were performed by a single operator on a single-detector spiral CT scanner that had been modified for CT fluoroscopy. The operator wore a commercially available dosimeter on the chest pocket of the lead apron for each procedure. Between procedures, the dosimeter was kept in an office drawer, away from possible radiation exposure, and was returned to the drawer immediately after each procedure. The dosimeter was used exclusively for this study and was not worn or moved at any other time. Because of the small doses measured during the procedures and the 1-mrem threshold of detection for the dosimeter, doses for individual cases could not be calculated, and the total dose was divided by the number of procedures at the end to obtain a mean dose per procedure.
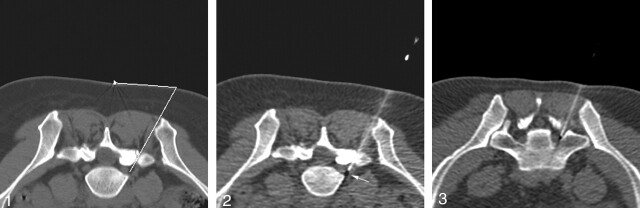
SNRB was performed with the patient in the prone position on the gantry. A linear marker affixed by silk tape was attached to the skin at the approximate level by the technologist. Before the physician entered the room, the technologist had laid out the necessary equipment, and imaged the desired level by using 3-mm axial contiguous sections from the inferior pedicle until the nerve root was seen exiting the foramen (Fig 1). Time recording was initiated when the radiologist entered the control room to pick the appropriate section and measure the angle. The skin entry site was marked with a surgical pen under sterile conditions, and 1% lidocaine was used for local anesthesia. A 22-gauge, 5-inch spinal needle was maneuvered directly adjacent to the nerve root in the outer neural foramen by using incremental low-dose CT fluoroscopy via a posterolateral approach (Figs 2 and 3). The operator performed the procedure while standing approximately 3 feet from the tube. Once optimal needle placement was achieved, a mixture of 80 mg depomedrol mixed with 1 mL 0.25% bupivacaine was drawn up and slowly infiltrated around the nerve. The needle was withdrawn with pressure held by the radiologist. Time recording was stopped when the radiologist left the room and was rounded to the nearest whole number, because smaller time distinctions were thought to be relatively unimportant. The number of fluoroscopic images and total fluoroscopy time needed to place the needle was also recorded. Because the equipment calculates fluoroscopy only in whole seconds, this number was used to calculate the mean fluoroscopy time and ranges.
Fig 1.
Initial scout image shows the nerve root in the neural foramen, indicating an appropriate injection level. The distance tool is used to calculate an appropriate skin injection site. Once the technologists become familiar with the anatomy, many studies can be done with only one or two scout images.
Fig 2.
Image from CT fluoroscopy-guided nerve root block demonstrates the needle tip in the outer neural foramen. Note that the image is not as sharp as standard CT images due to the low mA used with this technique.
Fig 3.
S1 nerve root block shows the needle traversing the sacral foramen and lying directly adjacent to the S1 nerve.
Of the 348 patients who underwent single selective lumbar nerve root blocks, there was a success rate of 100% in needle placement. One patient developed hives following the procedure, presumably because of an atopic reaction to either the steroid or local anesthetic. In the subset of 54 patients, the time for the procedure averaged 7 minutes (range, 5–16 minutes), most which was due to preparation of the patient. The average number of images necessary for needle placement was four with a range of 2–8, and the average CT-fluoroscopic time was 2 seconds (range, 1–7 seconds). Total radiation dose to the radiologist for the 54 procedures studied in the patient subset was 39 mrem, giving an average dose of 0.73 mrem per procedure.
Discussion
CT fluoroscopy, which allows low-dose images to be taken in near real time by using partial reconstruction algorithms, was first described by using real-time fluoroscopy to guide biopsies and drainages (5–7). As the technology has improved and become more accessible, it has been used for biopsies of almost all organ systems and is especially useful in deep organs or those, like the lung or liver, that are difficult to localize because of motion (5, 8). With more institutions gaining access to this technology, it seems likely that the number of cases performed with CT fluoroscopy will continue to increase.
CT guidance of SNRB, because of its excellent contrast resolution, has been previously described as allowing precise placement of the needle tip adjacent to the foraminal nerve or ganglion (2, 3), but has been criticized for increased procedure times when compared with fluoroscopic guidance. CT fluoroscopy, which allows the operator to stand by the bedside and manipulate the needle, has been shown to significantly reduce procedure times in other types of intervention. Silverman et al (9) demonstrated decreased procedure times and needle placement times by using CT fluoroscopy as compared with conventional CT guidance by using a number of different operators and techniques. Carlson et al (10) reported a 32% decrease in overall procedure time when comparing CT fluoroscopy to conventional CT guidance.
Radiation dose is an area of concern and study with any new technique that uses ionizing radiation. In Silverman et al’s study (9), the mean fluoroscopic time in these procedures was 79 seconds, with a range of 8–546 seconds. Nawfel et al (11) described a patient dose of 830 mGy from 80 seconds of CT fluoroscopy, by using a 90-mA and 120-kVp exposure. This technique uses a relatively high mA, and most CT fluoroscopic units made today limit the allowable mA to a maximum of 90 mA, with some allowing CT fluoroscopy by using as little as 10 mA. Continuous CT fluoroscopy will result in higher overall doses to the patient and radiologist as opposed to intermittent images (the so-called quick-check method) but is usually only necessary during biopsy of small lesions within moveable organs, such as the lung or liver. In a study by Carlson et al (10), intermittent CT fluoroscopy was used in 97% of patients and resulted in a 94% decrease in median calculated patient-absorbed dose per procedure. In this study, all procedures were performed by using the intermittent, or quick-check, technique to minimize radiation dose to the radiologist and patient, with the result that the fluoroscopy time per procedure was extremely low (median 2 seconds), much lower than previous studies have mentioned.
Lumbar SNRB can safely and easily be performed by using intermittent CT fluoroscopy because of the immobility of the nerve roots and the lack of important adjacent anatomic structure, especially within the lumbar spine. With practice, most lumbar SNRB procedures can be performed by using less than five rapidly acquired images. One problem with intermittent CT fluoroscopy that can increase the number of images and radiation dose is the difficulty finding the needle tip if it deviates from the plane of the image section. This can be minimized by use of the laser function of the CT scanner to ensure that the laser bisects the needle shaft as it enters the skin as well as the needle hub. Should the needle tip be displaced, the direction is usually easily ascertainable by comparing the positions of the needle entry site to the hub as compared with the laser marker (e.g., if the hub is located above the skin entry site, the tip would be deflected inferiorly).
Placing the foot pedal further from the gantry will reduce dosage by the inverse square law, and Nawfel et al (11) found reduced scatter radiation when a lead shield was placed over the patient. Other dose-reducing strategies include limiting the initial scout images to the neural foramen and altering the technique. Paulson et al (12) looked at radiologist dose among various CT fluoroscopic procedures by using very low mA levels (average 13.2 mA, with a range of 10–50mA) and found the mean radiation dose per procedure was 2.5 mrem, with a range among different procedures of 0.66–4.75 mrem. Although nerve root blocks were not included in the procedures of this study, there were 57 facet joint injections and 17 spine biopsies that were considered together when calculating doses. The whole-body dose varied among the three attending radiologists from 0.66 to 2.8 mrem, although each performed widely different numbers of facet injection to spine biopsies. There is no reason to perform CT fluoroscopically guided procedures with more than 50 mA, except for the occasional very obese patient. Using these techniques in this study, the average operator dose per case was well under 1 mrem, which could be reduced even further with equipment that allows less than 50 mA. Also, it must be remembered that the calculated doses for this study and Paulson’s study reflect radiation exposure outside of the lead apron. With the use of appropriate protective wear, including a lead apron, lead glasses, and thyroid shield, the actual dose to the radiologist should be almost nonexistent.
Another negative factor attributed to CT guidance is excessive procedure time, but this is markedly reduced with the use of CT fluoroscopy. The average procedure time was well under 10 minutes, which included selection and measurement of an appropriate image, marking the skin entry site, sterilizing the field, drawing up the local anesthetic and steroid, placing the needle, and holding initial pressure. Because the technologist was trained to select the appropriate pedicle and image through the foramen without the radiologist present, this portion of the study was not included in the calculated physician time. Having skilled and motivated technologists is invaluable in a busy practice and can streamline the process for the patient and radiologist.
Using CT fluoroscopy to guide needle placement also has the advantage in the lumbar spine of making contrast medium injection optional. Many descriptions of the CT-guided technique in the lumbar spine do not include contrast material injection (2, 4, 13), although it should always be injected when performing cervical nerve root blocks because of the chance of injecting into a vessel feeding the anterior spinal artery or vertebral artery. Within the lumbar spine, one must weigh the extremely low risk of injecting into an aberrant artery of Adamkiewicz against the also rare severe contrast medium reaction.
CT fluoroscopy allows rapid and safe needle placement in a variety of procedures. It is especially well suited for selective lumbar nerve root blocks, which are relatively quick procedures when using standard fluoroscopy but can be much longer when standard CT guidance is used. CT fluoroscopy matches the advantages of CT guidance to be matched with the speed of fluoroscopic guidance. Dose rates, which can be high with continuous CT fluoroscopy, can be minimized by exclusively using intermittent fluoroscopy, resulting in negligible dose to the radiologist.
Footnotes
Presented at the 41st annual meeting of the American Society of Neuroradiology, Washington, D.C., April 27–May 2, 2003.
References
- 1.Murtagh R. The neuroradiologist as pain therapist. AJNR Am J Neuroradiol 1998;19:353–354 [Google Scholar]
- 2.Quinn SF, Murtagh R. CT-guided nerve root sleeve block and ablation. AJR Am J Roentgenol 1988;151:1213–1216 [DOI] [PubMed] [Google Scholar]
- 3.Zennaro H, Dousset V, Viaund B, et al. Periganglionic foraminal steroid injections performed under CT control. AJNR AM J Neuroradiol 1998;19:349–352 [PMC free article] [PubMed] [Google Scholar]
- 4.Murtagh R. The art and science of nerve root and facet blocks. Neuroimaging Clin N Am 2000;10:465–477 [PubMed] [Google Scholar]
- 5.Katada K, Anno H, Ogura Y, et al. Early clinical experience with real-time CT fluoroscopy. Nippon Acta Radiol 1994;54:1172–1174 [PubMed] [Google Scholar]
- 6.Katada K, Kato R, Anno H, et al. Guidance with real-time CT fluoroscopy:early clinical experience. Radiology 1996;200:851–856 [DOI] [PubMed] [Google Scholar]
- 7.Meyer CA, White CS, Wu J, et al. Real-time CT fluoroscopy: usefulness in thoracic drainage. AJR Am J Roentgenol 1998;171:1097–1101 [DOI] [PubMed] [Google Scholar]
- 8.Muehlstaedt M, Bruening R, Diebold J, et al. CT/fluoroscopy-guided transthoracic needle biopsy: sensitivity and complications in 98 procedures. J Comput Assist Tomogr 2002;26:191–196 [DOI] [PubMed] [Google Scholar]
- 9.Silverman SG, Tuncali K, Adams DF, et al. CT fluoroscopy-guided abdominal interventions: techniques, results, and radiation exposure. Radiology 1999;212:676–681 [DOI] [PubMed] [Google Scholar]
- 10.Carlson SK, Bender CE, Classic KL, et al. Benefits and safety of CT fluoroscopy in interventional radiologic procedures. Radiology 2001;219:515–520 [DOI] [PubMed] [Google Scholar]
- 11.Nawfel RD, Judy PF, Silverman SG, et al. Patient and personnel exposure during CT fluoroscopy-guided interventional procedures. Radiology 2000;216:180–184 [DOI] [PubMed] [Google Scholar]
- 12.Paulson EK, Sheafor DH, Enterline DS, et al. CT fluoroscopy-guided interventional procedures: techniques and radiation dose to radiologists. Radiology 2001;220:161–167 [DOI] [PubMed] [Google Scholar]
- 13.Wagner AL, Murtagh FR. Selective nerve root blocks. Tech Vasc Interv Radiol 2002;5:194–200 [DOI] [PubMed] [Google Scholar]