Abstract
The global coronavirus pandemic (Covid 19) resulted in national lockdowns where individuals were asked to isolate in their homes to stop the spread of the disease. Using a cross-sectional survey, the current paper aimed to examine self-reported changes in eating patterns and behaviour during the lockdown in the UK, and associations with BMI, demographic variables, eating styles, health anxiety, food insecurity and coping strategies. Participants (N = 620) were recruited online through social media advertising. The results showed that there were self-reported changes to food consumption during the lockdown across the sample. Increases in consumption of HED (high energy density) snack foods during the lockdown was associated with sex, pre-lockdown eating behaviour (emotional eating and uncontrolled eating), and Covid-specific health anxiety. Increases in positive eating practices such as eating more home prepared foods, and fruits and vegetables, were associated with adaptive coping strategies. Higher emotional eating (EE) during the lockdown was associated with a higher BMI, higher pre-lockdown EE and maladaptive coping strategies. Maladaptive coping strategies moderated the relationship between BMI and EE during the lockdown. In particular a higher BMI was associated with higher EE during the lockdown if an individual also had higher maladaptive coping strategies. These findings suggest that changes to eating behaviour may be part of a wider style of maladaptive or adaptive coping, particularly in those with a history of EE or uncontrolled eating. Preparing individuals to adopt more adaptive coping strategies during lockdown situations may be crucial to improving health during subsequent the lockdown events.
Keywords: Emotional eating, Hed foods, Covid 19, Health anxiety, Coping, Lockdown
1. Introduction
The coronavirus (Covid 19) pandemic resulted in the UK government issuing a ‘lockdown’ on the 23rd of March 2020, whereby the entire population of the UK were told to, ‘Stay home, Protect the NHS, Save lives’(Gov.UK, 2020). Globally, the unprecedented scale of the virus and its associated lockdown measures has led to adverse psychological consequences, in particular anxiety relating to health and the virus (Jungmann & Witthöft, 2020; Van Rheenen et al., 2020). There is emerging evidence that psychological distress and risk perception has been particularly high in the UK compared to other countries experiencing the pandemic (Dryhurst et al., 2020). It has also been identified that individuals with eating disorders, such as binge eating disorder, bulimia nervosa and anorexia nervosa, are at risk from this unique environment (Touyz, Lacey, & Hay, 2020), and that lockdown in Australia has led to increased bingeing, purging and restriction in those with diagnosed eating disorders (Phillipou et al., 2020). Recent descriptive data on changes to eating behaviour in non-clinical populations during the lockdown has found both increased unhealthy consumption (Marty, de Lauzon-Guillain, Labesse, & Nicklaus, 2021; Robinson et al., 2020) but also healthier consumption of home prepared (Di Renzo, Gualtieri, & Pivari, 2020) and sustainable foods (Marty et al., 2021).
Research on populations who experienced previous pandemics such as H1N1, Ebola and SARS has shown that concerns about health, anxiety, and poor psychosocial functioning are common, particularly in those affected by the condition (Cowling et al., 2010; Jalloh et al., 2018; Ko, Yen, Yen, & Yang, 2006; Peng et al., 2010; (Williams, Regagliolo & Rasmussen, 2012)). Recent research into the current coronavirus pandemic has found that health anxiety is being experienced by many individuals and is strongly associated with trait anxiety and poor emotional regulation strategies (Jungmann & Witthöft, 2020). Health anxiety is a type of anxiety based on the fear or belief that an individual has the signs or symptoms of a serious illness. It is associated with general anxiety and is present in both clinical and non-clinical populations (Alberts, Hadjistavropoulos, Jones, & Sharpe, 2013). During a pandemic, anxiety about the virus has a predictable course, with many people showing higher health anxiety and risk avoidance behaviours in initial stages which decreases over time (Liao, Cowling, Lam, Ng, & Fielding, 2014; Yeung, Lau, Choi, & Griffiths, 2017). This suggests that the early stages of a pandemic are particularly associated with poor psychosocial functioning and distress.
Unanticipated natural or societal disasters can lead to disruptions to food supplies. Most of the research in this area is based on eating behaviour after earthquakes or hurricanes (Kuijer & Boyce, 2012; Turner-McGrivey et al., 2020; Xu et al., 2018). Interestingly, effects seem to be both related to increased desire for healthy eating driven by food safety concerns (Rukundo et al., 2016a, 2016b; Xu et al., 2018), and increased unhealthy eating driven by faulty coping strategies (Kuijer & Boyce, 2012; Turer-McGrivey et al., 2020). Natural disasters have also been associated with food insecurity due to disrupted supply chains and altered diet in those without economic and practical food related support (Alias & Nor, 2018). In the Covid 19 pandemic in the UK, rates of food insecurity increased dramatically as a result of both economic hardship, and disputed supply chains, especially for those who were vulnerable to the virus (Barker & Russell, 2020).Food insecurity in economically affluent countries has been associated with HED (foods high in energy density) consumption, overeating and overweight/obesity, and lower intake of health foods such as fruits and vegetables (Hanson & Connor, 2014; Mello et al., 2010) as food insecure individuals will eat more during cycles where they can access foods (Stinson et al., 2018).
Overeating of highly palatable HED snack foods such as chocolate, crisps and biscuits is more common in individuals in heightened emotional states (Bennett, Greene, & Schwartz-Barcott, 2013; Evers, Dingemans, Junhans, & Boevé, 2018; Greeno & Wing, 1994; Nguyen-Rodriguez, Chou, Unger, & Spruijt-Metz, 2008), to the extent where these foods are often referred to as comfort foods, implying they have an emotional regulation function (Evers, Stok, & De Ridder, 2010). The tendency to overeat in response to emotions such as stress, sadness, boredom, anxiety, or irritability, has been defined as Emotional Eating (EE; Van Strien et al., 2007; Braden, Musher-Eizenman, Watford & Emley, 2018). Emotional eaters show general patterns of emotion dysregulation, the need to escape from negative affect, and rumination (Gibson, 2012). One particular reason why emotional eating can increase in negative situations is because some individuals may use food to cope emotionally rather than using more adaptive methods of regulating their emotions (Spoor, Bekker, Van Strien, & Van Heck, 2007). Recent cross-sectional findings suggest that individuals who report higher perceived stress during the pandemic, also have higher EE (Shen, Long, Shih, & Ludy, 2020). EE is much more common in individuals who have overweight or obesity (Peneau, Menard, Mejean, Bellisle, & Hercberg, 2013), and worries about weight gain as a result of EE can lead to feelings of guilt (Dubé, LeBel, & Lu, 2005; Macht & Dettmer, 2006) and thereby potentially even cancelling out the short-term reduction in negative effect. It has additionally been found that those people who report a larger variety of strategies for coping with aversities have better mental health in general and are also less likely to report to engage in EE (Cheng, Lau, & Chan, 2014; Van den Tol, Coulthard, & Hanser, 2018) and found that eating is generally reported by people to be the least successful strategy for changing a bad mood (Thayer, Newman, & McClain, 1994) out of a number of affect regulation behaviours.
Most research in EE has focused on responses to emotional induction stressors such as performing a task or to daily hassles in everyday life (Evers et al., 2018; van Strien et al., 2013). Only one study has examined overeating in response to stress and environmental changes caused by a natural disaster; an earthquake in Christchurch, NZ in 2008 (Kuijer & Boyce, 2012). They found that EE did not change one month after the earthquake relative to baseline in the sample as a whole. However, they found a moderation effect with emotional distress about the earthquake, experienced in about 20% of their sample. This emotional distress, combined with higher baseline EE, led to greater consumption of ‘junk’ foods after the Earthquake. This suggests that, for some susceptible individuals who have problematic eating behaviours, if they are distressed by an event, this can trigger overconsumption episodes and the use of food to regulate emotions. Thus, anxiety about the event may be crucial in determining whether an event will trigger overeating as a response in individuals who are susceptible to EE behaviour. In the case of Covid 19, we believed that anxiety about the specific virus, and health anxiety in general, would be potentially important factors in changes to eating behaviour.
The present study aimed at examining the effects of the Covid 19 lockdown on changes to self-reported food consumption and EE in a sample of adults in the UK in the early part of the lockdown (April–May 2020). Based on previous research it was important to examine health anxiety in relation to the pandemic, as well as food insecurity and coping strategies. As individuals were experiencing the pandemic differently depending on their vulnerability to the virus, it was also important to measure access to foods through shopping, shielding, and employment status, as well as BMI. An exploratory approach was adopted, as this was a unique food environment. Firstly, we aimed to examine changes to perceived eating behaviour and their associations with factors caused by the lockdown, such as shielding, access to food shops, and employment status. Secondly, we aimed to examine whether these changes were associated with demographic factors, food insecurity, coping strategies and health anxiety.
2. Method and materials
2.1. Participants
Seven hundred and fifty participants were recruited through opportunity sampling from social media posts. The majority of the posts were on XX University Twitter pages, as well as those of the researchers (Twitter, Facebook, Instagram, Whatsapp), and snowballing from these sites. To be included in the study participants needed to be over 18 years old, and a resident in the UK. Participants who had tested positive for coronavirus were not eligible to participate. Sample size estimates for multiple regression with 20 potential predictor variables (G power calculation; medium effect size, p < .05, Power = 0.95) indicated that a minimum of 222 participants were required. 620 participants finished the questionnaire materials and were included in the final sample. The mean age of participants was 39.90 (SD = 13.96) years, ranging from 18 to 77 years. The mean BMI was 26.74 (SD = 6.12) kg/m2. Table 1 contains full details of the demographic characteristics of the final sample. The sample was overwhelmingly female, white-British/European and working from home. The majority of participants stated that they were located in the East and West Midlands of the UK (n = 451).
Table 1.
Demographic frequency characteristics of a sample of 620 adults under lockdown.
| N(%) |
Emotional eating (Lockdown) |
HED |
FV |
Homeprepared |
|
|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | ||
| Sex | |||||
| Female | 546(88%) | 7.17(2.75) | 0.21(0.88) | 0.06(0.70) | 0.69(0.87) |
| Male | 74(12%) | 5.47(2.25)** | −0.16(0.93) ** | 0.21(0.95) | 0.87(1.06) |
| Children in house | |||||
| Yes | 204 (33%) | 7.18(2.84) | 0.29(0.99)* | 0.12(0.94) | 0.81(1.14) |
| No | 416 (67%) | 6.87(2.92) | 0.11(0.86) | 0.21(0.90) | 0.85(0.97) |
| Isolating in house (missing n = 19) | |||||
| Yes | 102(16%) | 7.62(2.98) | 0.21(0.97) | 0.12(1.03) | 1.01(1.36) |
| No | 518(81%) | 6.83(2.87)* | 0.16(0.90) | 0.20(0.90) | 0.82(0.96) |
| Occupational classification | |||||
| Professional | 226(39%) | 6.64(2.90) | 0.16(0.90) | 0.25(0.92) | 0.88(0.96) |
| Intermediate | 121(21%) | 7.36(2.92) | 0.18(1.00) | −0.01(0.90) | 0.95(1.00) |
| Manual | 87(15%) | 7.55(2.93)* | 0.23(0.88) | 0.23(0.93) | 0.87(1.40) |
| Not working | 155 (25%) | 6.78(2.94) | 0.15(0.89) | 0.23(0.93) | 0.71(0.99) |
| Employment status | |||||
| Working from home | 293(47%) | 6.78(2.83) | 0.16(0.94) | 0.15(0.9) | 0.91(0.95) |
| Essential worker | 75 (12%) | 7.38(3.24) | 0.23(0.94) | 0.25(1.01) | 0.75(1.41) |
| Furloughed | 78(13%) | 7.58(2.74) | 0.23(0.87) | 0.14(0.96) | 0.99(1.09) |
| Lost employment | 19(3%) | 6.75(2.73) | 0.14(0.90) | 0.14(0.55) | 0.71(0.70) |
| Not working prior to lockdown/Retired | 155 (25%) | 6.78(2.94) | 0.15(0.89) | 0.23(0.93) | 0.71(0.99) |
| Food insecurity status | |||||
| None | 397(65%) | 6.73(2.87)* | 0.17(0.87) | 0.26(0.89)* | 0.90(1.02) |
| Mild | 180 (29%) | 7.20(2.90) | 0.27(0.99) | 0.18(0.90) | 0.91(1.04) |
| Moderate/severe | 65 (6%) | 7.52(2.93) | 0.08(1.06) | −0.14(1.03) | 0.66(1.06) |
| Shopping behaviour | |||||
| Doing own shopping | |||||
| Yes | 482(77%) | 6.86 | 0.21* | 0.19 | 0.82 |
| No | 136 (23%) | 7.22 | 0.04 | 0.17 | 0.89 |
| Ethnicity | |||||
| White- British/European | 565(88%) | 6.94(2.90) | 0.17(0.87) | 0.18(0.93) | 0.85(1.02) |
| Asian/British Asian | 35(6%) | 7.61(3.10) | 0.23(1.00) | 0.37(0.90) | 0.92(1.30) |
| Black/Black British | 8(1%) | 5.29(2.63) | 0.14(1.35) | 0.21(0.76) | 0.79(1.11) |
| Other | 27(4%) | 7.61(2.50) | 0.35(1.09) | 0.16(0.90) | 0.79(1.02) |
| Prefer not to say | 4(1%) | ||||
2.2. The event
The global coronavirus pandemic, Covid 19, was first detected in the city of Wuhan, China in late 2019 (WHO, 2020). By March 2020, the virus was spreading across multiple countries who responded by implementing social distancing measures to try and contain the spread of the infection and avert a health crisis. On Monday 23rd March 2020, the British Government recommended a lockdown where people were advised to, ‘Stay at home, Protect the NHS, Save lives’ (Gov.UK, 2020).
Leaving the home was allowed for four reasons; to exercise once a day, to shop for essentials such as food, to work outside the home as an essential worker, and to get medical treatment. In addition to this guidance, it was recommended that certain groups of individuals with pre-existing medical problems, those over 70, and pregnant women be shielded, whereby they should not leave the house except for emergency medical treatment. An additional group was identified as extremely vulnerable, which included those with COPD (chronic pulmonary obstructive disorder), undergoing active chemotherapy, and people in receipt of an organ donation. Those who were identified as vulnerable or extremely vulnerable were told to shield for 12 weeks from 23rd March.
As a consequence of the lockdown, citizens experienced dramatic and sudden changes to their daily routines and habits, including changes to many of their food environments. Many people were isolated in their homes, some with financial uncertainty, some experiencing food insecurity, and some with heightened vulnerability to the virus. These recommendations led to a spate of panic buying, and many vulnerable individuals were unable to access food deliveries in the initial weeks following lockdown (Nicola et al., 2020).
2.3. Materials
Demographic characteristics. Participants were required to provide details about their sex (male, female, prefer not to say), age (years), shielding status (shielding vs not), BMI (kg/m2), number of household members (children and adults), occupational status (ONS, 2010; professional/managerial, intermediate and manual),employment status (working from home, essential worker, furloughed, lost employment, not working/retired prior to the Lockdown), ethnicity (white-British/European, Asian/British Asian, Black/Black British, other and prefer not to say) and shopping behaviour (doing own shopping vs relying on others/delivery). Geographical location was also measured but not used in any analyses.
Food Consumption. Participants completed questions about changes to their intake of certain foods. We based our items on measures of high energy density snack foods, and also on fruits and vegetables (Hawkins, Farrow, & Thomas, 2020), as consumption of these two food groups are associated with unhealthy and healthy diets. In addition, as the lockdown meant that individuals were in their home environment, we wanted to examine whether there were shifts in consumption from eating out to eating in the home (Nicola et al., 2020). For each food category, participants were asked ‘Has your consumption of the following food items changed since the lockdown’ in relation to 10 food categories 1) Puddings, biscuits and cake, 2) Sweets and chocolate 3) Crisps and savoury snacks, 4) Fried foods, 5) Take away meals, 6) Home-made meals, 7) Home baked foods, 8) Fruits, 9) Vegetables, 10) Alcohol. For each of the 10 food categories, participants were asked to rate if they were, consuming much more than usual (2), consuming a little more than usual (1), consuming the same as usual (0), consuming a little less than usual (−1), and consuming less than usual (−2). As the Lockdown was an unusual food environment, and to identify clusters of eating behaviours in the present study from 10 food groups, a Principal Components factor analysis with varimax rotation was carried out to create factors based on food group self-perceived food consumption variables. Three factors were identified which had eigenvalues >1. Factor 1: HED (25.75% % of the variance) which contained 1) Puddings, biscuits and cake (0.82), 2) Sweets and chocolate (0.78) 3) Crisps and savoury snacks (0.76), and 4) Fried foods (0.61). Factor 2: fruit and vegetables (FV) which explained 16.96% of the variance and contained fruits (0.83) and vegetables (0.79), and factor 3: home prepared foods, which explained 11.85% of the variance and contained Home baked foods (0.67), home-made meals (0.67), and takeaway meals (reversed 0.60). Alcohol consumption loaded separately onto a single factor, so was treated as a separate variable. For each factor, HED, FV and Home prepared, a higher score indicated an increase in consumption of those foods.
Eating Behaviours: The Three-Factor Eating Questionnaire – Revised 18-item version (TFEQ-R18) (de Lauzon et al., 2004). The Three-Factor Eating questionnaire- R18 (TFEQ-R18) is a shortened and revised version of the original 51-item TFEQ which assessed a population with obesity (Stunkard & Messick, 1985). The TFEQ-R18 was developed to assess the relationship between eating behaviours and reported food intake in the general population. The TFEQ-R18 consists of 18 items measuring three aspects of ‘normal’ eating behaviours/patterns; (1) Cognitive Restraint (CR) for example, ‘Do you consciously hold back at meals in order not to gain weight?’ (6 items), (2) Uncontrolled Eating (UE) for example, ‘Sometimes when you start eating, do you feel you just can't seem to stop?’ and (3) Emotional Eating (EE) for example, ‘When you feel lonely, do you console yourself by eating?’. Responses are on a 4-point Likert scale ranging from 4 definitely true to 1 definitely false, and responses are summated into individual scale scores with a higher score indicating a higher level of CR, UE or EE. The three items of the EE subscale were filled in twice in relation to emotional eating behaviour before the lockdown (pre-lockdown EE) and again since the lockdown (lockdown EE). Four measures were used in the study, pre-lockdown EE, pre-lockdown UE and pre-lockdown CR and lockdown EE.
Coping strategies: The Brief Coping Inventory (Carver, 1997). The Brief COPE is a 28-item multidimensional measure of strategies that assess the frequency that people use different coping or regulating cognitions and behaviours in response to stressors. The Brief COPE is a frequently utilised, reliable instrument of measuring coping strategies (e.g. (Baumstarck et al., 2017; Yusoff, Low & Kip, 2010). Wang et al., 2018). It contains 14 subscales each with two items; (1) self-distraction, (2) active coping, (3) denial, (4) substance use, (5) use of emotional support, (6) use of instrumental support, (7) behavioural disengagement, (8) venting, (9) positive reframing, (10) planning, (11) humour, (12) acceptance, (13) religion, and (14) self-blame. In the present study, participants were asked to rate their use of coping strategies since the Covid 19 lockdown, on a Likert scale ranging from 1: ‘I haven't been doing this at all’, to 4: ‘I've been doing this a lot’, with a higher score indicating increased usage of that specific coping strategy.
Many researchers create factors from the Brief COPE, to identify styles of coping practices (e.g Woodhouse, Hebbard, & Knowles, 2018) and as this was an unusual, unprecedented event it was decided to carry this out statistically in the current study (Wang et al., 2018). A Principal Components factor analysis (PCA) with varimax rotation was carried out to create factors from the 14 coping strategies. Three of these factors had eigenvalues >1 and were used in subsequent analyses. Three strategies, substance use, religion and humour, did not load onto the factors and were excluded from further analysis. Factor 1 Adaptive coping (25.12% variance) contained the following subscales, with their loadings: Self distraction (0.60), active coping (0.79), positive reframe (0.70) and planning (0.73). Factor 2 Maladaptive coping (16.65% of variance) contained the following subscales: denial (0.71), self-blame (0.61), behavioural disengagement (0.79) and acceptance (reverse scored 0.59). Finally, Social support coping (8.64% of variance), containing the following subscales: Instrumental support (0.88), emotional support (0.85) and venting (0.49). All measures were converted to a mean score, with a higher score indicating higher coping strategies in that domain; Adaptive coping, Maladaptive coping, and Social support coping.
Health Anxiety: The Short Health Anxiety Inventory (SHAI) (Abramowitz, Deacon, and Valentiner (2007). The Short Health Anxiety Inventory (SHAI) has three subscales measuring cognitive factors typically associated with severe health anxiety; (1) perceived likelihood of becoming ill, (2) perceived severity of becoming ill and (3) body vigilance. The SHAI consists of 14 main items, each with four statements each scored from 0 to 3, with a higher score indicating higher health anxiety, for example: ‘I never have a serious illness’ (0), ‘I sometimes think I have a serious illness’(1), ‘I often think I have a serious illness’ (2) and ‘I usually think I have a serious illness’(3) and participants were required to indicate which statement applies to how they normally feel. In the present study this was used as a mean of all 14 items and was referred to as the health anxiety score. In addition, four further items (15–18) which form an additional subscale of the SHAI used in research studies (Alberts et al., 2013) were adapted to measure health anxiety in relation to COVID19, for example ‘If I had Covid 19 I would still enjoy things in my life (0)’. This was termed the Covid health anxiety score. The items were scored one directionally (with no reverse coded items) zero to three, with a higher score indicating higher levels of health anxiety. The SHAI is viewed as reliable and valid (Abramowitz et al., 2007; Salkovskis, Rimes, Warwick, & Clark, 2002). In the present study internal reliability was good for both the health anxiety score (α = 0.90) and the Covid health anxiety score (α = 0.78).
Food insecurity: The Food Insecurity Experience Scale (FIES) (Food & Agriculture Organization of the United States, 2015). The Food Insecurity Experience Scale (FIES) is a psychometric scale developed to assess the severity of food insecurity and accessibility of food at the individual and household level (FAO, 2015) which is well used and reliable (Cafiero, Melgar-Quinonez, Ballard, & Kepple, 2014; Jones, 2017). The FIES focuses on the subjective experiences associated with an increased difficulty in accessing food due to constraints on resources. The FIES consists of a statement ‘During the last 12 months, was there a time when, because of lack of money or other resources:’ and eight yes/no questions, for example, ‘Your household ran out of food?’, For the purposes of the present study, as the aim was to measure food insecurity since lockdown, the initial statement was changed to ‘Since the Covid 19 Lockdown, was there a time because of a lack of money or resources’. (Food & Agriculture Organisation of the United States, 2015). The food insecurity score was used in analyses as a continuous variable from 0 to 8, with a score of 8 indicating a high level of food insecurity. In addition a categorical score of food insecurity was used in demographic analyses of none (0), mild (score of 1–3) and moderate/severe (score 4+). The moderate and severe food insecure groups were combined as there was a low number of participants in the severe category (n = 6).
2.4. Procedure
Ethical clearance was granted by the the Health & Life Science Research and Ethics Committee of DeMontfort University, and adhered to guidelines of the British Psychological Society (BPS, 2013; BPS, 2014). A link to the study, which was conducted through Qualtrics, was posted on social media sites (Facebook, Twitter), and through snowball sampling. All of the data was collected in a one-month period, between 22nd April and 22nd May (weeks 5–9 of the lockdown). Informed consent was obtained at the beginning of the survey, and then participants answered a series of self-report questionnaires lasting approximately 20 minutes in duration. There was no renumeration for taking part, and participants were free to drop out at any time during the survey.
2.5. Data analysis
Kolmorgorov Smnirov tests for normality indicated that none of the variables were normally distributed (p<.05), so non-parametric tests were carried out where possible, and regression analyses were bootstrapped (N = 1000). Percentages were calculated for eating more than, the same as, or less than usual for the food groups (HED, home prepared, FV). One-way chi-square tests were used to examine whether individuals were more likely to be eating more than vs. less than/the same as, after lockdown compared to their usual eating behaviour. Preliminary analyses were carried out to examine whether the demographic variables of, employment, isolating in house, sex, age, BMI, shopping behaviour, living with children, and ethnicity, were associated with the dependent variables (HED, FV, Home prepared and lockdown EE) (see Table 1). Spearman rank correlations were carried out to examine associations between changes to food intake (HED, FV, Home prepared and lockdown EE) and BMI, coping strategies, health anxiety and food insecurity (see Table 2 ). A bonferroni adjustment was applied to the correlational analyses, with p < .001 as the threshold for acceptance. Four multiple hierarchical regression analyses were carried out to examine associations with 1) HED consumption 2) FV consumption 3) Home prepared food consumption and 4) Lockdown EE. Each model was built individually on the basis of associations with the dependent variable identified in preliminary analyses (at p < .05 threshold). Each model had a similar structure of entering variables into the regression analysis. In step 1 of the analysis, demographic variables (BMI, isolating in house, sex, age, shopping behaviour, ethnicity, employment) were entered when they were associated with the dependent variable (lockdown EE, HED, FV or home prepared food intake see Table 1). In step 2 of the analysis, health anxiety, pre-lockdown eating behaviours and food insecurity were entered if they had been associated with the dependent variable (see Table 2). Finally, in step 3, coping strategies were entered into the model if they had been associated with the dependent variable (see Table 2). Preliminary analyses found that EE was strongly associated with both BMI and maladaptive coping strategies. Therefore, a moderation regression analysis using Haynes (2013) Process MACRO with bootstrapped confidence intervals (5000 iterations) was carried out to examine the relationship between BMI and EE during lockdown was moderated by maladaptive coping strategies after controlling for pre lockdown EE.
Table 2.
Associations between BMI, baseline eating behaviour and perceived changes in food consumption in a sample of 620 adults during lockdown.
| HED foods | Home prepared | Fruit and vegetables | EE Lockdown | Alcohol | |
|---|---|---|---|---|---|
| BMI (kg/m2) | 0.12 | −0.03 | −0.05 | 0.37** | −0.02 |
| Baseline Emotional eating | 0.32** | 0.08 | −0.14** | 0.86** | −0.08 |
| Baseline Uncontrolled eating | 0.33** | 0.09 | −0.14** | 0.67** | 0.04 |
| Baseline dietary restraint | 0.00 | 0.03 | 0.02 | 0.05 | 0.04 |
| Food insecurity | −0.04 | −0.11 | −0.11 | 0.10 | −0.13 |
| Health anxiety | 0.10 | 0.09 | −0.07 | 0.22** | 0.09 |
| Health anxiety Covid | 0.13 | −0.08 | 0.05 | 0.30** | −0.10 |
| Adaptive coping | 0.04 | 0.20** | 0.15** | 0.01 | −0.01 |
| Maladaptive coping | 0.13** | 0.06 | −0.08 | 0.33** | 0.07 |
| Social support coping | 0.12 | 0.01 | 0.08 | 0.18** | 0.10 |
**p < .001.
aChange in consumption was scored from -2-2, where a positive score indicated eating more of the food, 0 indicated eating the same and a negative score indicated eating less than usual.
3. Results
3.1. Perceived changes to eating during lockdown
It was found that there were some differences in eating behaviour according to demographic characteristics in the sample (see Table 1). Woman were more likely to report higher EE scores, t(639) = −5.62, p < .001, and increases to their HED intake, t(639) = −3.50, p<.001, when compared to men. In addition, those isolating at home were more likely to report higher EE scores than those who were not, t(639) = 2.42, p < .001. Across the sample as a whole, there was a significant decrease in reported EE after lockdown had been implemented, M = 6.96 (2.90), compared to before lockdown had been implemented, M = 7.49 (2.77), t(639) = 8.63, p<.001. Food insecurity status during the lockdown (moderate vs none) was associated with lower FV consumption, F(2, 638) = 3.16, p<.05, and higher lockdown EE, F(2, 638) = 3.61, p<.05. Finally, the ability to do your own shopping was associated with increased HED intake, t(639) = −1.96, p<.05. There were no differences in eating behaviour according to employment status or ethnicity across the sample.
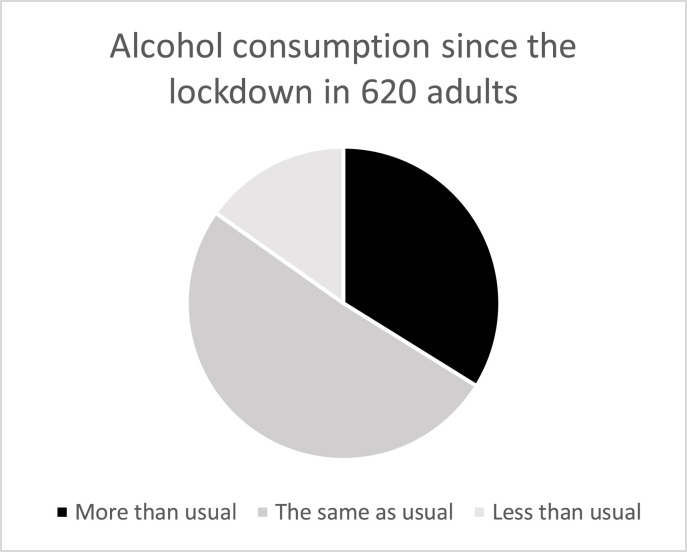
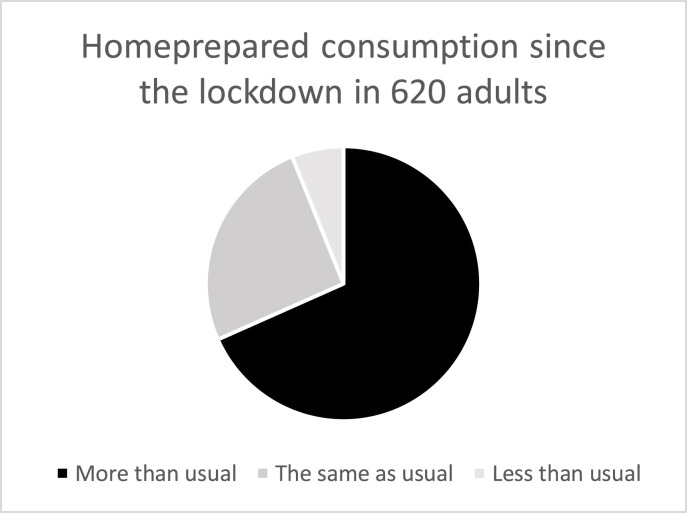
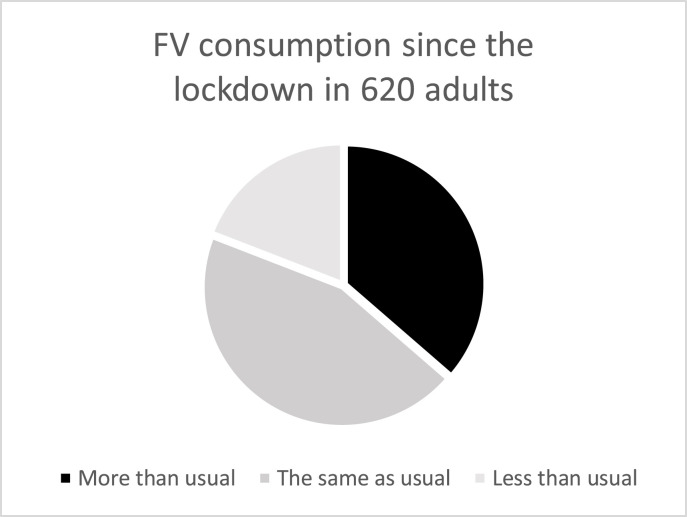
Across the sample, there were reported changes to consumption in the different food groups. When comparing whether individuals ate more of a food group during lockdown compared to eating less or the same, it was found there were differences in HED food intake, alcohol intake, FV intake, and homemade food intake (sees Fig. 1, Fig. 2, Fig. 3, Fig. 4 ). Individuals were more likely to report increases in the consumption of HED snacks and home prepared foods (p<.001), and report consuming less or the same, alcohol and FV (p<.001).
Fig. 1.
Self reported changes to food consumption during Lockdown in a sample of 620 adults.
Fig. 2.
Self reported changes to food consumption during Lockdown in a sample of 620 adults.
Fig. 3.
Self reported changes to food consumption during Lockdown in a sample of 620 adults.
Fig. 4.
Self reported changes to food consumption during Lockdown in a sample of 620 adults.
There were associations between perceived changes in food consumption since the lockdown, and the other variables measured in the study (Table 2). A higher BMI was associated EE during the lockdown. Pre-lockdown reported eating styles of EE and uncontrolled eating were associated with higher HED consumption, lower FV consumption and higher EE during the lockdown, however pre lockdown dietary restraint was not associated with any of the consumption variables.
3.2. Associations with perceived changes to food consumption during lockdown
3.2.1. HED consumption
A hierarchical regression analysis was carried out to examine the effects of demographic factors (sex, isolating in the house, BMI, shopping behaviour), (step 1) health anxiety, pre lockdown eating behaviour (step 2) and maladaptive coping (step 3) on increased HED consumption (see Table 3 ). In the first step of the model it was found that being female, having a higher BMI and doing your own shopping was consistently associated with higher HED intake during the lockdown. In step 2 higher BMI no longer accounted for variance but pre lockdown eating variables (EE and uncontrolled eating) and Covid health anxiety were associated with higher HED consumption. In the final model, being female, doing your own shopping, higher Covid health anxiety, higher pre lockdown EE and higher pre lockdown uncontrolled eating accounted for variance in higher HED consumption. Maladaptive coping did not account for any variance in the model. The regression equation formed a good fit with the data F(9, 518) = 10.61, p<.001 which accounted for 14% of the variance in increases in HED consumption during the lockdown (R2 Adj. = 0.14).
Table 3.
Associations with perceived changes in consumption of HED foods during lockdown in a sample of 620 adults in the UK.
| Model 1 B, CIa | Model 2 B, CIb | Model 3 B, CIc | |
|---|---|---|---|
| Sex1 | −0.45(-0.70, -0.19) | −0.30(-0.55, -0.03) | −0.30(-0.55, -0.02) |
| Isolating in house2 | 0.07(-0.15, 0.28) | 0.00(-0.19, 0.20) | 0.00(-0.20, 0.20) |
| BMI | 0.02(0.01, 0.04) | 0.02(0.01, 0.04) | <0.01(-0.01, 0.02) |
| Shopping 3 | 0.18(0.00, 0.40) | 0.22(0.02, 0.43) | 0.20(0.01, 0.40) |
| Children in the house4 | 0.17(-0.02, 0.35) | 0.16(-0.02, 0.33) | 0.16(-0.01, 0.33) |
| Covid Health anxiety | 0.05(0.02, 0.07) | 0.04(0.01, 0.07) | |
| Baseline EE | 0.05(0.01, 0.09) | 0.05(0.01, 0.09) | |
| Baseline Uncontrolled eating | 0.03(0.01, 0.06) | 0.03(0.01, 0.06) | |
| Maladaptive coping | 0.00(-0.01, 0.04) |
Codes for categorical predictor variables: 1 Male = 0, female = 1, 2 not isolating = 0 Isolating = 1, 3 delivery or food parcels = 0, own shopping = 1, 4Children in the house no = 0, yes = 1.
F(3, 614) = 8.20, p<.001, Adj. R2 = 0.04.
F change(2, 612) = 6.41, p<.05, Adj. R2 = 0.06.
F change(2, 610) = 13.89, p<.001, Adj. R2 = 0.15.
3.2.2. FV consumption
A hierarchical regression analysis was carried out to examine the effects of food security, pre lockdown eating behaviour (EE and uncontrolled eating) in step 1, and adaptive coping in step 2 on higher FV consumption during the lockdown(see Table 3). It was found that only higher adaptive coping strategies accounted for variance in increases in FV consumption, F(4, 557) = 3.07, p < .01 which accounted for 3% of the variance in higher FV consumption during lockdown (R2 Adj. = 0.03).
3.2.3. Home prepared consumption
A hierarchical regression analysis was carried out to examine the effects of age (step 1), health anxiety, food security, pre lockdown EE and pre lockdown uncontrolled (step 2), and adaptive coping (step 3) on higher home prepared food consumption during the lockdown (see Table 4 ). It was found that being younger was consistently associated with an increase in home prepared consumption during the lockdown. In the final model, younger age, higher pre lockdown emotional eating, and higher adaptive coping strategies accounted for variance in home prepared food consumption. The regression equation formed a good fit with the data F(5, 538) = 5.87, p<.001 Adj. R2 = 0.04, which accounted for 4% of the variance in higher home prepared consumption during the lockdown.
Table 4.
Associations between perceived changes in consumption of fruits and vegetables during lockdown in a sample of 620 adults in the UK.
| Model 1 B, CIa | Model 2 B, CIb | |
|---|---|---|
| Baseline EE | −0.01(-0.05, 0.03) | −0.01(-0.05, 0.03) |
| Baseline uncontrolled eating | 0.01(-0.04, 0.01) | −0.02(- 0.02, 0.01) |
| Food insecurity | −0.05(-0.11, 0.01) | −0.05(-0.11, 0.01) |
| Adaptive coping | 0.02(0.01, 0.03) |
Model 1F(3, 616) = 4.04, p<.05, Adj. R2 = 0.02.
Model 2, F change(1, 615) = 7.74, p<.01, Adj. R2 = 0.03.
3.3. Associations with EE during the lockdown
A hierarchical regression analysis was carried out to examine the effects of demographic factors (sex, BMI, isolating in the house), health anxiety, food security, pre lockdown EE, and maladaptive coping on the variance in reported EE during the lockdown (see Table 5 ). It was found that having a higher BMI was consistently associated with EE during the lockdown, whereas sex and isolating in the house (yes/no) did not account for variance in the model. In the final model, BMI, pre lockdown emotional eating and maladaptive coping strategies accounted for variance in emotional eating during the lockdown. The regression equation formed a good fit with the data F(9, 510) = 172.99, p<.001, which accounted for 76% of the variance in emotional eating during lockdown (R2 Adj. = 0.76) (Table 6).
Table 5.
Associations between perceived changes in consumption of home prepared foods during lockdown in a sample of 620 adults in the UK.
| Model 1 B, CIa | Model 2 B, CIb | Model 3 B, CIc | |
|---|---|---|---|
| Age | −0.01(-0.02, -0.002) | −0.01(-0.02, -0.002) | −0.01(-0.02, -0.001) |
| Baseline Emotional eating | 0.01(-0.03, 0.06) | 0.03(0.00, 0.07) | |
| Baseline uncontrolled eating | |||
| Health anxiety | 0.00(-0.01, 0.02) | 0.00(- 0.01, 0.02) | |
| Food insecurity | −0.06(-0.13, 0.02) | −0.06(-0.13, 0.02) | |
| Adaptive coping | 0.03(0.01, 0.04) |
Model 1 F(1, 618) = 8.07, p<.01 Adj. R2 = 0.01.
Model 2 F change(3, 614) = 2.74, p < .05 Adj R2 = 0.02.
Model 3 F change(1, 613) = 12.60, p < .001 Adj. R2 = 0.03.
Table 6.
Associations with emotional eating during lockdown in a sample of 620 adults in the UK.
| Model 1 B, CIa | Model 2 B, CIb | Model 3 B, CIc | |
|---|---|---|---|
| Sex1 | −1.66(-2.42, -0.89) | −0.16(-0.65, 0.28) | −0.06 (−0.52, 0.37) |
| Isolating in house2 | 0.27 (−0.50, 1.10) | 0.25(-0.22, 0.73) | 0.36(-0.10, 0.81) |
| BMI | 0.18(0.13, 0.23) | 0.02(-0.01, 0.05) | 0.03(-0.01, 0.06) |
| Occupation3 | 0.46(-0.09, 0.97) | 0.17(-0.12, 0.47) | 0.12(-0.16, 0.41) |
| Baseline Emotional eating | 0.84(0.75, 0.92) | 0.80(0.71, 0.89) | |
| Baseline uncontrolled eating | 0.03(-0.01, 0.08) | 0.03(-0.01, 0.07) | |
| Covid Health anxiety | −0.01(-0.01, 0.05) | −0.04(- 0.10, 0.03) | |
| Food insecurity | 0.01(-0.12, 0.10) | −0.05(-0.18, 0.05) | |
| Maladaptive coping | 0.12(0.07, 0.17) | ||
Codes for categorical predictor variables: 1 male = 0, female = 1, 2 not isolating = 0 isolating = 1, 3professional/managerial = 0, other = 1.
Model 1 F(4, 611) = 23.03, p < .001, Adj. R2 = 0.18.
Model 2 F change(4, 605) = 136.81, p < .001 Adj. R2 = 0.73.
Model 3 F change(1, 604) = 26.26, p < .001 Adj. R2 = 0.75.
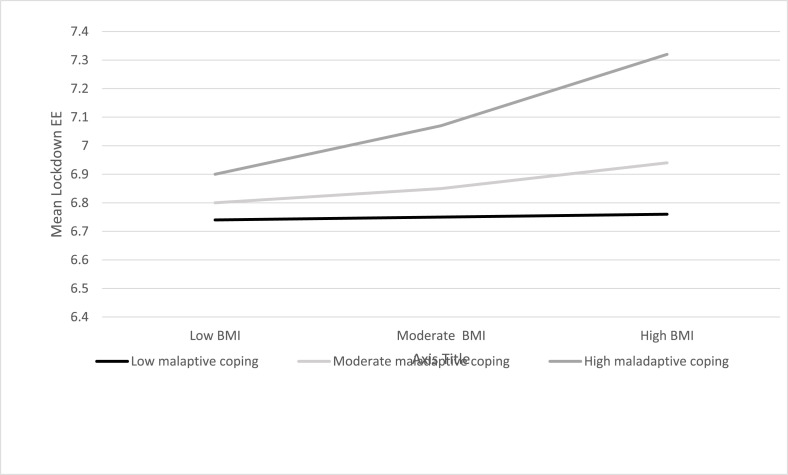
Maladaptive coping moderated the relationship between BMI and EE during the lockdown (B = 0.02, 95% CI < 0.00, 0.04) after controlling for pre lockdown emotional eating (see Fig. 5 ), which explained R2 = 75.8% of the variance in EE during the lockdown. The effect was conditional on the moderator at high levels of maladaptive coping. In particular, those with a higher BMI and higher maladaptive coping strategies had higher EE during the lockdown, after controlling for pre-lockdown EE.
Fig. 5.
Maladapative coping moderates the relationship between BMI and EE during Lockdown, after controlling for baseline EE.
4. Discussion
The main aim of the present study was to examine self-perceptions of changes to food consumption and eating behaviour during the lockdown in the UK. In particular, we wanted to examine whether environmental changes such as accessing foods, and shielding, pre-lockdown eating behaviour, BMI and health anxiety were associated with changes to eating, and whether coping strategies during lockdown could explain reported changed eating behaviour. Perceived increases in eating behaviour were reported by many individuals, and these related to both healthy and unhealthy eating patterns. Several baseline variables were associated with perceived changes to eating, and changes to eating were associated with health anxiety about Covid, pre-lockdown eating behaviours, and both adaptive and maladaptive coping strategies.
4.1. HED foods
In the current study it was found that less healthy eating patterns such as eating HED foods were more common in individuals who were female, who had a higher BMI, did their own food shopping, who had high baseline tendencies to overeat, and had higher health anxiety. Although increases in HED foods was associated with BMI, this association was accounted for by pre-lockdown EE and uncontrolled eating. This is similar to recent research findings conducted prior to the pandemic, that increases in snack consumption are related to BMI through increased emotional eating behaviours (Czepczor-Bernat & Brytek-Matera, 2020). Mood induction experiments have shown that negative mood inductions can lead to increased snack food consumption in those with baseline eating problems (Cardi, Leppanen, & Treasure, 2015). This suggests that certain individuals may turn to HED foods in times of stress, especially if they tend to overeat in response to their emotions (Michels, Man, Vinck, & Verbeyst, 2020). It is likely that there are a cluster of eating behaviours which are known to be associated with overweight, and consequences of the pandemic such as being at home for longer time periods and anxiety about health, may trigger eating episodes in those vulnerable individuals. Thus, a pandemic situation and lockdown creates a perfect storm for certain at-risk individuals.
4.2. EE
EE, that some individuals will change their eating in response to emotions, is a well-recognised concept however the processes through which EE works are not fully understood and variable. Macht (2008), proposed that emotions affect eating in a variety of ways, one of which is eating to regulate emotions. The level of arousal may affect intake, with very high stress being associated with undereating and lower stress being associated with overeating. In addition, individuals react differently to each given emotion, for example those with a higher BMI are more likely to eat food to regulate mood in times of stress (Robinson et al., 2020). In the present study EE at pre-lockdown was associated with multiple food intake changes, including higher HED snack intake and lower FV consumption. Although there was a change in EE behaviour across the sample as a whole, it was not in the expected direction, with many participants reporting a decrease in EE after the implementation of lockdown compared to their behaviour prior to lockdown. We found that EE before and after lockdown were strongly associated with each other, suggesting some continuity in this behaviour over time and disruptive events. This is very similar to findings by Kuijer and Boyce (2012), who did not find a change in EE following an earthquake in Christchurch, NZ, across their sample as a whole. They found that anxiety about the disaster did moderate the relationship between EE before and after the earthquake, suggesting that what is crucial is how individuals respond to the disaster. Other research has found that individuals with a higher BMI are particularly at risk from problematic eating during the Covid 19 pandemic (Robinson et al., 2020). In the current study health anxiety was not associated with EE after controlling for pre lockdown EE. However, it was found that the relationship between BMI and EE during lockdown was moderated by maladaptive coping strategies. In particular, it was found that higher maladaptive coping and a higher BMI at pre lockdown, were associated with higher EE during lockdown. This suggests that some individuals may be more at risk of adopting unhealthy eating practices during lockdown, and these may be part of a wider adoption of maladaptive coping strategies. Research following pandemics has found that anxiety and health anxieties are common (Jalloh et al., 2018) and are associated with maladaptive coping strategies (Jungmann & Witthöft, 2020). Interestingly, maladaptive coping strategies, which included the subscales behavioural disengagement, self-blame and low acceptance, were associated with emotional and uncontrolled eating prior to lockdown. This suggests that these eating behaviours are part of a wider set of coping strategies, whereby, these types of eating behaviours may be part of a toolbox of maladaptive coping strategies, which worsen behaviours in time of distress (Cheng et al., 2014; Van den Tol et al., 2018). Evers et al. (2010) found that individuals who were asked to supress cognitions, which is viewed as a maladaptive strategy, ate more foods following an emotion induction than those using other strategies. This suggests that maladaptive cognitions may be a precursor to both emotional eating and poor coping strategies in times of stress (Gibson, 2012).. It would be interesting to ascertain whether adjusting cycles of maladaptive coping, and replacing them with adaptive coping strategies, would be the most effective way of ensuring healthy eating behaviours during these periods. It was found that those who were shielded in their homes without access to walks or shops were more likely to show an increase in EE post lockdown. We think that reduction in exercise in those who were shielding, and the increased time spent in the home with easy access to foods may have both played a role in changes to eating.
4.3. Influences on positive eating behaviours
There were associations with increases in positive eating behaviours during lockdown. Generally, increases in eating FV and home prepared foods, both of which are viewed as positive dietary choices, were associated with decreased food insecurity and increased adaptive coping styles. Home cooking has been associated with greater time availability, which along with reduced access to meals from outside sources as they were shut (Nicola et al., 2020), may have partially accounted for the large increase in home cooking (Mills et al., 2017). Cooking was slightly more prevalent in individuals with higher pre lockdown EE. This could be because emotional eating is associated with nostalgia and comfort, which may increase baking and preparation of food in some individuals (Locher, Yoels, Maurer, & Ells, 2005). The transition to home preparation of foods through baking and cooked meals is a positive outcome of the lockdown experience, as there have been reported decreases to cooking skills and activities across the UK in recent decades (Cheng, Olsen, Southerton, & Warde, 2007). It is likely that self-care, in terms of eating, exercising and sleeping well, are part of a collection of adaptive coping strategies that will support individuals in times of difficulty. It would be interesting to examine whether increases to cooking and baking behaviour observed in this study will become habitual and remain higher after lockdown, or whether individuals will readjust to the loosening of the lockdown regulations and the reopening of food and catering establishments.
4.4. Food insecurity
Food insecurity studies have found consistently that food insecurity is associated with a poor dietary pattern, which some researchers have attributed to over consuming when food is available to compensate for inconsistent access to food (Stinson et al., 2018). It is also likely that those who are food insecure cannot afford fruits and vegetables, which are more expensive whilst less calorific and thereby less filling (Drisdelle et al., 2020). It is known that food insecurity increased dramatically during the lockdown, particularly for those who were food insecure prior to the lockdown and experienced economic hardship (Barker & Russell, 2020; Loopstra, 2020). However, there was an additional group of individuals, particularly those who were vulnerable to the virus, were not able to secure home deliveries nor leave their houses to shop. Although we measured employment status, and whether this had changed as a consequence of lockdown, we did not measure whether individuals were food insecure prior to lockdown. We adjusted the food insecurity measure to just refer to post-lockdown access to food, which would be a transient problem caused by the unusual circumstances which meant that food was hard to obtain safely in the short term, rather than the individual being unable to afford food. In addition, as distribution networks improved, it is likely that those isolating who were food insecure at the beginning of lockdown, would have become less so as lockdown progressed (Nicola et al., 2020). It would have been interesting to track this longitudinally. As this was a cross sectional study and we had no pre lockdown measures of food insecurity, there are limitations to the conclusions that can be made about food insecurity in this sample.
4.5. Limitations
There were some limitations to the present research. Our sample was not representative of the UK population, as it was overwhelmingly female, majority white-British, and working from home. This is a consequence of the sampling method, which was mainly through social media sites, and is similar to other lockdown studies (eg Robinson et al., 2020). At the time of recruitment it was unknown that both men and BAME populations would be disproportionately at risk of severe reactions to the virus, and it would have been interesting to examine differences in stress and eating according to sex and ethnic origin, yet our unequal demographic data made this difficult. All participants completed all of the measures during lockdown, as we did not have access to baseline data prior to the lockdown event (Kuijer & Boyce, 2012). Recent research into disordered eating has also used similar perceived change measures, and we argue it is a pragmatic solution to conducting research with a large sample in relation to an unexpected event (Phillipou et al., 2020). It is important to note that during a pandemic, restrictions and regulations around working conditions, social interactions, as well as access to shops/food, are dynamic depending on the infection rate. All our data was collected between the dates of 22nd April and 22nd May, approximately 4 weeks after the start of lockdown. This was relatively early in the lockdown which started to ease more substantially in early July 2020. The government's advice did not change during this time period, and it is likely that there was some consistency in eating behaviour across this period. However, those who had been unable to access food during the early part of lockdown did gradually gain access to foods (Nicola et al., 2020). Previous research has found that the initial period of a pandemic is one of anxiety and poor emotional regulation, which is replaced by more adaptive cognitive risk evaluation as more is known about the scale and spread of the virus (Liao et al., 2014). Death and infection rates from Covid 19 were increasing rapidly during the period of April–May 2020 in the UK, and it is likely that patterns of perceived eating behaviour reflected this feeling of uncertainty and anxiety. One limitation of our research, was that we did not measure financial or economic stress, as it was unclear at that time how devasting the effect would be on income and job security across the UK. Future research should adopt a longitudinal approach to examine changes in eating as a consequence of changing restrictions, a variety of social, economic and health stressors, and infection rate.
5. Conclusions
Overall, our findings demonstrate that the unique environmental and psychological factors experienced by individuals whilst experiencing lockdown during the Covid 19 pandemic, led to changes in eating behaviour. It was apparent that pre lockdown tendencies to overeat and higher BMI coupled with maladaptive coping strategies were associated with increases to EE consumption. Adaptive coping strategies were associated with increased home cooking and FV consumption. This is the first study to show that eating behaviours during the pandemic were associated with adoption of coping strategies, leading to the possibility of recommendations and guidance about future lockdowns. It is clear that certain individuals, who already have problematic eating and high BMI may need to be supported more to adopt healthy coping practices.
Ethics disclosure
This study was granted ethical approval by the Health & Life Sciences Faculty Research Ethics Committee, De Montfort University, Application number 3599, April 2020.
All participants gave informed consent prior to data collection, and ethical standards of confidentiality and anonymity were upheld at all times in the research process.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.appet.2020.105082.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Abramowitz J.S., Deacon B.J., Valentiner D.P. The Short Health Anxiety Inventory: Psychometric properties and construct validity in a non-clinical sample. Cognitive Therapy and Research. 2007;31(6):871–883. doi: 10.1007/s10608-006-9058-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alberts N.M., Hadjistavropoulos H.D., Jones S.L., Sharpe D. The short health anxiety inventory: A systematic review and meta-analysis. Journal of Anxiety Disorders. 2013;27(1):68–78. doi: 10.1016/j.janxdis.2012.10.009. [DOI] [PubMed] [Google Scholar]
- Alias N.A., Nor N.M. Measurement needs of food security during flood disaster in bera, pahang. Current Research in Nutrition and Food Science Journal. 2018;6(1):83–88. doi: 10.12944/CRNFSJ.6.1.08. [DOI] [Google Scholar]
- Barker M., Russell J. Feeding the food insecure in britain: Learning from the 2020 COVID-19 crisis. Food Sec. 2020;12:865–870. doi: 10.1007/s12571-020-01080-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baumstarck K., Alessandrini M., Hamidou Z., Auquier P., Leroy T., Boyer L. Assessment of coping: A new French four-factor structure of the brief COPE inventory. Health and Quality of Life Outcomes. 2017;15(1):8. doi: 10.1186/s12955-016-0581-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett J., Greene G., Schwartz-Barcott D. Perceptions of emotional eating behavior. A qualitative study of college students. Appetite. 2013;60:187–192. doi: 10.1016/j.appet.2012.09.023. [DOI] [PubMed] [Google Scholar]
- Braden A.D., Watford T., Emley E. Eating when depressed, anxious, bored, or happy: Are emotional eating types associated with unique psychological and physical health correlates? Appetite. 2018;125:410–417. doi: 10.1016/j.appet.2018.02.022. [DOI] [PubMed] [Google Scholar]
- British Psychological Society . 2013. Ethics guidelines for internet-mediated research. Leicester, UK: Author. [Google Scholar]
- British Psychological Society . 2014. Code of human research ethics. Leicester, UK: Author. [Google Scholar]
- Cafiero C., Melgar-Quinonez H.R., Ballard T.J., Kepple A.W. Validity and reliability of food security measures. Annals of the New York Academy of Sciences. 2014;1331(1):230–248. doi: 10.1111/nyas.12594. [DOI] [PubMed] [Google Scholar]
- Cardi V., Leppanen J., Treasure J. The effects of negative and positive mood induction on eating behaviour: A meta-analysis of laboratory studies in the healthy population and eating and weight disorders. Neuroscience & Biobehavioral Reviews. 2015;57:299–309. doi: 10.1016/j.neubiorev.2015.08.011. [DOI] [PubMed] [Google Scholar]
- Carver C.S. You want to measure coping but your protocol ‘too long: Consider the brief cope. International Journal of Behavioral Medicine. 1997;4(1):92. doi: 10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- Cheng C., Lau H.P.B., Chan M.P.S. Coping flexibility and psychological adjustment to stressful life changes: A meta-analytic review. Psychological Bulletin. 2014;140(6):1582. doi: 10.1037/a0037913. [DOI] [PubMed] [Google Scholar]
- Cheng S.L., Olsen W., Southerton D., Warde A. The changing practice of eating. Evidence from UK time diaries, 1975 and 2000. British Journal of Sociology. 2007;58(1):39–61. doi: 10.1111/j.1468-4446.2007.00138.x. [DOI] [PubMed] [Google Scholar]
- Cowling B.J., Ng D.M., Ip D.K., Liao Q., Lam W.W., Wu J.T., et al. Community psychological and behavioral responses through the first wave of the 2009 influenza A (H1N1) pandemic in Hong Kong. The Journal of Infectious Diseases. 2010;202(6):867–876. doi: 10.1086/655811. [DOI] [PubMed] [Google Scholar]
- Czepczor-Bernat K., Brytek-Matera A. The impact of food-related behaviours and emotional functioning on body mass index in an adult sample. Eating and Weight Disorders-Studies on Anorexia, Bulimia and Obesity. 2020:1–7. doi: 10.1007/s40519-020-00853-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Renzo L, Gualtieri P, Pivari F, et al. Eating habits and lifestyle changes during COVID-19 lockdown: an Italian survey. Journal of Translational Medicine. 2020;18:229. doi: 10.1186/s12967-020-02399-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drisdelle C., Kestens Y., Hamelin A.-M., et al. Disparities in access to healthy diets: How food security and food shopping behaviors relate to fruit and vegetable intake. Journal Of The Academy Of Nutrition And Dietetics, . 2020;120(11):1847–1858. doi: 10.1016/j.jand.2020.03.020. [DOI] [PubMed] [Google Scholar]
- Dryhurst S., Schneider C.R., Kerr J., Freeman A.L., Recchia G., Van Der Bles A.M., et al. Risk perceptions of COVID-19 around the world. Journal of Risk Research. 2020:1–13. doi: 10.1080/13669877.2020.1758193. [DOI] [Google Scholar]
- Dubé L., LeBel J.L., Lu J. Affect asymmetry and comfort food consumption. Physiology & Behavior. 2005;86:559–567. doi: 10.1016/j.physbeh.2005.08.023. [DOI] [PubMed] [Google Scholar]
- Evers, Dingemans, Junhans, Boevé Feeling bad or feeling good, does emotion affect your consumption of food? A meta-analysis of the experimental evidence. Neuroscience & Biobehavioral Reviews. 2018;92:195–208. doi: 10.1016/j.neubiorev.2018.05.028. [DOI] [PubMed] [Google Scholar]
- Evers C., Stok F.M., De Ridder D.T.D. Feeding your feelings: Emotion regulation strategies and emotional eating. Personality and Social Psychology Bulletin. 2010;36(6):792–804. doi: 10.1177/0146167210371383. [DOI] [PubMed] [Google Scholar]
- 2015. http://www.fao.org/3/a-i4646e.pdf
- Gibson E.L. The psychobiology of comfort eating: Implications for neuropharmacological interventions. Behavioural Pharmacology. 2012;23(5–6):442–460. doi: 10.1097/FBP.0b013e328357bd4e. [DOI] [PubMed] [Google Scholar]
- Gov.UK Coronavirus (Covid 19) advice and support. 2020. https://www.gov.uk/coronavirus Retrieved from.
- Greeno C.G., Wing R.R. Stress-induced eating. Psychological Bulletin. 1994;115(3):444–464. doi: 10.1037/0033-2909.115.3.444. [DOI] [PubMed] [Google Scholar]
- Hanson K.L., Connor L.M. Food insecurity and dietary quality in US adults and children: A systematic review. American Journal of Clinical Nutrition. 2014;100(2):684–692. doi: 10.3945/ajcn.114.084525. [DOI] [PubMed] [Google Scholar]
- Hawkins L.K., Farrow C, Thomas J.M. Do perceived norms of social media users’ eating habits and preferences predict our own food consumption and BMI? Appetite. 2020;149:104611. doi: 10.1016/j.appet.2020.104611. [DOI] [PubMed] [Google Scholar]
- Hayes A.F. Guilford Press; New York, NY: 2013. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. [Google Scholar]
- Jalloh M.F., Li W., Bunnell R.E., Ethier K.A., O'Leary A., Hageman K.M., et al. Impact of Ebola experiences and risk perceptions on mental health in Sierra Leone, July 2015. BMJ global health. 2018;3(2) doi: 10.1136/bmjgh-2017-000471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones A.D. Food insecurity and mental health status: A global analysis of 149 countries. American Journal of Preventive Medicine. 2017;53(2):264–273. doi: 10.1016/j.amepre.2017.04.008. [DOI] [PubMed] [Google Scholar]
- Jungmann S.M., Witthöft M. Health anxiety, cyberchondria, and coping in the current COVID-19 pandemic: Which factors are related to coronavirus anxiety? Journal of Anxiety Disorders. 2020;73:102239. doi: 10.1016/j.janxdis.2020.102239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ko C.H., Yen C.F., Yen J.Y., Yang M.J. Psychosocial impact among the public of the severe acute respiratory syndrome epidemic in Taiwan. Psychiatry and Clinical Neurosciences. 2006;60(4):397–403. doi: 10.1111/j.1440-1819.2006.01522.x. [DOI] [PubMed] [Google Scholar]
- Kuijer R.G., Boyce J.A. Emotional eating and its effect on eating behaviour after a natural disaster. Appetite. 2012;58(3):936–939. doi: 10.1016/j.appet.2012.02.046. [DOI] [PubMed] [Google Scholar]
- de Lauzon B., Monique R., Deschamps V., Lafay L., Borys J.M., Karlsson J., et al. Fleurbaix Laventie Ville Sante (FLVS) Study Group The Three-Factor Eating Questionnaire-R18 is able to distinguish among different eating patterns in a general population. Journal of Nutrition. 2004;134(9):2372–2380. doi: 10.1093/jn/134.9.2372. [DOI] [PubMed] [Google Scholar]
- Liao Q., Cowling B.J., Lam W.W., Ng D.M., Fielding R. Anxiety, worry and cognitive risk estimate in relation to protective behaviors during the 2009 influenza A/H1N1 pandemic in Hong Kong: Ten cross-sectional surveys. BMC Infectious Diseases. 2014;14(1):169. doi: 10.1186/1471-2334-14-169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Locher J., Yoels W.C., Maurer D., Ells J.V. Comfort foods: An exploratory journey into the social and emotional significance of food. Food and Foodways. 2005;13:273–297. doi: 10.1080/07409710500334509. [DOI] [Google Scholar]
- Loopstra R. Vulnerability to food insecurity since the Covid 19 pandemic: A preliminary report. 2020. https://foodfoundation.org.uk/wp-content/uploads/2020/04/Report_COVID19FoodInsecurity-final.pdfulnerability
- Macht M. How emotions affect eating: A five-way model. Appetite. 2008;50(1):1–11. doi: 10.1016/j.appet.2007.07.002. [DOI] [PubMed] [Google Scholar]
- Macht M., Dettmer D. Everyday mood and emotions after eating a chocolate bar or an apple. Appetite. 2006;46:332–336. doi: 10.1016/j.appet.2006.01.014. [DOI] [PubMed] [Google Scholar]
- Marty L., de Lauzon-Guillain B., Labesse M., Nicklaus S. Food choice motives and the nutritional quality of diet during the Covid 19 Lockdown in France. Appetite. 2021;157 doi: 10.1016/j.appet.2020.105005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mello J.A., Gans K.M., Risica P.M., Kirtania U., Strolla L.O., Fournier L. How is food insecurity associated with dietary behaviors? An analysis with low income, ethnically diverse participants in a nutrition intervention study? Journal of the American Dietetic Association. 2010;110(12):1906–1911. doi: 10.1016/j.jada.2010.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michels N., Man T., Vinck B., Verbeyst L. Dietary changes and its psychosocial moderators during the university examination period. European Journal of Nutrition. 2020;59(1):273–286. doi: 10.1007/s00394-019-01906-9. [DOI] [PubMed] [Google Scholar]
- Mills S., White M., Brown H., Wrieden W., Kwasnicka D., Halligan J., et al. Health and social determinants and outcomes of home cooking: A systematic review of observational studies. Appetite. 2017;111:116–134. doi: 10.1016/j.appet.2016.12.022. [DOI] [PubMed] [Google Scholar]
- Nguyen-Rodriguez S.T., Chou C.-P., Unger J.B., Spruijt-Metz D. BMI as a moderator of perceived stress and emotional eating in adolescents. Eating Behaviors. 2008;9(2):238–246. doi: 10.1016/j.eatbeh.2007.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicola M., Alsafi Z., Sohrabi C., Kerwan A., Al-Jabir A., Iosifidis C., et al. The socio-economic implications of the coronavirus pandemic (COVID-19): A review. International Journal of Surgery (London, England) 2020;78:185. doi: 10.1016/j.ijsu.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Office for National Statistics . Palgrave Macmillan; Basingstoke: 2010. Standard occupational classification 2010. [Google Scholar]
- Péneau S., Menard E., Mejean C., Bellisle F., Hercberg S. Sex and dieting modify the association between emotional eating and weight status. American Journal of Clinical Nutrition. 2013;97(6):1307–1313. doi: 10.3945/ajcn.112.054916. [DOI] [PubMed] [Google Scholar]
- Peng E.Y.C., Lee M.B., Tsai S.T., Yang C.C., Morisky D.E., Tsai L.T., et al. Population-based post-crisis psychological distress: An example from the SARS outbreak in taiwan. Journal of the Formosan Medical Association. 2010;109(7):524–532. doi: 10.1016/S0929-6646(10)60087-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillipou A., et al. Eating and exercise behaviors in eating disorders and the general population during the COVID ‐19 pandemic in Australia: Initial results from the COLLATE project. International Journal of Eating Disorders. 2020 doi: 10.1002/eat.23317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson E., Boyland E., Chisholm A., Harrold J., Maloney N.G., Marty L., et al. Obesity, eating behavior and physical activity during COVID-19 lockdown: A study of UK adults. Appetite. 2020 doi: 10.1016/j.appet.2020.104853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rukundo P.M., Andreassen B.A., Kikafunda J., Rukooko B., Oshaug A., Iversen P.O. b. Household food insecurity and diet diversity after the major 2010 landslide disaster in Eastern Uganda: a cross-sectional survey. British Journal of Nutrition. 2016;115(4):718–729. doi: 10.1017/S0007114515004961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rukundo P.M., Oshaug A., Andreassen B.A., Kikafunda J., Rukooko B., Iversen P.O. a. Food variety consumption and household food insecurity coping strategies after the 2010 landslide disaster–the case of Uganda. Public Health Nutrition. 2016;19(17):3197–3209. doi: 10.1017/S1368980016001397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salkovskis P.M., Rimes K.A., Warwick H.M.C., Clark D.M. The health anxiety inventory: Development and validation of scales for the measurement of health anxiety and hypochondriasis. Psychological Medicine. 2002;32(5):843–853. doi: 10.1017/s0033291702005822. [DOI] [PubMed] [Google Scholar]
- Shen W., Long L.M., Shih C.H., Ludy M.J. A humanities-based explanation for the effects of emotional eating and perceived stress on food choice motives during the COVID-19 pandemic. Nutrients. 2020;12(9):2712. doi: 10.3390/nu12092712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spoor S.T.P., Bekker M.H.J., Van Strien T., Van Heck G.L. Relations between negative affect, coping, and emotional eating. Appetite. 2007;48(3):368–376. doi: 10.1016/j.appet.2006.10.005. [DOI] [PubMed] [Google Scholar]
- Stinson E.J., Votruba S.B., Venti C., Perez M., Krakoff J., Gluck M.E. Food insecurity is associated with maladaptive eating behaviors and objectively measured overeating. Obesity. 2018;26(12):1841–1848. doi: 10.1002/oby.22305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stunkard A.J., Messick S. The three-factor eating questionnaire to measure dietary restraint, disinhibition and hunger. Journal of Psychosomatic Research. 1985;29:71–83. doi: 10.1016/0022-3999(85)90010-8. [DOI] [PubMed] [Google Scholar]
- Thayer R.E., Newman J.R., McClain T.M. Self-regulation of mood: Strategies of changing a bad mood, raising energy and redirecting tension. Journal of Personality and Social Psychology. 1994;67(5):910–925. doi: 10.1037//0022-3514.67.5.910. [DOI] [PubMed] [Google Scholar]
- Touyz S., Lacey H., Hay P. Eating disorders in the time of COVID-19. J Eat Disord. 2020;8:19. doi: 10.1186/s40337-020-00295-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner-McGrievy G., Karami A., Monroe C., Brandt H.M. Dietary pattern recognition on twitter: A case example of before, during, and after four natural disasters. Natural Hazards: Journal of the International Society for the Prevention and Mitigation of Natural Hazards. 2020:1–15. doi: 10.1007/s11069-020-04024-6. [DOI] [Google Scholar]
- Van Rheenen T.E., Meyer D., Neill E., Phillipou A., Tan E.J., Toh W.L., et al. Mental health status of individuals with a mood-disorder during the COVID-19 pandemic in Australia: Initial results from the COLLATE project: COVID-19 and mood disorders. Journal of Affective Disorders. 2020;275:69–77. doi: 10.1016/j.jad.2020.06.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Strien T., Van de Laar F.A., Van Leeuwe J.F.J., Lucassen P.L.B.J., Van den Hoogen H.J.M., Rutten G.E.H.M. The dieting dilemma in patients with newly diagnosed type 2 diabetes: Does dietary restraint predict weight gain 4 years after diagnosis? Health Psychology. 2007;26:105–112. doi: 10.1037/0278-6133.26.1.105. [DOI] [PubMed] [Google Scholar]
- Van den Tol A.J.M., Coulthard H., Hanser W.A. Music listening as a potential aid in reducing emotional eating: An exploratory study. Musicae Scientiae. 2018 doi: 10.1177/1029864918780186. [DOI] [Google Scholar]
- van Strien T, Cebolla A, Etchemendy E, Gutiérrez-Maldonado J, Ferrer-García M, Botella C, Baños R. Emotional eating and food intake after sadness and joy. Appetite. 2013;66 doi: 10.1016/j.appet.2013.02.016. [DOI] [PubMed] [Google Scholar]
- Wang A.W.T., Cheng C.P., Chang C.S., Chen D.R., Chen S.T., Shieh V., et al. Does the factor structure of the brief cope fit different types of traumatic events? A test of measurement invariance. European Journal of Psychological Assessment. 2018;34(3):162–173. doi: 10.1027/1015-5759/a000321. [DOI] [Google Scholar]
- Williams L., Regagliolo A., Rasmussen S. Predicting psychological responses to Influenza A, H1N1 (“Swine flu”): The role of illness perceptions. Psychology Health & Medicine. 2012;17(4):383–391. doi: 10.1080/13548506.2011.626564. [DOI] [PubMed] [Google Scholar]
- World Health Organisation Covid timeline. 2020. https://www.who.int/news-room/detail/29-06-2020-covidtimeline Retrieved on 01/07/2020 from.
- Woodhouse S, Hebbard G, Knowles S.R. Exploring symptom severity, illness perceptions, coping styles, and well-being in gastroparesis patients using the common sense model. Digestive Diseases and Sciences. 2018;63(4):958–965. doi: 10.1007/s10620-018-4975-x. [DOI] [PubMed] [Google Scholar]
- Xu X., Bai R., Bing L., Rao Y., Liu L., Reis C., Zhao Y. Food guide pagoda and the food safety of women: One-year follow-up study on the effects of the 2008 sichuan earthquake. Asia Pacific Journal of Clinical Nutrition. 2018;27(3):662. doi: 10.6133/apjcn.092017.08. [DOI] [PubMed] [Google Scholar]
- Yeung N.C., Lau J.T., Choi K.C., Griffiths S. Population responses during the pandemic phase of the influenza A (H1N1) pdm09 Epidemic, Hong Kong, China. Emerging Infectious Diseases. 2017;23(5):813. doi: 10.3201/eid2305.160768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yusoff N., Low W.Y., Yip C.H. Reliability and validity of the brief COPE scale (English version) among women with breast cancer undergoing treatment of adjuvant chemotherapy: A Malaysian study. Medical Journal of Malaysia. 2010;65(1):41–44. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.