Abstract
Summary: Loss of air pressure resistance leads to a high rate (25.7%) of inaccurate needle-tip placement in the posterior soft tissues of the back during lumbar epidural steroid administration employing a 20-gauge Tuohy needle. Imaging and epidurogram are essential for confident identification of the lumbar epidural space to enable accurate location of steroid administration. Studies assessing efficacy of lumbar epidural steroid injection and individual patient treatments should ensure location of administration with epidurogram to enhance the validity of results.
Lumbar epidural steroid injection (LESI) is commonly used as a supplemental treatment in the conservative management of lower back pain and lumbar radiculopathy. Radiologists who practice pain management typically use image guidance such as fluoroscopy or CT in performing LESI, but this procedure is most commonly performed without the assistance of imaging techniques by using the so-called loss of resistance technique (1). Prior studies evaluating treatment success of the LESI procedure have voiced concern regarding the accuracy of needle-tip positioning and location of medication delivery (2, 3). These studies suggest that inappropriate needle position may occur in as many as 30% of lumbar epidural injection procedures performed with either sacral hiatus or lumbar puncture approach and could affect treatment outcome. Treatment success and outcome assessment in various studies could differ.
The purpose of this study was to evaluate the need for imaging assistance during lumbar epidural steroid injection by establishing the incidence of inaccurate extracanal needle placement with the loss of air pressure resistance technique.
Description of Technique
A single senior experienced neuroradiologist (W.S.B.) routinely performed LESI by using loss of air pressure resistance in combination with fluoroscopy to confirm location of needle-tip position in all patients. LESI procedures performed by this operator were retrospectively reviewed, and the incidence and characteristics of inaccurate position of the needle tip outside the spinal canal was assessed. Institutional review board approval was obtained for this retrospective data evaluation.
Over a 10-month period, this operator performed 74 consecutive LESI procedures on 55 patients. C-arm fluoroscopy was used in all cases with anteroposterior and lateral positional capability (OEC series 9800, General Electric, Milwaukee, WI).
Patients typically presented with back pain or lumbar radiculopathy. Twenty-five patients were male and 30 were female (age range, 20–83 years; mean age, 56.6 years). In 24 procedures, LESI was combined with other treatment (nerve root block, facet injection). In 50 procedures, only LESI was performed.
LESI was always performed at non-operative levels only, and the patients’ CT or MR imaging studies were typically available and evaluated before the LESI. Level choice was made closest to the maximum degenerative changes noted and location of the patients back pain considering the largest accessible posterior lumbar epidural space. Lumbar levels injected included L1–2 (11), L2–3 (17), L3–4 (39) and L4–5 (7) procedures.
LESI Technique
After the back was cleansed, the interlaminar trajectory to the midline posterior lumbar epidural space was determined in the anteroposterior projection with minor tube angulation and minimal obliquity and local anesthetic was applied. A 20-gauge Tuohy needle was inserted into the soft tissues of the back to a typical depth of approximately 3–4 cm and connected via a short (6 cm, 0.5 cc) low-volume extension tube (Baxter, Deerfield, IL) to a standard 3 cc plastic syringe filled with 1.5 cc air and nonionic contrast (Iohexol, 240 mgI/cc; Amersham Health, Oslo, Norway).
Initial needle depth was assessed with lateral fluoroscopy, after which the anteroposterior fluoroscopic position was reestablished and the needle was progressively advanced toward the lumbar epidural space. The 3-mL syringe was turned upward, and intermittent testing with air in the air/contrast syringe was performed to assess positioning within the back soft tissues. Intermittent fluoroscopic assessment in the minimally oblique anteroposterior projection was again employed to guide the needle tip between the medial aspect of the lamina and direct ultimate positioning to the posterior lumbar canal and epidural space.
When pressure resistance in the syringe was lost, lateral fluoroscopy was reestablished and needle-tip position was assessed with a small nonionic contrast medium injection and a fluoroscopic image obtained to determine exact needle-tip location.
If the needle tip remained outside the spinal canal epidural space as noted by tip position and contrast distribution, the needle was advanced with anteroposterior fluoroscopic assistance and resumed intermittent air pressure resistance until the epidural space was appropriately entered. Confirmation of correct needle-tip position was made with a 1.5-mL nonionic contrast medium injection, and anteroposterior and lateral epidurogram was inspected and recorded.
Study Design
The 74 LESI procedures were retrospectively reviewed, and the incidence and characteristics of inaccurate position of the needle tip outside the spinal canal were assessed and tabulated. The results are summarized in Table 1.
TABLE 1:
LESI procedures and initial needle tip position with loss of resistance as seen in the lateral projection
| Initial Needle Tip Position | # LESI Procedures | % | Adjacent to Spinal Canal | Mid Spinous Process |
|---|---|---|---|---|
| Extracanal position | 19 | 26 | 15 | 4 |
| Epidural position | 55 | 74 | ||
| Total | 74 | 100 | 15 (20.3%) | 4 (5.4%) |
In 19 of 74 (25.7%) LESI procedures, resistance to intermittent pressure was lost during needle insertion while the needle-tip position was still within the back soft tissues and not in the posterior lumbar epidural space. In 15 of these 19 procedures (79%), needle-tip position was overlying the facet and posterior lamina at the base of the spinous process, likely just posterior to the ligamentum flavum (Fig 1A, –B). Confident position relative to the lumbar canal was difficult to judge in these cases by fluoroscopy alone. Contrast medium injection confirmed position external to the lumbar canal and outside the lumbar epidural space. In four of the 19 procedures (21%), the needle tip was still several centimeters from the correct epidural position when loss of air pressure resistance occurred overlying the midportion of the spinous process (Fig 2).
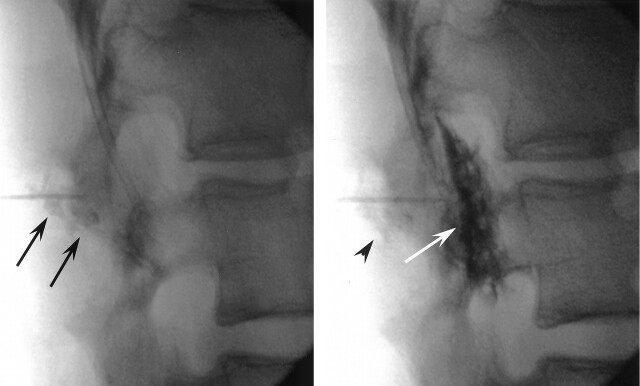
Fig 1.
Lateral fluoroscopic images of a 52-year-old man with back pain and leg pain during LESI procedure.
A, Contrast medium injected at loss of resistance is seen overlying the deep paraspinal region just posterior to the ligamentum flavum and spinal canal (arrows).
B, The needle was advanced and the epidural space is correctly engaged and the correct needle-tip location is confirmed with epidurogram (white arrow). Initial injection is also visible (black arrowhead).
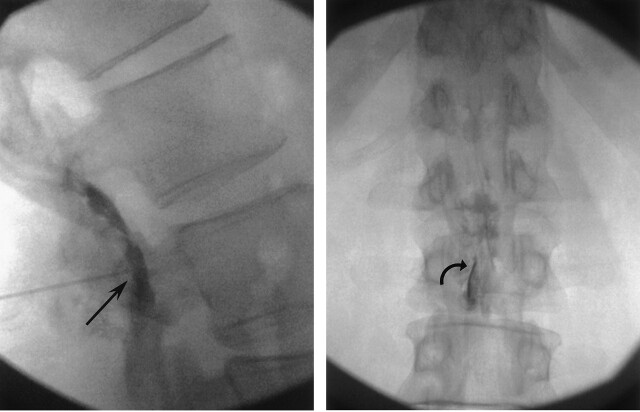
Fig 2.
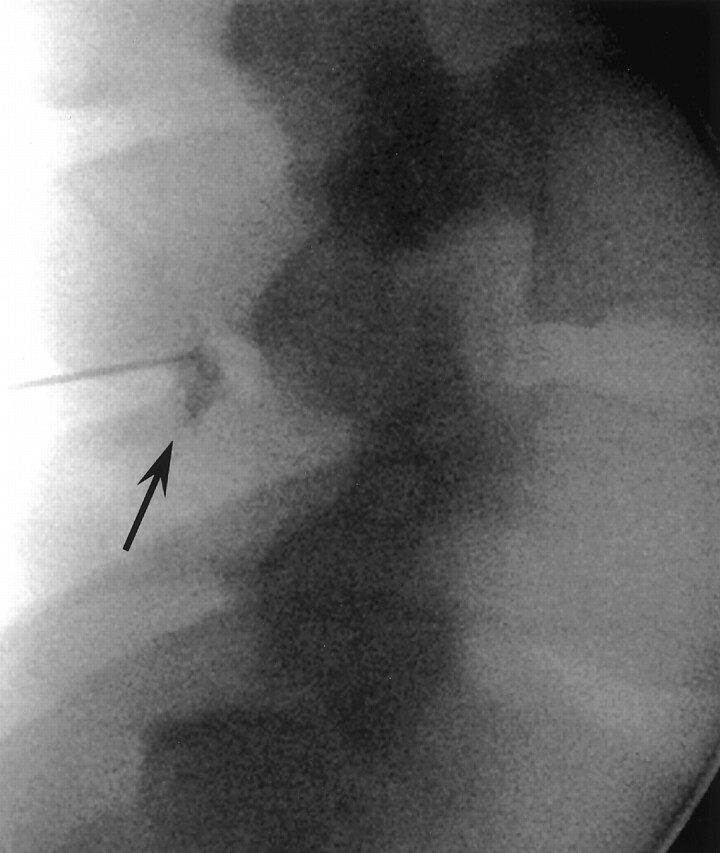
Lateral fluoroscopic images of a 23-year-old man with back pain during LESI procedure. Contrast medium injected at point of loss of resistance is seen overlying the spinous process still within the midback soft tissues (arrow). The needle tip was subsequently advanced to the posterior epidural space and confirmed with epidurogram.
In all of these procedures, after initial loss of pressure resistance, air was added to the syringe, and the needle tip was progressively advanced with fluoroscopy and air pressure resistance assessment until the lumbar epidural space was correctly entered and confirmed with contrast medium injection and epidurogram.
In 55 of 74 LESI procedures (74.3%), air pressure resistance was first lost upon appropriately entering the lumbar posterior epidural space. Confirmation of tip position was made with nonionic contrast medium injection and anteroposterior and lateral epidurogram and correct position was clearly recognized in these patients (Fig 3 A and B).
Fig 3.
A and B, Lateral and anteroposterior fluoroscopic images of a 56 year-old-man with back and leg pain during LESI procedure demonstrates proper position of the needle tip after initial loss of resistance in the posterior epidural space in the lateral (arrow) and anteroposterior (curved arrow) projections.
In all instances, the epidural space was successfully entered. No complications were encountered in these 74 procedures, and the subarachnoid space was never engaged.
Discussion
Most LESI procedures are performed blind by physicians in an office practice without fluoroscopy rather than by radiologists. Injection of air via a well-lubricated syringe is commonly used as a method to test needle-tip position during LESI, because the ligamentous and muscular soft tissues of the back usually present resistance to injection. When loss of resistance to air injection is noted, it is assumed that the posterior epidural space has been engaged and injection can proceed.
Early studies evaluating LESI warned that the loss of resistance technique could be a false indicator of needle-tip position (3). White et al (3) suggested that needle-tip position was inaccurate in 25% of caudal and 30% of lumbar epidural injections by using the air injection technique. They clearly recognized that loss of air pressure resistance, while simple and helpful, was not intrinsically reliable. Lateral fluoroscopy can help with needle placement, but the exact position of the needle tip may still be in doubt.
Other authors support the loss of resistance technique without fluoroscopic confirmation (4–6). Fredman et al (4), evaluating epidural “catheter” placement in the lumbar canal in patients with prior lumbar surgery, employed an 18-gauge Tuohy needle and encountered significant problems in engaging the posterior epidural space in six of 50 (12%) procedures by using the loss of air resistance technique (repetitive dural puncture: three patients; paraspinal catheter placement: three patients). In their study, six of 50 patients required multiple punctures in an attempt to locate the posterior epidural space. It was suggested that fluoroscopy alone was inadequate to determine needle-tip position in their patients and epidurogram was essentially necessary to confirm the final placement of the catheter and ultimate dispersion of contrast and steroid (4).
McNeill and Thornburn (5), evaluating epidural catheter placement by using 16- or 18-gauge Tuohy needles and loss of resistance technique, encountered placement difficulties in 25% of procedures with difficulty (12.7%) or failed (3.5%) catheter insertion in 16.2% and vein canulation in 8%. These studies suggest that correct positioning can be a challenge even by using larger gauge systems with the advantage of more stable direction control and sensitivity to air resistance.
Liu et al (6) report an 8% incidence of incorrect needle placement by using a 20-gauge Tuohy needle and loss of resistance to saline injection during needle insertion. They report a sensitivity of 99% and positive predictive value of 92% but a specificity and negative predictive value of only 27% and 75%, respectively (6). It was concluded that fluoroscopy might be necessary to ensure correct needle-tip positioning (6).
Sharrock et al (7) reports epidural anesthesia delivered by 17-gauge Tuohy needle and either midline or paramedian approach, failure (defined by inability to locate the epidural space, dural puncture, or failed anesthetic) in only 1.3% of procedures but suggests that the large dose of local anesthetic (15–25 mL) used could have played a role in the success rate. They report a higher rate of failure (8.8%) in patients with prior spine surgery although the level of anesthetic delivery relative to surgical site was not addressed.
In a study evaluating the success of LESI in sciatica, Loy supplemented the typical loss of air resistance technique with the injection of excess air and a saline-wetted 18-gauge Tuohy needle hub, listening for a characteristic “whistle” when free backflow was identified (8). Although his patients were not studied with contrast and epidurogram for tip confirmation, he concluded that his epidural needle position was accurate.
Our data are more consistent with the report of White et al (3) and more strongly supports inaccuracy of the loss of resistance technique. In 25.7% of LESI procedures, loss of air pressure resistance was encountered while the needle tip was outside the spinal canal in the posterior back soft tissues. In 15 of 74 procedures (20.3%), the needle tip was positioned at the base of the spinous process or overlying the facets, just posterior to the ligamentum flavum. Injection of contrast confirmed that the lumbar epidural space was not correctly engaged for proper placement of the steroid treatment. This was the suspected location of incorrect positioning suggested by White et al (3).
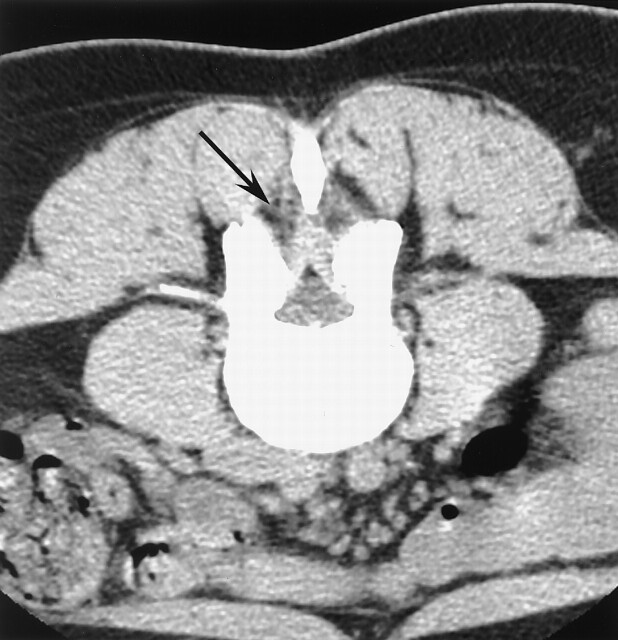
The probable cause of inaccuracy of the loss of air resistance technique is injection while the needle tip is positioned within the fat overlying the ligamentum flavum (Fig 4). This posterior paraspinal fat likely presents the perception of similar intrinsic resistance to injection as epidural fat, leading to a false sense of low resistance to air or contrast medium injection. Midline and slightly paramedian approaches can be affected in a similar fashion. Needle-tip deflection has been demonstrated with spinal needles and is more severe with beveled or epidural delivery systems (9). In an in vitro study, Kopacz and Allen (9) demonstrated that Tuohy needles incurred deflection of 1.42–2.05 mm when a 22-gauge system was used and 2.62–3.55 mm when an 18-gauge system was used during 5 cm penetration through porcine muscle or synthetic test material. This problem of needle-tip deflection is well known to those of us who perform spine procedures with typical beveled or Tuohy needles (10).
Fig 4.
Prone CT image in a 36-year-old woman with radiculopathy undergoing epidural steroid injection with CT guidance demonstrates extensive fat in the posterior paraspinal soft tissues adjacent to the ligamentum flavum (arrow).
Simple lateral fluoroscopic assessment of needle-tip position was inadequate to determine tip location in these cases. Overlying facet hypertrophy and sclerosis made tip position uncertain, and the oblique angle of the lamina and ligamentum flavum further confounds tip location. Often the difference between extracanal needle-tip position and correct epidural tip location is small. These problems reinforce the need for contrast identification of needle-tip location by fluoroscopic epidurogram (2, 10–12). The combined frontal and lateral projections used here confirm tip position in the posterior epidural space. In addition, distribution of contrast with the epidurogram and diffusion of the epidural contrast with steroid administration can be helpful in assessing the ultimate distribution of the steroid in the spinal canal. This distribution could play a role in ultimate procedure outcome. CT guidance for needle placement is an equally valid imaging approach for confirmation of needle-tip location.
In four of 74 procedures (5.4%), pressure resistance was lost while the needle tip was overlying the midspinous process. This suggests that other areas of paraspinal fat can present the same intrinsic low resistance to pressure as occurs outside the spinal canal.
Although LESI is commonly used to supplement conservative management of lower back pain and lumbar radiculopathy, study outcomes of this procedure remain controversial (13–16). Accuracy of steroid placement is crucial in establishing treatment efficacy of the LESI procedure. Studies evaluating the use of LESI often fail to detail the route of administration or confirm location of medication delivery.
Conclusion
Simple loss of air pressure resistance is an inadequate method of establishing needle-tip positioning in the posterior epidural space. Incorrect needle-tip position occurred in 25.7% of LESI procedures when using the loss of resistance technique and a relatively large 20-gauge Tuohy needle. Fluoroscopy and contrast medium injection with epidurogram were essential to identify incorrect needle-tip location and confirm epidural position when the lumbar canal was correctly engaged.
References
- 1.Waldman SD. Lumbar epidural nerve block. In: Waldman SD. Atlas of Interventional Pain Management. Philadelphia: Saunders;1998. :308–317
- 2.Johnson BA, Shellhas KP, Pollei SR. Epidurography and therapeutic epidural injections: technical considerations and experience with 5334 cases. AJNR Am J Neuroradiol 1999;20:697–705 [PMC free article] [PubMed] [Google Scholar]
- 3.White AH, Derby R, Wynne G. Epidural injections for the diagnosis and treatment of low-back pain. Spine 1980;5:78–86 [DOI] [PubMed] [Google Scholar]
- 4.Fredman B, Nun MB, Zohar E, et al. Epidural steroids for treating “failed back surgery syndrome”: fluoroscopy really necessary? Anesth Analg 1999;88:367–372 [PubMed] [Google Scholar]
- 5.McNeill MJ, Thornburn J. Cannulation of the epidural space. A comparison of 18- and 16-gauge needles. Anaesthesia 1988;43:154–155 [PubMed] [Google Scholar]
- 6.Liu SS, Melmed AP, Klos JW, Innis CA. Prospective experience with a 20-gauge Tuohy needle for lumbar epidural steroid injections: is confirmation with fluoroscopy necessary? Reg Anesth Pain Med 2001;26:143–146 [DOI] [PubMed] [Google Scholar]
- 7.Sharrock NE, Urquhart B, Mineo R. Extradural anaesthesia in patients with previous lumbar surgery. Br J Anaesth 1990;65:237–239 [DOI] [PubMed] [Google Scholar]
- 8.Loy TTT. Epidural steroid injection for sciatica: an analysis of 526 consecutive cases with measurements and the whistle test. J Orth Surg 2000;8:39–44 [DOI] [PubMed] [Google Scholar]
- 9.Kopacz DJ, Allen HW. Comparison of needle deviation during regional anesthetic techniques in a laboratory model. Anesth Analg 1995;81:630–633 [DOI] [PubMed] [Google Scholar]
- 10.Sitzman TB. Epidural injections. In: Fenton DS, Czervionke LF, eds. Image-Guided Spine Intervention. Philadelphia: Saunders;2003. :99–126
- 11.El-Khoury, Ehara S, Weinstein JN, et al. Epidural steroid injection: a procedure ideally performed with fluoroscopic control. Radiology 1988;168:554–557 [DOI] [PubMed] [Google Scholar]
- 12.Renfrew DL, Moore TE, Kathol MH, et al. Correct placement of epidural steroid injections: fluoroscopic guidance and contrast administration. AJNR Am J Neuroradiol 1991;12:1003–1007 [PMC free article] [PubMed] [Google Scholar]
- 13.Carette S, Leclaire R, Marcoux S, et al. Epidural corticosteroid injection for sciatica due to herniated nucleus pulposus. N Engl J Med 1997;336:1634–1640 [DOI] [PubMed] [Google Scholar]
- 14.Bush K, Hiller S. A controlled study of caudal epidural injections of triamcinolone plus procaine for the management of intractable sciatica. Spine 1991;16:572–575 [DOI] [PubMed] [Google Scholar]
- 15.Bowman SJ, Wedderburn L, Whaley A, et al. Outcome assessment after epidural cortical steroid injection for low back pain and sciatica. Spine 1993;18:1345–1350 [DOI] [PubMed] [Google Scholar]
- 16.Fukusaki M, Kobayashi I, Tetsuya H, Sumikawa K. Symptoms of spinal stenosis do not improve after epidural steroid injection. Clin J Pain 1998;14:148–151 [DOI] [PubMed] [Google Scholar]