Abstract
Summary: Simple bone cysts are common, benign, fluid-filled, cystic lesions that occur mostly in the metaphysis of the long bones and are rarely found in vertebrae. A case of a simple bone cyst in the spinous process of the fourth cervical vertebra in a 26-year-old woman is reported. According to the radiologic findings, the lesion was identified as a simple bone cyst, and the diagnosis was verified by surgical and histopathologic examinations.
Although Bloodgood first recognized simple bone cysts as a distinct disease entity in 1910, Jaffe and Lichtenstein (1) were the first to provide a detailed description of the simple vertebral bone cyst in 1942. Simple bone cysts are common, benign, fluid-filled, cystic lesions that cause minimal expansion of the bone and usually occur in the metaphysis of long bones. To date, 10 cases of simple bone cysts have been reported in the literature (2), and those bone cysts involved vertebral bodies (three), spinous process (three), lamina (one), pedicle (one), both spinous processes and lamina (one), and all components of the vertebrae (one) (2–6). To our knowledge, only four were in cervical vertebrae (3–6), and the rest were in lumbar vertebrae (2, 4). We present a simple bone cyst involving the C4 vertebra of a 26-year-old female patient. We discuss the radiologic differential diagnosis of simple vertebral bone cysts, and the surgical and histopathologic verifications of the diagnosis are presented.
Case Report
An otherwise healthy 26-year-old female patient presented with a 1-year history of neck pain radiating to both upper extremities. No neurologic deficits or abnormal values were noted on physical examination or in laboratory data. The patient was suspected of having degenerative disk disease, so she was referred to our radiology department for examination.
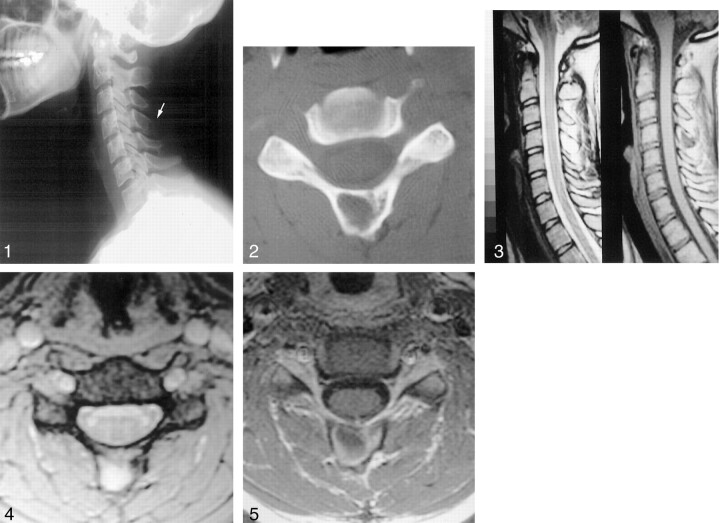
The lateral view of radiographs of the cervical vertebrae demonstrated a faintly visible osteolytic lesion causing minimum expansion in the C4 vertebral spinous process (Fig 1). CT (Fig 2) of the cervical spine showed the expansile unilocular cystic lesion of the spinous process at C4 and cortical thinning of the bone. Cervical MR images showed a unilocular homogeneous cyst having regular contours and measuring 10 × 8 mm in the spinous process of C4 vertebra (Fig 3). The lesion appeared homogeneous and hyperintense on axial T2*-weighted images, and no blood degradation products were observed (Fig 4). No enhancement was observed on T1-weighted images following contrast medium administration (Fig 5). When all of the radiologic findings were assessed, we concluded that the lesion had the characteristic radiologic appearance of a simple bone cyst.
Fig 1.
Lateral radiograph of the cervical vertebrae. There is a minimally expansile lesion of the spinous process of C4 vertebra (arrow).
Fig 2.
Axial nonenhanced CT scan with bone window of the fourth cervical vertebra. Note the thinning of the cortical bone.
Fig 3.
Sagittal T2-weighted and T1-weighted MR images of cervical vertebrae show the spinous process, unilocular, and homogeneous cystic lesion of the fourth cervical vertebra.
Fig 4.
Axial T2*-weighted MR image of the fourth cervical vertebra shows homogeneous and hyperintense appearance of the lesion. Note the lack of blood degradation products.
Fig 5.
Axial postcontrast T1-weighted MR image demonstrates similar signal intensity characteristics as those of precontrast T1-weighted images (not shown) that define nonenhancing lesions.
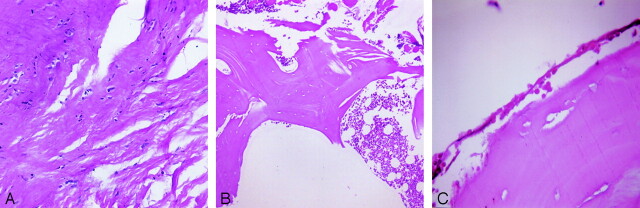
The patient underwent surgery to remove the suspected simple bone cyst in the C4 vertebra. On opening, a lesion containing fluid involving the spinous process was seen. There was little bleeding. The spinous process and the lesion within were removed. The specimen was sent for pathologic examination. Microscopic examination revealed mature fat cells, muscle fibers, and connective tissue fragments of the tendons that showed chondroid metaplastic foci (Fig 6A). In addition, predominantly mature compact bone and focal spongious bone fragments containing bone marrow elements were seen (Fig 6B). The cyst had a thin wall and was lined by flat epithelial cells with a mesothelial appearance (Fig 6C). There were no blood cells in its cavity and the characteristic morphology of an aneurysmal bone cyst in its wall was absent.
Fig 6.
Results of histopathologic examination
A, Chondroid metaplastic foci in the connective tissue surrounding the lesion (hematoxylin-eosin stain ×100).
B, Lamellar and spongy bone fragments containing bone marrow elements (hematoxylin-eosin stain ×40).
C, Mesothelium-like flat endothelial cells line the wall of the simple bone cyst (hematoxylin eosin stain ×400).
Discussion
The differential diagnosis of an expansile cystic lesion involving the posterior elements of vertebrae, such as spinous processes in children or young adults, should include aneurysmal bone cyst, giant cell tumor, and simple bone cyst (5).
Aneurysmal bone cysts are multiloculated, expansile, highly vascular, osteolytic lesions that are filled with free-flowing blood products with fluid levels. They are common in patients younger than 30 years, with a slight female predominance. They may occur in all parts of the skeleton and particularly involve the metaphysis of long bones (5, 7) but occasionally involve spine, especially cervical and thoracic regions. When aneurysmal bone cysts are found in vertebrae, they typically occur in the posterior elements, including the transverse process, spinous process, lamina, and neural arches. Often, however, they expand secondarily into the pedicles and vertebral body (7). Roentgenographic and CT views indicate an osteolytic lesion that results in an expansion and thinning of the surrounding cortical bone. A soft tissue mass is often present. Aneurysmal bone cysts are typically characterized by their lobulated and multiseptated appearance with fluid-fluid levels and blood degradation products on MR images. The radiologic appearance of the lesion of our patient was not multiloculated and did not have fluid-fluid levels, blood degradation products, or soft tissue around the lesion.
Giant cell tumors are expansile, lytic, locally aggressive, primary benign bone tumors with thinning of the cortex. Most patients are between 20 and 40 years old. Giant cell tumors have been described at the ends of long bones, characteristically around the knee. Giant cell tumors of the spine only accounts for 3–7% of primary bone tumors. In the spine, the most typical site of localization is the sacrum; other vertebral segments are rarely involved (7). Radiographs and nonenhanced CT images show lytic lesions producing cortical thinning and expansion with a destructive sacral or vertebral mass. MR images show a multiloculated mass of heterogeneous signal intensity that usually has blood products within (7). In the case of our patient, the radiologic findings were not suggestive of a giant cell tumor, because the cystic lesion was not destructive or aggressive and did not have multiple compartments or heterogeneous signal intensity and blood degradation products on MR images.
Simple bone cysts are common, benign, fluid-filled, cystic lesions that cause minimal expansion of the bone and occur mostly in the metaphysis of long bones. Those cysts predominantly occur in male patients with a ratio of 2.5:1. Most occur in children and adolescents. Simple bone cysts are found in the metaphysis of long tubular bones in 90–95% of cases, and 5–65% of such cysts involve the proximal humerus; 25–30%, the femur; and the rest, the proximal tibia, fibula, radius, ulna, ileum, patella, rib (8), and calcaneus (9).
The pathogenesis of simple bone cysts is still unknown. According to many authors, the lesions in the long bones are due to the developmental defect of the epiphyseal plate (4). Another suggestion is that venous obstruction of interstitial fluid drainage might be the cause (10). Aegerter and Kirkpatrick (11) proposed that the cause of the simple bone cysts is post-traumatic and posthemorrhagic, except the ones in the long bones. This may be the reason why simple bone cysts occur in vertebrae in an older age group than do the cysts of long bone. Moreover, our patient was 26 years old, well above the usual age for lesions in the long bones (7).
Most of the simple bone cysts are asymptomatic, unless they come with pathologic fracture. They are recognized incidentally on radiographic examinations. Any other prior symptoms are mild pain, local tenderness, and swelling (5). Although roentgenography is usually adequate to identify the simple bone cyst, CT and MR imaging should be used for diagnosis of lesions in anatomically complex locations such as the vertebrae. Hence, we used all these three imaging techniques to make a complete diagnosis. CT and MR imaging were also used to determine the extent of the lesions and detect possible complications such as fractures. Roentgenography usually shows simple bone cysts as well-defined, intramedullary, metaphyseal, and pure lytic lesions. Some of them are found in diaphysis. They may cause expansion of the bone with thinning of the overlying cortex. Simple bone cysts usually lead to fracture of the bone; therefore, some of these fractures may cause the migration of a fractured bone tissue into the cystic cavity. This rare pathognomic radiologic finding is known as “fallen fragment sign” (12). In the case of our patient, the lesion did not cause any such fracture in the bone.
Until now, to our knowledge, only 10 cases of a simple bone cyst involving the vertebrae have been reported, with four of them in the cervical vertebrae. Dawson et al (3) were the first investigators to describe a simple bone cyst developing in cervical vertebrae, and it was located in the C4 vertebra. Our case reports the fifth simple bone cyst developing in cervical vertebrae.
References
- 1.Jaffe HL, Lichtenstein L. Solitary bone cyst. Arch Surg 1942;44:1004–1025 [Google Scholar]
- 2.Ha KY, Kim YH. Simple bone cyst with pathologic lumbar pedicle fracture: a case report. Spine 2003;28:129–E131 [DOI] [PubMed] [Google Scholar]
- 3.Dawson EG, Mirra JM, Yuhl ET, et al. Solitary bone cyst of the cervical spine. Clin Orthop 1976;119:141–143 [PubMed] [Google Scholar]
- 4.Park CK, Cho KK, Lee SW, et al. Simple bone cyst of the axis. Childs Nerv Syst 1997;13:171–174 [DOI] [PubMed] [Google Scholar]
- 5.Lee CC, Wei JD, How SW. Simple bone cyst in cervical vertebral spinous process and laminae: report of a case. J Formos Med Assoc 2000;99:54–58 [PubMed] [Google Scholar]
- 6.Zenmyo M, Komiya S, Hamada T, Inoue E. A solitary bone cyst in the spinous process of the cervical spine: a case report. Spine 2000;25:641–642 [DOI] [PubMed] [Google Scholar]
- 7.Osborn AG. Tumors, cysts, and tumorlike lesions of the spine and spinal cord. In: Osborn AG, ed. Diagnostic Neuroradiology. St. Louis: Mosby; 1994. :876–918
- 8.March JI, Munk PL, Muller NL. CT of a unicameral bone cyst in a rib. Br J Radiol 1992;65:74–75 [DOI] [PubMed] [Google Scholar]
- 9.Smith SB, Shane HS. Simple bone cyst of the calcaneus: a case report and literature review. J Am Pediatr Med Assoc 1994;84:127–130 [DOI] [PubMed] [Google Scholar]
- 10.Cohen J. Etiology of simple bone cyst. J Bone Joint Surg Am 1970;52:1493–1497 [PubMed] [Google Scholar]
- 11.Aegerter EE, Kirkpatrick JA Jr. Miscellaneous diseases of the skeleton. In: Aergerter EE, Kirkpatrick JA Jr, eds. OrthopedicDiseases. 3rd ed. Philadelphia: Saunders,1968;491–500
- 12.Struhl S, Edelson C, Pritzker H, et al. Solitary (unicameral) bone cyst: the fallen fragment sign revisited. Skeletal Radiol 1989;18:261–266 [DOI] [PubMed] [Google Scholar]